Targeted vs. Non-Targeted Delivery Systems for Nucleic Acid Drugs: A Strategic Evaluation for Next-Generation Therapeutics
This article provides a comprehensive evaluation of targeted and non-targeted nucleic acid drug delivery systems for researchers and drug development professionals.
Targeted vs. Non-Targeted Delivery Systems for Nucleic Acid Drugs: A Strategic Evaluation for Next-Generation Therapeutics
Abstract
This article provides a comprehensive evaluation of targeted and non-targeted nucleic acid drug delivery systems for researchers and drug development professionals. It explores the foundational principles of nucleic acid therapeutics—including ASOs, siRNAs, and mRNA—and their delivery challenges. The content systematically compares the methodologies, applications, and optimization strategies for viral vectors, lipid nanoparticles, polymer-based systems, and ligand-conjugated platforms. By analyzing clinical validation data and comparative performance metrics, this review serves as a strategic guide for selecting and engineering delivery systems to overcome biological barriers and advance the clinical translation of nucleic acid drugs.
Nucleic Acid Therapeutics and the Imperative for Advanced Delivery
Nucleic acid drugs represent a revolutionary class of therapeutics that use engineered sequences of DNA, RNA, or synthetic analogs to treat diseases by targeting their underlying genetic causes rather than just the symptoms [1]. This category has expanded significantly beyond early concepts to include a diverse arsenal of modalities including antisense oligonucleotides (ASOs), small interfering RNAs (siRNAs), messenger RNA (mRNA), and the CRISPR-Cas gene editing system [2] [3]. Unlike traditional small molecule drugs that primarily target proteins, nucleic acid therapeutics can theoretically target any gene by leveraging the principle of complementary base pairing, making them particularly valuable for addressing previously "undruggable" targets [1]. The field has gained substantial momentum in recent years, with the global nucleic acid therapeutics market projected to grow from $6.01 billion in 2024 to $12.24 billion by 2029, representing a compound annual growth rate of 15.2% [4].
The development of these therapeutics is inseparable from major discoveries in molecular biology, from the initial conceptualization of antisense technology in 1978 to the Nobel Prize-winning discovery of RNA interference in 1998 and the more recent development of CRISPR-Cas9 gene editing technology [2]. The COVID-19 pandemic notably accelerated the field, with mRNA vaccines demonstrating the tremendous potential of nucleic acid therapeutics on a global scale [2]. This guide provides a comprehensive comparison of the major nucleic acid drug modalities, with particular focus on their applications within targeted versus non-targeted delivery system research.
Comparative Analysis of Major Nucleic Acid Drug Modalities
Fundamental Characteristics and Mechanisms
Table 1: Comparison of Key Nucleic Acid Drug Modalities
| Characteristic | ASOs | siRNAs | mRNA | CRISPR-Cas |
|---|---|---|---|---|
| Molecular Type | Single-stranded oligonucleotides (18-30 nt) [1] | Double-stranded RNA (20-25 bp) [5] | Single-stranded RNA (hundreds to thousands of nt) [5] | RNA-protein complex or mRNA + gRNA [6] |
| Primary Mechanism | RNase H1-mediated degradation or steric hindrance [1] | RNAi pathway: RISC-mediated mRNA cleavage [7] | Protein replacement: in vivo protein production [2] | Gene editing: DNA cleavage and repair [8] |
| Cellular Target | Nucleus/Cytosol [6] | Cytosol [6] | Cytosol [6] | Nucleus [6] |
| Therapeutic Effect | Transient knockdown [8] | Transient knockdown [8] | Transient expression [2] | Permanent knockout or knock-in [8] |
| Key Advantages | Multiple mechanisms; splicing modulation [1] | High specificity; multi-targeting potential [9] | Non-integrating; broad applicability [2] | Permanent correction; versatile editing [2] |
| Key Challenges | Off-target effects; delivery limitations [7] | Off-target effects; RISC saturation risk [7] | Immunogenicity; instability [2] | Off-target edits; ethical considerations [2] |
Key Differentiating Factors for Research Applications
When selecting a nucleic acid modality for research or therapeutic development, several critical factors must be considered. The choice between knockdown versus knockout is fundamental: while ASOs and siRNAs reduce gene expression (knockdown), CRISPR generates permanent genetic modifications (knockout) [8]. This makes CRISPR ideal for studying essential genes or creating stable cell lines, while RNAi methods are better suited for studying genes where complete knockout would be lethal [8].
Specificity and off-target effects represent another crucial consideration. RNAi methods, particularly siRNAs, can suffer from significant off-target effects due to partial complementarity with non-target mRNAs [8] [7]. Although CRISPR initially had sequence-specific off-target effects, advanced guide RNA design and chemically modified sgRNAs have substantially reduced these concerns, making CRISPR generally more specific than RNAi for most applications [8].
The duration of effect also varies significantly: ASOs, siRNAs, and mRNA therapeutics provide transient effects (days to weeks), making them suitable for acute conditions or vaccines [8] [2]. In contrast, CRISPR-Cas can create permanent genetic changes, offering potential one-time treatments for genetic disorders but raising safety concerns about irreversible edits [2].
Delivery Systems: Targeted vs. Non-Targeted Approaches
Delivery Challenges and Pharmacological Barriers
All nucleic acid therapeutics face significant delivery challenges that must be addressed for successful research and clinical application. As negatively charged macromolecules, nucleic acids cannot passively diffuse across cellular membranes and are highly vulnerable to degradation by nucleases in the bloodstream [6] [2]. Furthermore, they are rapidly cleared by the kidneys and can trigger immune responses [2]. Perhaps the most significant barrier is endosomal entrapment: after cellular uptake, nucleic acids often become trapped in endosomes and are subsequently degraded in lysosomes, never reaching their intended subcellular targets [6] [2].
Different nucleic acid modalities have distinct subcellular destination requirements that further complicate delivery. For instance, siRNA and mRNA function in the cytosol, while ASOs and CRISPR-Cas need to reach the nucleus to access genomic DNA or pre-mRNA [6]. These varying requirements necessitate carriers with different functional domains optimized for specific cargo types and target cells [6].
Targeted Delivery Systems
Targeted delivery systems employ specific ligands that recognize and bind to receptors on particular cell types, enabling precision targeting of therapeutic nucleic acids.
GalNAc Conjugates: N-acetylgalactosamine (GalNAc) conjugates represent one of the most successful targeted delivery approaches, specifically targeting the asialoglycoprotein receptor (ASGPR) highly expressed on hepatocytes [5]. This technology has revolutionized liver-targeted siRNA therapeutics, with advantages including low immunogenicity, improved stability, and strong specific targeting [5]. However, its application is limited primarily to liver diseases, with stronger targeting of normal hepatocytes than diseased cells potentially limiting efficacy in some hepatic disorders [5].
Antibody-Oligonucleotide Conjugates (AOCs): These conjugates utilize monoclonal antibodies that bind specifically to receptors on target cells, enabling rapid and precise delivery [5]. AOCs offer strong targeting capabilities with low toxicity but face challenges including complex pharmacokinetics, short duration of efficacy, and degradation of the monoclonal antibody after cellular internalization [5].
Peptide-Based Targeted Carriers: Sequence-defined peptide carriers can be designed with specific targeting ligands to enable cell-specific delivery [6]. These synthetic peptides offer precise control over chemical structure and functionality, allowing researchers to incorporate various functional domains including nucleic acid binding regions, endosomal escape enhancers, and tissue-specific targeting moieties [6].
Non-Targeted Delivery Systems
Non-targeted systems rely on physicochemical properties and passive accumulation mechanisms for nucleic acid delivery.
Lipid Nanoparticles (LNPs): LNPs have emerged as the leading non-viral delivery platform, particularly following their successful use in COVID-19 mRNA vaccines [2] [5]. These systems encapsulate nucleic acids within lipid bilayers, protecting them from degradation and facilitating cellular uptake through endocytosis [5]. LNPs can be modified with PEG lipids to enhance stability and circulation time, though this can sometimes lead to cytotoxicity concerns [5]. Their primary advantages include strong encapsulation efficiency, ease of preparation, and biodegradability, though they can suffer from significant off-target effects in non-liver tissues without additional targeting modifications [5].
Cationic Polymers: Cationic polymers, including sequence-defined peptides, form polyplexes with nucleic acids through electrostatic interactions [6]. Linear, dendritic, and hyperbranched poly(L)lysine (PLL) structures have been extensively studied, with branching generally beneficial for transfection efficiency though sometimes accompanied by increased cytotoxicity [6]. Incorporation of histidine residues enhances endosomal buffering and escape capacity, while cysteine residues enable disulfide cross-linking for improved polyplex stability [6].
Viral Vectors: Viral vectors, particularly adeno-associated viruses (AAVs), remain important delivery vehicles for nucleic acid therapeutics, especially for CRISPR-based therapies [5]. They offer efficient transduction and long-term expression but face challenges including immunogenicity, limited cargo capacity, and potential insertional mutagenesis concerns [6] [5].
Table 2: Comparison of Targeted vs. Non-Targeted Delivery Systems
| Delivery System | Mechanism | Advantages | Limitations | Best-Suited Applications |
|---|---|---|---|---|
| GalNAc Conjugates | ASGPR receptor-mediated endocytosis [5] | High specificity to hepatocytes; low immunogenicity; clinical validation [5] | Limited to liver targeting; potentially reduced uptake in diseased hepatocytes [5] | Liver-specific diseases (e.g., hATTR amyloidosis, hepatitis) [1] |
| Antibody-Oligonucleotide Conjugates (AOCs) | Antibody-receptor binding and internalization [5] | High specificity; adaptable to various cell types; potential for immune cell targeting [5] | Complex manufacturing; limited payload; potential immunogenicity [5] | Oncology; targeted delivery to specific cell populations [5] |
| Lipid Nanoparticles (LNPs) | Endocytosis; passive targeting [5] | Proven clinical success; adaptable to various nucleic acid types; scalable production [2] [5] | Primarily hepatic accumulation without targeting; potential cytotoxicity with PEG [5] | Vaccines; systemic delivery when broad tissue distribution is acceptable [2] |
| Cationic Polymers | Electrostatic complexation; endosomal buffering [6] | Tunable properties; potential for biodegradability; enhanced endosomal escape [6] | Variable cytotoxicity; complex structure-activity relationships [6] | Local delivery; in vitro research; customizable carrier design [6] |
| Viral Vectors (AAV) | Viral transduction; nuclear delivery [5] | High transduction efficiency; long-lasting expression; tissue-specific serotypes [5] | Immunogenicity; limited cargo capacity; pre-existing immunity [6] [5] | Gene therapy requiring sustained expression; hard-to-transfect cells [2] |
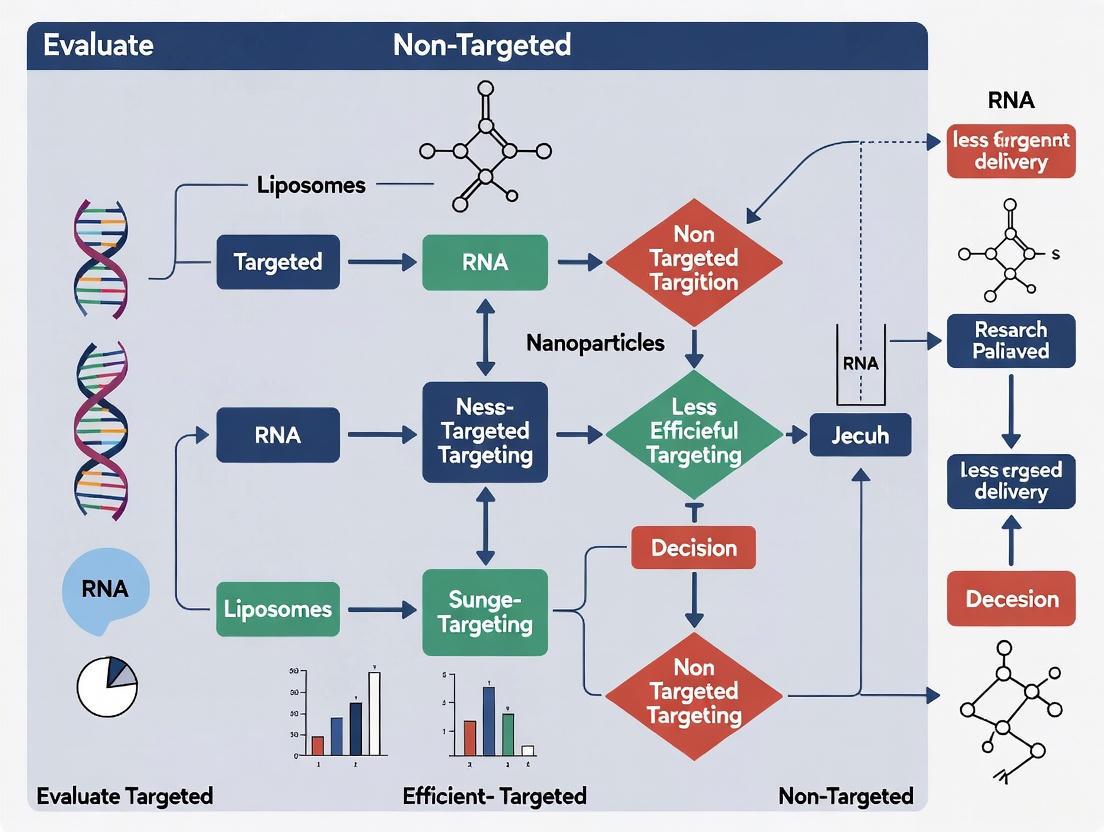
Nucleic Acid Delivery Pathways Comparison
Experimental Protocols for Delivery System Evaluation
In Vitro Assessment of Delivery Efficiency
Protocol 1: Quantitative Cellular Uptake and Internalization Analysis
Materials Required:
- Fluorescently labeled nucleic acids (e.g., Cy3-labeled siRNA, FAM-labeled ASO)
- Candidate delivery systems (LNPs, polyplexes, conjugates)
- Target cell lines with relevant receptor expression
- Flow cytometer or confocal microscopy with quantitative image analysis software
- Early endosome marker (e.g., EEA1 antibody) for subcellular localization
Methodology:
- Prepare nucleic acid-loaded delivery systems at optimal N:P ratios (for cationic carriers) or lipid:nucleic acid ratios (for LNPs) [6].
- Treat target cells with formulated complexes at predetermined concentrations (typically 10-200 nM nucleic acid concentration).
- Incubate for 2-24 hours depending on the application and internalization kinetics.
- For flow cytometry: Harvest cells, wash with cold PBS to remove surface-bound complexes, and analyze fluorescence intensity to quantify internalization [6].
- For confocal microscopy: Fix cells, stain with endosomal/lysosomal markers, and perform colocalization analysis to determine endosomal escape efficiency [6].
- Include appropriate controls: naked nucleic acids, free dye, and untreated cells.
Protocol 2: Functional Gene Silencing/Expression Efficiency
Materials Required:
- Reporter system (e.g., luciferase-expressing cells, GFP knockdown models)
- qRT-PCR equipment and reagents for target mRNA quantification
- Western blot apparatus for protein-level analysis
- Cell viability assay kits (MTT, CCK-8, or similar)
Methodology:
- Establish baseline target gene expression in chosen cell model.
- Treat cells with nucleic acid delivery systems targeting the gene of interest.
- For knockdown studies (siRNA, ASO): Incubate 48-72 hours, then harvest for mRNA and protein analysis [8].
- For expression studies (mRNA): Incubate 24-48 hours, then assess protein production via ELISA, western blot, or functional assay [2].
- For CRISPR editing: Extend incubation to 72-96 hours to allow for protein degradation and editing manifestation, then analyze editing efficiency via T7E1 assay, ICE analysis, or sequencing [8].
- Normalize results to control treatments and include appropriate positive and negative controls.
In Vivo Biodistribution and Efficacy Studies
Protocol 3: Biodistribution Analysis Using Radiolabeled or Fluorescent Probes
Materials Required:
- Nucleic acids labeled with near-infrared dyes (Cy5.5, DIR) or radionuclides (⁹⁹mTc, ¹²⁵I)
- In vivo imaging system (IVIS) or microPET/CT scanner
- Tissue homogenization equipment
- Delivery systems formulated with labeled nucleic acids
Methodology:
- Formulate delivery systems incorporating traceable nucleic acids.
- Administer to animal models via relevant route (IV, SC, etc.) at therapeutically appropriate doses.
- Perform time-course imaging at predetermined intervals (1, 4, 24, 48 hours post-injection) to track whole-body distribution [6].
- Euthanize animals at endpoint, collect and image tissues (liver, spleen, kidney, target organs).
- Quantify nucleic acid accumulation in tissues via fluorescence measurement, gamma counting, or qPCR analysis of recovered nucleic acids.
- Process tissues for histological analysis to determine cellular localization within organs.
Protocol 4: In Vivo Therapeutic Efficacy Assessment
Materials Required:
- Disease-relevant animal models (transgenic, xenograft, infection models)
- Delivery systems containing therapeutic nucleic acids
- Disease-specific biomarkers for efficacy evaluation
- Physiological monitoring equipment
Methodology:
- Randomize animals into treatment groups (n=5-8 per group minimum).
- Administer nucleic acid formulations at predetermined dosage schedules.
- Monitor disease progression through appropriate parameters (tumor volume, biomarker levels, behavioral assessments, survival).
- Collect tissues at endpoint for molecular analysis (target reduction, editing efficiency, protein expression).
- Include control groups: untreated, empty delivery system, and appropriate benchmark therapeutics.
- Perform statistical analysis to determine significance of therapeutic effects.
Research Reagent Solutions for Nucleic Acid Delivery Studies
Table 3: Essential Research Reagents for Nucleic Acid Delivery System Development
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Chemical Modification Reagents | Phosphorothioate backbone [1], 2'-O-methyl [1], 2'-fluoro [5], N-acetylgalactosamine (GalNAc) [5], Pseudouridine (Ψ) [2] | Enhance stability, reduce immunogenicity, enable targeted delivery | Balance between stability improvement and maintenance of biological activity [2] |
| Lipid Nanoparticle Components | Ionizable lipids, PEG-lipids, phospholipids, cholesterol [2] [5] | Formulate protective nucleic acid carriers for in vivo delivery | Optimize ratios for efficiency vs. cytotoxicity; PEG content affects pharmacokinetics [5] |
| Cationic Polymers | Poly(L)lysine (PLL) dendrimers [6], Histidine-Lysine (HK) peptides [6], PEI, sequence-defined carriers [6] | Nucleic acid complexation and endosomal escape enhancement | Molecular weight and branching affect efficiency and toxicity; incorporate buffering domains [6] |
| Targeting Ligands | GalNAc [5], Transferrin, Antibodies [5], Cell-penetrating peptides [6], Aptamers [1] | Cell-specific delivery for enhanced potency and reduced off-target effects | Consider receptor density, internalization efficiency, and ligand orientation [5] |
| Analytical Tools | Dynamic light scattering [10], ELISA for protein expression [2], qRT-PCR [8], NGS for off-target analysis [8] [10], Flow cytometry [6] | Characterize delivery systems and assess biological outcomes | Implement multiple orthogonal methods for comprehensive characterization [10] |
The field of nucleic acid therapeutics has evolved from theoretical concept to clinical reality, with multiple modalities now available to researchers and clinicians. Each modality—ASOs, siRNAs, mRNA, and CRISPR-Cas—offers distinct advantages and limitations, making them suited for different therapeutic applications. The critical challenge across all platforms remains efficient delivery to target tissues and cells, with both targeted and non-targeted approaches showing promise for different applications.
Looking forward, several key trends are shaping the future of nucleic acid drug development. Integration of artificial intelligence in nucleic acid design and delivery system optimization is accelerating the development process, with AI algorithms capable of predicting optimal sequences, chemical modifications, and compatible delivery systems [4] [9]. Advanced chemical modification strategies continue to emerge, enhancing stability, reducing immunogenicity, and improving the pharmacokinetic profiles of nucleic acid therapeutics [2] [1]. The expansion of delivery capabilities beyond the liver represents a critical frontier, with ongoing research focused on overcoming biological barriers to enable targeting of the central nervous system, solid tumors, and other challenging tissues [6] [10].
The growing pipeline of nucleic acid therapeutics in clinical trials—with the small nucleic acid drug market projected to reach $33.28 billion by 2034—underscores the tremendous potential of this field [9]. As delivery technologies continue to advance, nucleic acid drugs are poised to address an increasingly broad range of genetic, infectious, and chronic diseases, ultimately fulfilling their promise as a transformative modality in modern medicine.
The therapeutic potential of nucleic acid drugs (NADs), including siRNA, mRNA, and antisense oligonucleotides (ASOs), has transformed modern medicine by enabling targeted intervention at the genetic level [2]. These modalities can silence harmful genes, replace defective proteins, and potentially cure genetic disorders at their source [11] [2]. However, their clinical translation faces a fundamental trilemma: these large, negatively charged molecules must overcome * enzymatic degradation in circulation, bypass complex cellular barriers for intracellular delivery, and avoid triggering unwanted immunogenic responses*—challenges that constitute the central delivery problem in nucleic acid therapeutics [2] [12]. The resolution of this trilemma hinges on the development of sophisticated delivery systems that can navigate these interconnected obstacles while maintaining therapeutic efficacy.
The evolution of delivery platforms has progressed from viral vectors to non-viral systems, with lipid nanoparticles (LNPs) emerging as clinically validated carriers through their success in siRNA therapeutics and mRNA vaccines [13] [14]. These systems represent two philosophical approaches: targeted delivery systems designed for precise cellular recognition through surface ligands, and non-targeted systems that rely on passive accumulation and intrinsic cellular uptake mechanisms. This review systematically compares these approaches through the lens of overcoming the three central delivery challenges, providing researchers with experimental data and methodological frameworks for evaluating next-generation delivery platforms.
Quantitative Analysis of Delivery Barriers
Enzymatic Degradation Susceptibility
Nucleic acid therapeutics face immediate vulnerability to nucleases upon administration, necessitating protective formulations. The comparative stability data reveals significant differences between naked nucleic acids and those complexed within delivery systems.
Table 1: Comparative Stability of Nucleic Acid Formulations
| Formulation Type | Half-Life in Serum | Protection Mechanism | Key Stabilizing Features |
|---|---|---|---|
| Naked siRNA | <5 minutes [12] | None | Unmodified phosphodiester backbone |
| Naked mRNA | ~Minutes [14] | None | Susceptible to ribonucleases |
| Chitosan Polyplexes | Hours [12] | Polyelectrolyte complexation | Cationic amine groups form stable complexes |
| Standard LNPs | >24 hours [14] | Encapsulation in lipid bilayer | Ionizable lipid encapsulation protects payload |
| GalNAc-siRNA Conjugates | Enhanced stability [13] | Chemical modification + ligand targeting | Sugar moiety shields from nucleases |
Chemical modifications represent the first line of defense against enzymatic degradation. Early NADs like fomivirsen incorporated phosphorothioate backbones that resist nuclease cleavage, establishing a foundation for later innovations [13]. Contemporary approaches combine structural modifications with encapsulation strategies. In LNP systems, ionizable lipids with pKa values optimized for endosomal escape (typically pH 6.0-6.5) also provide a protective hydrophobic environment that shields nucleic acids from serum nucleases during circulation [15] [14]. Chitosan polyplexes leverage dense cationic charge to form stable complexes that physically block enzyme access through electrostatic interactions and hydrogen bonding [12].
Cellular Uptake Efficiency and Intracellular Trafficking
Cellular internalization represents a critical bottleneck, with significant differences observed between targeted and non-targeted systems. Quantitative microscopy studies reveal that only a fraction of internalized nanoparticles successfully mediate cytosolic delivery.
Table 2: Cellular Uptake and Endosomal Escape Efficiency
| Delivery System | Cellular Uptake Efficiency | Endosomal Escape Rate | Key Measurement Technique |
|---|---|---|---|
| Non-targeted LNPs | High in hepatocytes (ApoE-mediated) [14] | ~1-4% of internalized RNA [15] | Galectin-9 recruitment assays [15] |
| Ligand-targeted LNPs | Enhanced in specific cell types [16] | Varies with targeting moiety | Fluorescence co-localization microscopy |
| GalNAc-siRNA Conjugates | >60% in hepatocytes [13] | ASGPR-mediated efficient release | Receptor binding/internalization assays |
| Chitosan Polyplexes | Moderate (charge-dependent) [12] | pH-dependent (varies with chitosan DDA%) | Endosomal dye release assays |
Super-resolution microscopy of LNP trafficking has identified multiple distinct inefficiencies in the cytosolic delivery pathway [15]. Live-cell imaging demonstrates that both siRNA and mRNA LNPs trigger galectin-9 recruitment to damaged endosomes, with only 67-74% of damaged vesicles containing detectable siRNA cargo and approximately 20% containing mRNA cargo [15]. This suggests significant payload segregation during endosomal sorting. Furthermore, only a small fraction of the nucleic acid cargo contained within damaged endosomes is actually released to the cytosol, creating a compound inefficiency where only a minority of internalized LNPs both damage endosomes and release their payload [15] [17].
Targeted systems like GalNAc-siRNA conjugates bypass these inefficiencies through receptor-mediated uptake, achieving significantly higher functional delivery rates to hepatocytes by leveraging the asialoglycoprotein receptor (ASGPR) [13]. Similarly, ligand-conjugated chitosan polyplexes functionalized with folate, transferrin, or RGD peptides demonstrate enhanced cellular uptake through specific receptor interactions compared to their non-targeted counterparts [12].
Immunogenicity Profiles
The immunostimulatory potential of NADs varies significantly by formulation, with recognition by pattern recognition receptors (PRRs) triggering potentially therapeutic or adverse immune activation.
Table 3: Immunogenicity Profile Comparison
| Delivery System | Immune Activation Pathway | Strategies for Mitigation | Clinical Implications |
|---|---|---|---|
| Unmodified mRNA | TLR7/8, RIG-I, PKR recognition [2] | Nucleoside modifications (pseudouridine) [2] | Enhanced vaccine responses, undesirable for protein replacement |
| LNP-mRNA | Minor innate immune activation [14] | Purification to remove dsRNA contaminants | Generally favorable safety profile in vaccines |
| Chitosan Polyplexes | Varies with degree of deacetylation [12] | Chemical modification to reduce cationic charge density | Can be tuned for adjuvant or stealth properties |
| GalNAc-siRNA | Minimal immune activation [13] | Extensive chemical modification of siRNA backbone | Suitable for chronic administration |
The immunogenicity landscape reveals a delicate balance—while excessive immune activation can cause adverse effects and reduce therapeutic efficacy, controlled immune stimulation may be desirable for vaccine applications. The success of mRNA vaccines against COVID-19 demonstrated how nucleoside modifications (pseudouridine) combined with LNP delivery could achieve the optimal balance: sufficient innate immune sensing to generate robust adaptive immunity without excessive reactogenicity [2]. For non-vaccine applications, advanced LNP systems incorporate PEGylated lipids and optimized ionizable lipids that minimize immune recognition, while chitosan formulations can be chemically modified to reduce their inherent immunostimulatory properties [12] [14].
Experimental Approaches for Barrier Analysis
Methodologies for Assessing Enzymatic Stability
Protocol 1: Serum Stability Assay
- Preparation: Formulate nucleic acids with candidate delivery systems (LNPs, polyplexes) and label with appropriate fluorophores (e.g., Cy5, AF647).
- Incubation: Expose formulations to 50-90% human or fetal bovine serum at 37°C.
- Sampling: Remove aliquots at predetermined time points (0, 15, 30, 60, 120, 240, 480 minutes).
- Analysis: Separate intact nucleic acids using gel electrophoresis or quantify using fluorescence-based techniques after degradation.
- Quantification: Calculate half-life by plotting percentage of intact nucleic acid versus time [12] [14].
This fundamental protocol enables direct comparison of protective capabilities across delivery platforms. For targeted systems, stability should be assessed both with and without targeting ligands to determine their potential impact on nuclease resistance.
Methodologies for Evaluating Intracellular Fate
Protocol 2: Live-Cell Imaging of Endosomal Escape
- Cell Preparation: Seed appropriate cell lines in glass-bottom dishes and culture to 60-80% confluence.
- Transfection: Add fluorescently labeled nucleic acid formulations (50-100 nM final concentration).
- Staining: Co-transfect with galectin-9-GFP or other membrane damage markers [15].
- Imaging: Conduct time-lapse microscopy using confocal or super-resolution systems at 37°C with 5% CO₂.
- Analysis: Quantify co-localization of nucleic acid signal with damage markers and track individual endosomes over time [15] [17].
This approach directly visualizes the critical endosomal escape step, identifying formulations that efficiently mediate cytosolic release versus those trapped in endolysosomal pathways. For targeted systems, receptor dependence can be validated through competitive inhibition with free ligands.
Visualization 1: The intracellular trafficking pathway of lipid nanoparticles, highlighting key decision points between functional cytosolic release and non-productive degradation pathways, with quantitative estimates based on live-cell imaging data [15] [17].
Methodologies for Immunogenicity Assessment
Protocol 3: Innate Immune Response Profiling
- Cell Models: Use primary human peripheral blood mononuclear cells (PBMCs) or specialized reporter cell lines (HEK-Blue hTLR).
- Stimulation: Treat cells with nucleic acid formulations across a concentration range (0.1-10 μg/mL).
- Cytokine Measurement: Quantify IFN-α, TNF-α, IL-6, and IP-10 production via ELISA at 6-24 hours post-treatment.
- Pathway Analysis: Assess specific PRR activation (TLR3/7/8, RIG-I, MDA5) using knockout cells or inhibitory oligonucleotides.
- Flow Cytometry: Evaluate dendritic cell maturation markers (CD80, CD86, CD83) [2] [14].
This comprehensive profiling enables researchers to identify the specific immune pathways activated by delivery systems and optimize formulations for either stealth delivery (protein replacement) or controlled immunostimulation (vaccine applications).
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Nucleic Acid Delivery Research
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Membrane Damage Sensors | Galectin-9-GFP, Galectin-3-mCherry [15] | Visualizing endosomal escape | Galectin-9 most sensitive for LNP-induced damage |
| Endosomal Markers | Rab5-GFP (early), Rab7-mCherry (late), LAMP1-RFP (lysosomal) [15] | Tracking intracellular trafficking | Multiple markers needed for complete pathway mapping |
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 [14] | LNP formulation | pKa optimization critical for endosomal escape |
| Targeting Ligands | GalNAc, Folate, Transferrin, RGD peptides [13] [12] | Cell-specific targeting | Receptor density and internalization capacity vary |
| Cationic Polymers | Chitosan (varied DDA%), PEI, PAMAM dendrimers [12] | Polyplex formation | Charge density and molecular weight determine efficacy |
| Fluorescent Reporters | Cy5-labeled siRNA, AF647-mRNA [15] | Particle tracking and quantification | Consider fluorophore quenching in intact nanoparticles |
Integrated Analysis: Targeted Versus Non-Targeted Systems
The comparative analysis reveals a nuanced landscape where targeted and non-targeted systems each occupy distinct therapeutic niches. Non-targeted LNP systems excel in applications where hepatic delivery is desirable, leveraging endogenous ApoE-mediated targeting to hepatocytes with established safety profiles [14]. Their formulation simplicity and scalability make them ideal for rapid vaccine deployment and liver-directed therapies like patisiran [13].
Receptor-targeted systems like GalNAc-siRNA conjugates demonstrate superior efficiency for specific cell types, achieving robust gene silencing at significantly lower doses through enhanced cellular uptake and reduced non-specific distribution [13]. Similarly, antibody-conjugated or ligand-functionalized nanoparticles show promise for extrahepatic targeting, though their clinical translation has been hampered by complex manufacturing and potential immunogenicity [16].
Visualization 2: Comparative mechanisms of non-targeted (ApoE/LDLR-mediated) versus targeted (ligand-receptor-mediated) delivery systems, highlighting their distinct cellular uptake pathways and tissue tropism [13] [14].
Emerging hierarchical targeting approaches represent the next frontier, combining multiple targeting modalities within a single system. These platforms may incorporate initial tissue-level targeting through size optimization, followed by cell-specific targeting through surface ligands, and finally subcellular localization through organelle-targeting peptides [16]. The development of stimuli-responsive systems that transform their properties at different biological milestones offers particular promise for addressing the paradoxical requirements of circulation, penetration, and internalization that have limited previous generations of delivery systems [16].
The resolution of the central delivery challenge requires continued innovation across multiple fronts. While significant progress has been made in understanding and overcoming enzymatic degradation and immunogenicity, intracellular delivery barriers remain the most significant bottleneck, with even advanced LNP systems achieving only modest endosomal escape efficiency [15] [17]. Future research directions should prioritize the development of more sophisticated delivery systems that dynamically adapt to their environment, the discovery of novel endosomolytic agents that enhance cytosolic release without excessive toxicity, and the creation of standardized assessment protocols that enable direct comparison across platforms.
The convergence of nucleic acid therapeutics with advances in bionanomaterials science, microfluidic production technologies like the NANOSPRESSO concept for point-of-care manufacturing, and artificial intelligence-driven formulation optimization promises to accelerate this progress [11] [18]. As these fields mature, the distinction between targeted and non-targeted systems may blur, giving rise to adaptive delivery platforms capable of navigating the entire delivery cascade—from administration to subcellular site of action—with unprecedented precision. Through continued systematic evaluation of how emerging platforms address the fundamental challenges of enzymatic degradation, cellular barriers, and immunogenicity, researchers can unlock the full therapeutic potential of nucleic acid medicines across an expanding range of clinical applications.
The therapeutic application of nucleic acids—including DNA, mRNA, and siRNA—represents a revolutionary advance in treating genetic disorders, cancers, and infectious diseases. However, the clinical success of these therapies is fundamentally constrained by the challenge of delivering these fragile macromolecules to their intended cellular targets [19] [20]. Nucleic acids exhibit poor inherent stability, rapid clearance from circulation, and limited cellular uptake due to their size and negative charge [20]. To overcome these biological barriers, scientists have developed sophisticated delivery systems that can be broadly categorized into non-targeted and targeted approaches.
Non-targeted delivery, primarily relying on passive accumulation mechanisms, formed the foundation of nanocarrier-based therapies. In contrast, targeted delivery employs active homing mechanisms to improve precision and therapeutic outcomes [21] [22]. This guide provides a systematic comparison of these core strategies, focusing on their operational principles, experimental evidence, and practical implementation for research and therapeutic development.
Fundamental Mechanisms: Passive vs. Active Targeting
Non-Targeted (Passive) Delivery
Non-targeted delivery systems operate primarily through the Enhanced Permeability and Retention (EPR) effect, a physiological phenomenon unique to solid tumors and inflamed tissues [21] [22]. Tumor vasculature is characterized by irregular architecture with gaps between endothelial cells (ranging from 100 to 1000 nanometers), combined with impaired lymphatic drainage. This combination allows nanocarriers (typically <150 nm) to extravasate from the bloodstream into tumor tissue and accumulate there over time [21].
The efficiency of passive targeting is governed by the nanocarrier's physicochemical properties:
- Size: Optimal particle sizes are approximately 100 nm for prolonged circulation and effective tumor accumulation [21].
- Surface Characteristics: Modification with hydrophilic polymers like polyethylene glycol (PEG) creates a "stealth" effect, reducing opsonization and clearance by the mononuclear phagocyte system (MPS), thereby extending circulation half-life [21] [22].
- Shape and Elasticity: These properties influence margination (movement toward vessel walls), extravasation potential, and cellular uptake profiles [22].
Despite its conceptual elegance, the EPR effect demonstrates significant heterogeneity across tumor types and individual patients, which limits the consistent clinical application of purely passive targeting strategies [22].
Targeted (Active) Delivery
Active targeting enhances delivery precision by decorating nanocarriers with targeting ligands that recognize and bind to specific receptors overexpressed on target cells [21] [22] [23]. This approach builds upon the passive accumulation foundation but adds a specific recognition layer.
Common targeting moieties include:
- Antibodies and Antibody Fragments: Provide high specificity and affinity for cell-surface antigens [23].
- Peptides: Often derived from natural ligands or discovered through phage display screens.
- Aptamers: Short, structured oligonucleotides with selective binding capabilities.
- Small Molecules: Such as folate for targeting folate receptor-overexpressing cancers.
The binding process, mediated by these ligands, can trigger receptor-mediated endocytosis, enhancing cellular internalization and potentially influencing intracellular trafficking [21]. A prominent example is the development of Antibody-Targeted Lipid Nanoparticles (Ab-LNPs), where antibodies conjugated to the LNP surface redirect particles from the liver to specific cells, such as T cells (via CD4) or lung endothelium (via PECAM-1) [23].
The diagram below illustrates the core mechanistic differences between these two fundamental strategies.
Comparative Performance Analysis
The selection between targeted and non-targeted strategies involves trade-offs across multiple performance parameters. The following table synthesizes quantitative and qualitative data from preclinical and clinical studies to illustrate these key differences.
Table 1: Performance Comparison of Targeted vs. Non-Targeted Delivery Systems
| Performance Parameter | Non-Targeted Systems | Targeted Systems | Experimental Evidence & Notes |
|---|---|---|---|
| Tumor Accumulation Efficiency | Typically <1% of injected dose [22] | Can reach ~10% in optimized systems; AI-optimized LNPs showed up to 89% in preclinical models [24] | High variability observed; depends on tumor model and EPR heterogeneity [22] |
| Cellular Uptake Mechanism | Non-specific fluid-phase pinocytosis [21] | Receptor-mediated endocytosis [21] [23] | Active targeting enhances uptake by 30-fold in specific cells (e.g., CD4+ T cells) [23] |
| Liver Accumulation | High (35-40% hepatic sequestration) [24] | Significantly reduced with proper targeting | Anti-PECAM-1 Ab-LNPs inhibited hepatic uptake, redirecting to lungs [23] |
| Therapeutic Efficacy | Moderate; improves pharmacokinetics [22] | Enhanced due to higher target site concentration | CPX-351 (passive) showed survival benefit in AML; Ab-LNPs enable in vivo CAR-T generation [22] [23] |
| Specificity & Off-Target Effects | Limited; relies on EPR effect only [22] | High for target cells; reduces systemic toxicity | Targeted LNPs reduce risks of acute liver toxicity and systemic side effects [23] |
| Manufacturing Complexity | Relatively simple [22] | Complex due to conjugation chemistry and characterization [22] | Scale-up challenges for actively targeted nanocarriers present translational hurdles [22] |
| Clinical Translation Status | Multiple FDA-approved products (e.g., Doxil, Onpattro) [22] [20] | Early clinical trials (e.g., Capstan's CPTX2309) [23] | No actively targeted NCs approved yet as of 2018; clinical progress emerging [22] [23] |
Experimental Protocols for Evaluation
Protocol: Evaluating Passive Targeting via the EPR Effect
Objective: Quantify the tumor accumulation and biodistribution of non-targeted nanocarriers in a murine model.
Materials:
- Nanocarrier: PEGylated liposomes (~100 nm) loaded with a near-infrared fluorophore (e.g., DiR) [21].
- Animal Model: Mice bearing subcutaneous xenograft tumors.
- Imaging System: In vivo fluorescence imaging system (e.g., IVIS).
- Analytical Tools: HPLC or gamma counter if using radiolabeled carriers.
Methodology:
- Formulation & Characterization: Prepare and characterize liposomes for size (100 nm optimal), PDI, zeta potential, and dye encapsulation efficiency [21].
- Administration: Inject DiR-liposomes intravenously via the tail vein.
- Longitudinal Imaging: Anesthetize mice and image at predetermined time points (e.g., 1, 4, 24, 48 hours) to track biodistribution and tumor accumulation.
- Ex Vivo Analysis: At endpoint (e.g., 48 hours), euthanize animals, collect tumors and major organs, and image ex vivo to quantify fluorescence intensity per gram of tissue.
- Data Analysis: Calculate tumor-to-background ratios and % injected dose per gram of tissue (%ID/g) [22].
Key Measurements:
- Blood Circulation Half-life: Determined by serial blood collection.
- Tumor Accumulation: Peak accumulation typically occurs between 24-48 hours [22].
- EPR Heterogeneity: Compare accumulation between different tumor models.
Protocol: Evaluating Active Targeting Efficiency
Objective: Compare the targeting efficiency and cellular uptake of ligand-functionalized vs. non-functionalized nanocarriers in vitro and in vivo.
Materials:
- Nanocarriers: Ligand-decorated LNPs (e.g., anti-CD4 Ab-LNPs) and non-targeted control LNPs [23].
- Cell Model: CD4+ T cells for in vitro studies.
- Animal Model: Appropriate disease model.
- Flow Cytometer: For quantifying cellular uptake.
Methodology:
- In Vitro Binding and Uptake:
- Incubate targeted and non-targeted LNPs (loaded with a fluorescent reporter) with CD4+ T cells.
- Use flow cytometry to quantify mean fluorescence intensity (MFI) per cell after incubation.
- Perform competitive inhibition by pre-blocking receptors with free antibodies [23].
- In Vivo Targeting:
- Systemically administer both LNP formulations to animal models.
- After 24 hours, harvest target tissues/organs and process into single-cell suspensions.
- Use flow cytometry or confocal microscopy to quantify particle delivery to specific cell populations.
- Functional Assessment:
- Load LNPs with therapeutic mRNA (e.g., Cre recombinase).
- Measure functional output (e.g., gene recombination efficiency) versus non-targeted controls [23].
Key Measurements:
- Fold-Enhancement in Delivery: Targeted vs. non-targeted MFI.
- Specificity Index: Uptake in target cells vs. non-target cells.
- Functional Payload Delivery: Efficacy of delivered nucleic acids.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of delivery strategies requires specific reagents and materials. The following table catalogues key components for formulating and evaluating targeted and non-targeted systems.
Table 2: Essential Reagents for Nucleic Acid Delivery Research
| Reagent / Material | Function & Application | Examples & Notes |
|---|---|---|
| Ionizable Lipids | Core component of LNPs; enables nucleic acid encapsulation and endosomal escape [24] | SM-102, DLin-MC3-DMA; pKa optimization critical for performance |
| PEGylated Lipids | Confers "stealth" properties, reduces MPS clearance, modulates particle size [21] [24] | DMG-PEG, DSPE-PEG; concentration and PEG chain length affect circulation time |
| Targeting Ligands | Confers specificity for active targeting strategies [21] [23] | Monoclonal antibodies (e.g., anti-PECAM-1, anti-CD4), peptides, aptamers |
| Fluorescent Probes | Tracking and quantifying biodistribution and cellular uptake [22] | Near-infrared dyes (DiR, Cy5.5); compatible with in vivo imaging |
| Characterization Instrumentation | Measuring critical quality attributes of nanocarriers [21] | Dynamic Light Scattering (size, PDI), Zetasizer (zeta potential), NMR/TLC (lipid quantification) |
| Specialized Lipids for Conjugation | Provides chemical handle for ligand attachment [23] | DSPE-PEG-Maleimide; reacts with thiol groups on antibodies or peptides |
Emerging Technologies and Future Directions
The field of nucleic acid delivery is rapidly evolving, with several emerging technologies poised to address current limitations.
Artificial Intelligence in Formulation Design: Machine learning models, including graph neural networks (GNNs) and generative adversarial networks (GANs), are accelerating LNP optimization by virtually screening millions of lipid structures. These AI-driven approaches can predict structure-property relationships with R² > 0.85, significantly reducing development timelines [24]. For instance, GAN-generated lipids have demonstrated structural novelty while maintaining higher encapsulation efficiency compared to traditionally developed lipids.
Advanced Targeting Modalities: Bispecific antibodies and peptide conjugates are expanding the repertoire of targeting options. Furthermore, researchers are exploring "dual targeting" approaches that combine two different siRNA payloads or targeting ligands to achieve synergistic effects and address tumor heterogeneity [10] [23].
Novel Delivery Platforms: Beyond conventional LNPs, platforms such as extracellular vesicles, polymeric nanoparticles, and hybrid systems offer complementary advantages for specific applications. The integration of stimuli-responsive elements (e.g., pH-sensitive linkers) enables triggered payload release in the tumor microenvironment [22].
The convergence of these advanced technologies with a deeper understanding of biological barriers will continue to push the boundaries of what is achievable with nucleic acid therapeutics, potentially enabling effective treatment for a broader range of diseases.
The field of RNA therapeutics represents one of the most transformative advancements in modern medicine, fundamentally changing our approach to treating genetic disorders, infectious diseases, and cancer. This journey from conceptual foundations to clinical reality has been marked by key scientific breakthroughs that progressively addressed fundamental challenges of RNA instability, immunogenicity, and delivery. The evolution from first-generation antisense oligonucleotides (ASOs) to the sophisticated RNA interference (RNAi) therapeutics and mRNA vaccines of today illustrates a remarkable scientific trajectory spanning nearly five decades [25]. This progression has occurred within the broader context of evaluating targeted versus non-targeted nucleic acid drug delivery systems, a critical determinant of therapeutic efficacy and safety. The development of these modalities underscores a continuous refinement in our ability to precisely modulate gene expression for therapeutic benefit, moving from simple hybridization-based strategies to complex cellular machinery hijacking and genetic reprogramming [2]. As the field matures, understanding these historical milestones provides invaluable insights for researchers and drug development professionals seeking to advance the next generation of nucleic acid therapeutics.
Major Historical Breakthroughs in RNA Therapeutics
The development of RNA therapeutics has followed a defined pathway of discovery and innovation, with each milestone building upon previous insights to overcome specific biological challenges. The table below chronicles the pivotal moments that have shaped the current landscape.
Table 1: Key Historical Milestones in RNA Therapeutics Development
| Year | Breakthrough Discovery/Event | Key Researchers/Entities | Significance and Impact |
|---|---|---|---|
| 1978 | First ASO Concept | Zamecnik and Stephenson [25] | Pioneered use of synthetic oligodeoxynucleotide to inhibit Rous sarcoma virus replication; established antisense principle |
| 1998 | RNA Interference (RNAi) Discovery | Fire and Mello [2] | Discovered potent gene silencing by double-stranded RNA in C. elegans; unveiled new regulatory pathway |
| 2001 | siRNA in Mammalian Cells | Elbashir et al. [25] | Demonstrated siRNA could silence genes in mammalian cell lines; enabled therapeutic application |
| 2003 | First In Vivo siRNA Proof | — | Showed intravenous Fas siRNA protected mice from fulminant hepatitis [2] |
| 2005 | mRNA Nucleoside Modification | Karikó and Weissman [2] | Pseudouridine modification reduced mRNA immunogenicity; crucial for therapeutic application |
| 2006 | Nobel Prize for RNAi | Fire and Mello [1] | Recognized foundational importance of RNA interference discovery |
| 2016 | First SMA ASO Drug (Nusinersen) | Biogen/Ionis [25] | FDA approved splice-switching ASO for spinal muscular atrophy; validated steric-blocking mechanism |
| 2018 | First siRNA Drug (Patisiran) | Alnylam [25] | FDA approved LNP-formulated siRNA for hATTR amyloidosis; validated RNAi clinical application |
| 2020 | mRNA COVID-19 Vaccines | Pfizer/BioNTech, Moderna [25] | Global validation of mRNA platform; demonstrated rapid vaccine development and scalability |
| 2023 | First CRISPR/Cas9 Therapy (Exa-cel) | Vertex/CRISPR Tx [25] | FDA approved for sickle cell disease and β-thalassemia; inaugurated therapeutic gene editing |
| 2024+ | Emerging Modalities (saRNA, circRNA) | Multiple entities [25] | Investigation of self-amplifying and circular RNAs for enhanced stability and durability |
The initial concept of antisense therapeutics emerged from the straightforward principle of Watson-Crick base pairing, with synthetic oligonucleotides designed to bind complementary RNA sequences and physically block translation or induce degradation [2]. The discovery of RNA interference revealed a natural, potent cellular pathway for gene silencing that could be harnessed therapeutically with synthetic small interfering RNAs (siRNAs), offering greater potency and specificity than early ASOs [1]. Parallel work on mRNA therapeutics focused on overcoming inherent instability and immunogenicity through nucleoside modifications and delivery system optimization, culminating in the dramatic success of COVID-19 vaccines [26]. Most recently, CRISPR-based technologies have expanded the toolbox to include precise gene editing, while novel RNA structures like circular RNAs and self-amplifying RNAs promise further enhancements in stability and therapeutic duration [25].
Comparative Analysis of Approved RNA Therapeutics
The clinical translation of RNA therapeutics has yielded numerous approved drugs across different modalities, each with distinct mechanisms, chemical modifications, and delivery strategies. The following table provides a comprehensive comparison of selected approved RNA therapeutics, highlighting the evolution from early to modern approaches.
Table 2: Comparison of Approved RNA Therapeutics Across Modalities
| Therapeutic (Brand Name) | RNA Modality | Target/Indication | Key Modifications | Delivery System | Year Approved |
|---|---|---|---|---|---|
| Nusinersen (Spinraza) | ASO (splice-switching) | SMN2 gene / Spinal Muscular Atrophy [25] | 2'-MOE phosphorothioate [1] | Intrathecal injection (no carrier) [1] | 2016 |
| Patisiran (Onpattro) | siRNA | Transthyretin (hATTR amyloidosis) [25] | 2'-O-methyl, 2'-fluoro [1] | Lipid Nanoparticles (LNP) [25] | 2018 |
| Givosiran (Givlaari) | siRNA | ALAS1 / Acute Hepatic Porphyria [27] | Extensive chemical stabilization [1] | GalNAc conjugate (liver-targeted) [25] | 2019 |
| Inclisiran (Leqvio) | siRNA | PCSK9 / Hypercholesterolemia [25] | Stabilizing modifications | GalNAc conjugate (liver-targeted) [28] | 2021 |
| mRNA-1273 (Moderna) | mRNA vaccine | SARS-CoV-2 Spike Protein [25] | N1-methylpseudouridine [26] | Lipid Nanoparticles (LNP) [25] | 2020 (EUA) 2022 (full) |
| COVID-19 mRNA Vaccine (Pfizer-BioNTech) | mRNA vaccine | SARS-CoV-2 Spike Protein [25] | N1-methylpseudouridine [26] | Lipid Nanoparticles (LNP) [25] | 2020 (EUA) 2022 (full) |
The comparison reveals a clear evolutionary trajectory in delivery strategies. Early approved ASOs like Nusinersen utilized local administration (intrathecal) without complex delivery systems, bypassing distribution challenges [1]. The first siRNA drug, Patisiran, required sophisticated lipid nanoparticles for systemic administration and tissue penetration [25]. Subsequent siRNA therapeutics (Givosiran, Inclisiran) adopted more precise GalNAc conjugation for efficient liver targeting without the complexity of nanoparticles, reflecting a trend toward targeted delivery approaches [25] [28]. Meanwhile, mRNA vaccines necessitated comprehensive LNP formulations to protect the large, fragile mRNA molecules and facilitate cellular uptake and endosomal escape [6]. The chemical modification strategies have also evolved, with early ASOs relying predominantly on phosphorothioate backbones and 2'-sugar modifications, while siRNAs and mRNA incorporate more diverse modifications including 2'-O-methyl, 2'-fluoro, and pseudouridine derivatives to enhance stability, reduce immunogenicity, and improve translational efficiency [26].
Delivery Systems: Targeted vs. Non-Targeted Approaches
The efficacy of RNA therapeutics is inextricably linked to delivery strategies, which have evolved from simple local administration to sophisticated targeted systems. The primary challenge remains overcoming multiple biological barriers: protection from nucleases, clearance by renal filtration and mononuclear phagocyte system, cellular uptake, endosomal escape, and intracellular trafficking to the correct subcellular compartment [6]. Different RNA modalities have distinct subcellular destinations—siRNA and mRNA function in the cytoplasm, while ASOs targeting nuclear pre-mRNA and CRISPR systems require nuclear access [6].
Non-Targeted Delivery Systems often rely on physical or chemical methods to enhance cellular uptake. Cationic lipids and polymers form nanoparticles through electrostatic interactions with negatively charged nucleic acids, protecting them and promoting cellular entry via endocytosis [6]. Lipid nanoparticles (LNPs), used in Patisiran and mRNA vaccines, represent the most clinically advanced non-targeted approach, offering robust encapsulation and endosomal escape capabilities but predominantly accumulating in the liver and spleen after systemic administration [25]. While effective for hepatocyte targets and intramuscular vaccines, this limited tropism restricts applications for extrahepatic diseases.
Targeted Delivery Systems employ specific ligands to direct therapeutics to particular cell types or tissues. The most successful example is GalNAc conjugation, which leverages high-affinity binding to the asialoglycoprotein receptor abundantly expressed on hepatocytes [29]. This approach has revolutionized siRNA therapeutics for liver diseases, enabling subcutaneous administration with efficient, specific uptake at lower doses and reduced off-target effects [28]. Emerging targeting strategies include cell-penetrating peptides, antibody conjugates, and ligand-modified LNPs directed to extrahepatic tissues like muscle, CNS, and tumors [29]. For instance, ASOs conjugated to muscle-targeting ligands have shown improved delivery in preclinical models of myotonic dystrophy [29].
The choice between targeted and non-targeted approaches involves trade-offs between specificity, complexity, manufacturing, and therapeutic application. Targeted systems generally offer superior pharmacokinetics and reduced side effects but require identification of appropriate receptors and ligand conjugation. Non-targeted systems provide broader applicability and easier formulation but may necessitate local administration or tolerate wider tissue distribution.
Figure 1: Pharmacological Barriers and Delivery Strategies for RNA Therapeutics. The diagram illustrates the sequential biological barriers that RNA therapeutics encounter and how targeted and non-targeted delivery systems employ different mechanisms to overcome them, resulting in distinct distribution outcomes [6].
Experimental Protocols for Evaluating Delivery Systems
Robust experimental methodologies are essential for evaluating the efficacy of nucleic acid delivery systems. The following protocols represent standard approaches used in the field to assess key parameters from in vitro characterization to in vivo performance.
Polyplex Formation and Stability Analysis
This protocol evaluates the formation and stability of nucleic acid-carrier complexes ("polyplexes"), a critical determinant of delivery efficiency [6].
Materials and Reagents:
- Nucleic Acid Cargo: siRNA, ASO, or mRNA diluted in nuclease-free buffer
- Delivery Carrier: Cationic polymer (e.g., PEI), lipid nanoparticle formulation, or GalNAc-conjugate
- Gel Electrophoresis System: Agarose, loading dye, ethidium bromide or SYBR Safe stain
- Dynamic Light Scattering (DLS) Instrument: For particle size and zeta potential measurement
- Heparin Sulfate Solution: For polyplex stability challenge
Procedure:
- Polyplex Formation: Prepare polyplexes at various carrier:nucleic acid weight or charge (N:P) ratios by adding the carrier solution to nucleic acid with gentle vortexing. Incubate for 30 minutes at room temperature.
- Gel Retardation Assay: Load polyplexes onto 1% agarose gel containing ethidium bromide. Run gel at 100V for 45 minutes. Visualize under UV light—complete nucleic acid retention in wells indicates efficient complexation.
- Particle Characterization: Dilute polyplexes in distilled water or specific buffer. Measure hydrodynamic diameter and polydispersity index (PDI) by DLS. Determine zeta potential using laser Doppler anemometry.
- Heparin Competition Assay: Incubate pre-formed polyplexes with increasing concentrations of heparin sulfate (a polyanion) for 30 minutes. Run on agarose gel to determine the minimum heparin concentration that dissociates polyplexes, indicating complex stability.
In Vitro Transfection Efficiency and Gene Silencing
This protocol assesses the functional delivery of RNA therapeutics in cell culture models, quantifying target gene modulation [6].
Materials and Reagents:
- Cell Line: Relevant to disease model (e.g., hepatocytes for liver-targeted therapeutics)
- Transfection Medium: Serum-free or reduced-serum medium appropriate for cell type
- Quantitative PCR (qPCR) System: Primers for target mRNA, reverse transcription kit, SYBR Green master mix
- Western Blot System: Antibodies against target protein and loading control
- Cell Viability Assay: MTT, MTS, or CellTiter-Glo reagents
Procedure:
- Cell Seeding: Plate cells in 24- or 96-well plates at appropriate density to reach 60-80% confluency at time of transfection.
- Treatment Application: Dilute nucleic acid polyplexes in serum-free medium. Replace cell culture medium with polyplex-containing medium. For GalNAc-conjugates, add directly to culture medium containing serum.
- Incubation and Harvest: Incubate cells for 24-72 hours at 37°C, 5% CO₂. Harvest cells for RNA extraction (qPCR) or protein extraction (Western blot) at appropriate timepoints.
- Gene Expression Analysis:
- Extract total RNA and synthesize cDNA.
- Perform qPCR with target-specific primers and normalize to housekeeping genes (e.g., GAPDH, β-actin).
- Calculate percentage gene silencing relative to untreated controls.
- Protein Expression Analysis:
- Perform Western blotting with target-specific antibodies.
- Quantify band intensity normalized to loading control.
- Viability Assessment: Treat parallel wells with identical formulations. After 24-48 hours, add MTT reagent and measure absorbance according to manufacturer's protocol. Express viability as percentage of untreated controls.
In Vivo Biodistribution and Efficacy
This protocol evaluates the tissue distribution and pharmacological activity of RNA therapeutics in animal models, providing critical preclinical data [6].
Materials and Reagents:
- Animal Model: Appropriate disease model (e.g., transgenic mice for human target)
- Formulation: RNA therapeutic in final delivery system (LNP, conjugate) in appropriate buffer for injection
- IVIS Imaging System (if using labeled formulations) or qPCR equipment for biodistribution
- Sample Collection: Tubes for tissue and blood collection, RNA stabilization reagents
- Clinical Chemistry Analyzer: For relevant disease biomarkers (e.g., serum TTR for amyloidosis models)
Procedure:
- Dosing Groups: Randomize animals into groups (n=5-8): untreated control, vehicle control, and treated groups with various doses/formulations.
- Administration: Administer formulation via relevant route (intravenous, subcutaneous, intrathecal). For biodistribution studies, use fluorescently labeled RNA (e.g., Cy5) or carrier.
- Biodistribution Analysis:
- At predetermined timepoints (e.g., 1, 4, 24 hours), euthanize animals and collect tissues (liver, spleen, kidney, lung, target tissue).
- For fluorescent imaging, image intact organs using IVIS system and quantify fluorescence intensity.
- For qPCR-based biodistribution, extract tissue RNA and quantify therapeutic RNA levels using specific probes.
- Pharmacodynamic Assessment:
- At therapeutic timepoints (days to weeks post-dose), collect tissue and blood samples.
- Isolate target tissue RNA and measure target mRNA reduction by qPCR.
- Measure relevant protein biomarkers in serum or tissue by ELISA or Western blot.
- Statistical Analysis: Compare results using appropriate tests (t-test, ANOVA) with significance at p<0.05.
The Scientist's Toolkit: Essential Research Reagents
Research in RNA therapeutics relies on specialized reagents and materials that enable the design, production, and evaluation of novel therapeutic candidates. The following table catalogizes key solutions essential for working in this field.
Table 3: Essential Research Reagents for RNA Therapeutics Development
| Reagent/Material | Supplier Examples | Primary Function and Research Application |
|---|---|---|
| Modified Nucleotides | TriLink BioTechnologies, Thermo Fisher | N1-methylpseudouridine, 2'-fluoro, 2'-O-methyl ribose substitutions; reduce immunogenicity, enhance stability [26] |
| Cationic Lipids/Polymers | Avanti Polar Lipids, Sigma-Aldrich | DOTAP, MC3, PEI; form nanostructured complexes with nucleic acids for cellular delivery [6] |
| GalNAc Conjugation Reagents | BroadPharm, Sigma-Aldrich | N-Acetylgalactosamine derivatives with activated esters; create liver-targeted oligonucleotide conjugates [29] |
| In Vitro Transcription Kits | New England Biolabs, Thermo Fisher | T7 polymerase, capping enzymes, nucleotide mixes; produce research-grade mRNA [2] |
| Lipid Nanoparticle Formulation Systems | Precision NanoSystems | Microfluidic chips and instruments; manufacture reproducible, size-controlled LNPs [25] |
| RNA-Induced Silencing Complex (RISC) Loading Assays | Reaction Biology, Eurofins | Components to monitor siRNA strand loading into RISC; assess functional potential [1] |
| Endosomal Escape Reporters | Thermo Fisher, ATCC | Galectin-8-GFP, fluorescent dyes with pH-sensitive properties; quantify endosomal release efficiency [6] |
These specialized research tools address the unique challenges of RNA therapeutic development. Modified nucleotides are fundamental for overcoming the inherent instability and immunogenicity of natural RNA, with specific modifications like N1-methylpseudouridine proven critical for therapeutic mRNA applications [26]. Cationic lipids and polymers serve as building blocks for non-viral delivery systems, enabling researchers to formulate and screen nanocarriers for specific applications [6]. The availability of GalNAc conjugation reagents has democratized the development of targeted siRNA therapeutics, mirroring the approach used in clinically approved products [29]. Sophisticated formulation systems allow laboratories to produce clinical-grade nanoparticles at benchtop scale, while functional assays for RISC loading and endosomal escape provide critical insights into the intracellular trafficking and mechanism of action beyond simple gene expression changes.
Figure 2: RNA Therapeutic Development Workflow. The diagram outlines the key stages in the research and development of RNA therapeutics, from initial design to clinical translation, highlighting essential tools and assays employed at each stage [25] [6] [26].
The journey from first-generation ASOs to modern RNAi therapeutics and mRNA vaccines represents a paradigm shift in pharmaceutical development, demonstrating the power of leveraging natural biological processes for therapeutic benefit. This evolution has been characterized by successive innovations addressing the fundamental challenges of nucleic acid delivery, with a clear trend toward increasingly sophisticated targeted approaches. The historical progression from simple antisense principles to the complex orchestration of RNA interference and genetic reprogramming underscores the remarkable acceleration of this field [25]. The critical importance of delivery systems is evident throughout this history, with breakthroughs in GalNAc conjugation and lipid nanoparticle formulation enabling the transition from laboratory concepts to clinical medicines [29] [6].
Future developments in RNA therapeutics will likely focus on expanding beyond current limitations, particularly the challenge of extrahepatic delivery [28]. Next-generation delivery technologies targeting the central nervous system, muscle, and other tissues are already in development, promising to broaden the therapeutic landscape [29]. Emerging modalities such as circular RNAs, self-amplifying RNAs, and RNA editing technologies represent the next frontier, offering potential solutions for enhanced durability, reduced dosing, and expanded therapeutic applications [25]. Furthermore, the integration of artificial intelligence and machine learning into RNA design and delivery optimization promises to accelerate the development process and enhance the precision of future therapeutics [28]. As the field continues to mature, the historical milestones chronicled in this review serve as both foundation and inspiration for the next generation of innovations that will further expand the boundaries of what is possible with RNA-targeted medicines.
Delivery Platform Architectures: From Passive Carriers to Active Targeting
The Enhanced Permeability and Retention (EPR) effect represents a cornerstone principle in cancer nanomedicine, enabling the passive targeting of therapeutic agents to tumor tissues without requiring specific molecular ligands. This phenomenon leverages the distinctive pathophysiology of solid tumors, which exhibit leaky vasculature with gaps between endothelial cells ranging from 100 nm to 2 μm, and impaired lymphatic drainage that reduces the clearance of accumulated particles [30]. Non-targeted lipid and polymer nanoparticles systematically exploit these anatomical abnormalities to achieve higher drug concentrations at tumor sites while minimizing damage to healthy tissues. For researchers evaluating targeted versus non-targeted delivery systems, understanding the capabilities and limitations of EPR-based strategies provides a crucial baseline for assessing the incremental value of active targeting approaches. While contemporary research increasingly focuses on ligand-functionalized nanoparticles, EPR-mediated delivery continues to offer substantial advantages in simplicity, manufacturability, and regulatory pathway familiarity, with several FDA-approved formulations relying exclusively on this passive targeting mechanism [31].
The clinical relevance of EPR-driven delivery systems continues to evolve, particularly as researchers develop more sophisticated nanoparticle designs that optimize EPR exploitation. Current estimates suggest that nanoparticles leveraging the EPR effect can achieve tumor drug concentrations representing 1–5% of the injected dose per gram of tumor tissue, a significant improvement over the less than 0.1% typically achieved with free-form chemotherapeutic drugs [31]. This review provides a comprehensive comparison of lipid and polymer nanoparticle platforms for non-targeted systemic delivery, examining their respective capabilities for harnessing the EPR effect, with specific attention to design parameters that maximize passive accumulation in malignant tissues.
Comparative Analysis of Nanoparticle Platforms for EPR Exploitation
Structural and Functional Characteristics
Different nanoparticle classes exhibit distinct advantages for EPR-mediated delivery based on their structural properties, composition, and drug release kinetics. The table below summarizes the key characteristics of major nanoparticle platforms used in non-targeted drug delivery.
Table 1: Comparison of Lipid and Polymer Nanoparticle Platforms for EPR-Based Delivery
| Nanoparticle Type | Optimal Size Range (nm) | Surface Charge Optimization | Drug Loading Capacity | Circulation Half-Life | Key Advantages for EPR |
|---|---|---|---|---|---|
| Liposomes | 80-150 | Neutral to slightly negative | High for hydrophilic drugs (aqueous core) and hydrophobic drugs (lipid bilayer) | Moderate to long (PEGylation extends circulation) | Excellent biocompatibility; tunable surface properties; established clinical translation |
| Solid Lipid Nanoparticles (SLNs) | 50-150 | Negative | Moderate for lipophilic drugs | Moderate | Enhanced stability over liposomes; controlled release; protection of encapsulated drugs from degradation |
| Polymeric Nanoparticles (e.g., PLGA) | 20-150 | Adjustable (positive for cancer cell targeting) | High for both hydrophilic and hydrophobic drugs | Moderate (depends on polymer biodegradation rate) | Precise controlled release kinetics; mechanical robustness; versatile surface functionalization potential |
| Lipid-Polymer Hybrid NPs (LPHNPs) | 70-130 | Tunable via shell composition | High for diverse drug types | Prolonged (combines advantages of both systems) | Synergistic benefits: stability of polymers + biocompatibility of lipids; core-shell structure for sequential release |
Quantitative Performance Metrics in EPR Exploitation
The effectiveness of nanoparticle systems in leveraging the EPR effect can be quantified through specific performance parameters established in preclinical studies. The following table compares key metrics across different nanoparticle platforms based on experimental data.
Table 2: Experimental Performance Metrics of Nanoparticle Platforms in Preclinical Models
| Nanoparticle Platform | Tumor Accumulation (% Injected Dose/g) | Peak Accumulation Time Post-Injection | Tumor-to-Normal Tissue Ratio | Key Evidence and Model System |
|---|---|---|---|---|
| PEGylated Liposomes (Doxil) | 3-5% | 24-48 hours | 5-10:1 | FDA-approved; human clinical data; accumulates in various solid tumors via EPR [31] |
| PLGA Nanoparticles | 2-4% | 12-24 hours | 4-8:1 | Demonstrated in lung cancer models; size-dependent accumulation with optimal range of 70-150 nm [30] |
| Lipid-Polymer Hybrid NPs | 3-6% | 24-72 hours | 8-15:1 | Shown in colorectal cancer and melanoma models; enhanced retention due to structural stability [32] [33] |
| Solid Lipid Nanoparticles | 1.5-3% | 12-24 hours | 3-6:1 | Documented in breast cancer models; slower release kinetics moderate tumor exposure levels |
Critical Design Parameters for Maximizing EPR Efficacy
Optimizing nanoparticles for EPR-mediated delivery requires careful consideration of several physicochemical parameters that collectively determine in vivo behavior and tumor accumulation:
Size Optimization: Nanoparticles in the 20-150 nm range demonstrate optimal EPR exploitation, as they are small enough to extravasate through leaky tumor vasculature yet large enough to avoid rapid renal clearance. Particles smaller than 5-10 nm are rapidly cleared by renal filtration, while those exceeding 200 nm may be sequestered by the spleen and liver [30]. Liposomes and polymeric nanoparticles can be precisely engineered within this optimal size window through manufacturing control of composition and formulation parameters.
Surface Charge and Functionalization: Cationic nanoparticles typically exhibit higher nonspecific cellular uptake but also increased clearance by the mononuclear phagocyte system, reducing circulation time and EPR-mediated tumor accumulation. Neutral or slightly negative surfaces (approximately -10 to -15 mV) optimize circulation half-life, while cationic surfaces (positive zeta potential) can enhance cancer cell interaction due to the net negative charge of cancer cell membranes resulting from the Warburg effect [30]. PEGylation creates a steric barrier that reduces opsonization and extends circulation time, enhancing EPR-mediated accumulation.
Drug Release Kinetics: Effective EPR exploitation requires a balance between circulation stability and timely drug release at the tumor site. Lipid-polymer hybrid nanoparticles (LPHNPs) exemplify this balance with a core-shell architecture where the polymeric core provides sustained release properties while the lipid shell offers biocompatibility and enhanced stability during circulation [32]. Premature drug release during circulation severely diminishes therapeutic efficacy despite successful tumor accumulation of the carrier itself.
Experimental Models and Methodologies for Evaluating EPR
Standardized Protocols for Assessing Nanoparticle Distribution
Establishing robust experimental methodologies is essential for accurately evaluating the EPR effect and comparing nanoparticle performance. The following protocols represent standardized approaches used in preclinical studies:
Protocol 1: Quantitative Biodistribution Analysis Using Radiolabeling
- Nanoparticle Labeling: Incorporate gamma-emitting radioisotopes (e.g., 111In, 99mTc) or fluorescent dyes (e.g., DiR, Cy5.5) into nanoparticle formulations during synthesis. For lipid nanoparticles, incorporate 3H-labeled phospholipids; for polymeric nanoparticles, use 14C-labeled polymers or encapsulate near-infrared fluorophores [31].
- Animal Models: Utilize murine models with subcutaneously implanted xenograft tumors (typically 500-800 mm3 in volume) or genetically engineered spontaneous tumor models. Orthotopic models may provide more realistic vascularization patterns.
- Administration and Tracking: Administer labeled nanoparticles via tail vein injection (dose: 5-20 mg nanoparticles/kg body weight). At predetermined time points (1, 4, 12, 24, 48, and 72 hours), euthanize animals (n=5-8 per time point) and collect tumors and major organs [30].
- Quantification: Measure radioactivity using a gamma counter or fluorescence intensity with an in vivo imaging system. Calculate percentage injected dose per gram of tissue (%ID/g) and tumor-to-normal tissue ratios for comparative analysis.
Protocol 2: Pharmacokinetic and Tumor Accumulation Profiling
- Blood Circulation Kinetics: Collect blood samples (50-100 μL) at serial time points post-injection (5, 15, 30 minutes; 1, 2, 4, 8, 12, 24 hours). Separate plasma and quantify nanoparticle concentration using appropriate analytical methods (HPLC, fluorescence measurement, or radioactivity counting) [32].
- Data Analysis: Fit plasma concentration-time data to a two-compartment pharmacokinetic model to determine key parameters: elimination half-life (t1/2β), area under the curve (AUC), and clearance (CL). Correlate pharmacokinetic parameters with tumor accumulation metrics.
- Histological Validation: Process tumor tissues for cryosectioning and fluorescence microscopy to visualize nanoparticle distribution within tumor regions. Co-staining with endothelial markers (CD31) assesses perivascular distribution, while staining for hypoxic regions reveals penetration to avascular areas [30].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for EPR and Nanoparticle Delivery Studies
| Reagent Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 | Enable efficient nucleic acid encapsulation and endosomal escape | pKa range of 6.2-6.5 optimizes endosomal escape; biodegradable variants reduce accumulation concerns [33] |
| Structural Lipids | DSPC, Cholesterol, DOPE | Form nanoparticle backbone and enhance membrane stability | Cholesterol content (30-50%) modulates membrane rigidity and drug release kinetics [34] |
| PEGylated Lipids | DMG-PEG2000, DSPE-PEG2000 | Provide steric stabilization, reduce protein opsonization, extend circulation | Optimal PEG density (1.5-5 mol%) balances circulation time and cellular uptake; PEG shedding strategies can improve target cell interaction [33] |
| Biodegradable Polymers | PLGA, PLA, Chitosan | Form nanoparticle matrix for controlled drug release | Varying lactide:glycolide ratios in PLGA (50:50 to 85:15) tunes degradation rates from weeks to months [32] |
| Tracking Agents | DiR, DiD, Cy5.5, 111In-oxine | Enable in vivo and ex vivo nanoparticle tracking | Near-infrared dyes (e.g., DiR) minimize tissue autofluorescence; radioisotopes provide quantitative biodistribution data [31] |
Visualization of EPR Mechanism and Experimental Workflow
The following diagrams illustrate the fundamental principles of EPR-mediated nanoparticle delivery and standard experimental approaches for its evaluation.
Diagram 1: EPR Effect Mechanism and Design Parameters. This illustrates how nanoparticle size, surface properties, composition, and drug release kinetics collectively influence EPR-mediated tumor accumulation.
Diagram 2: Experimental Evaluation Workflow. This outlines the standardized approach for assessing nanoparticle biodistribution, pharmacokinetics, and therapeutic efficacy in preclinical models.
Non-targeted lipid and polymer nanoparticles leveraging the EPR effect represent a mature yet continuously evolving platform for cancer drug delivery. While the EPR effect demonstrates significant variability between tumor types, individual patients, and even different regions within the same tumor, it remains a fundamental mechanism enabling selective drug accumulation in malignant tissues [31]. The optimization of nanoparticle physicochemical parameters—particularly size, surface characteristics, and drug release kinetics—can significantly enhance EPR-mediated delivery efficiency.
For researchers evaluating targeted versus non-targeted delivery systems, non-targeted nanoparticles present distinct advantages in formulation simplicity, manufacturing scalability, and regulatory approval pathways, with several EPR-dependent formulations already achieving clinical translation [34] [31]. The experimental frameworks and comparison data presented in this review provide foundational reference points for assessing the incremental benefits of active targeting strategies. As the field advances, non-targeted nanoparticles continue to serve as both therapeutic modalities in their own right and essential benchmarks against which more complex targeted systems must demonstrate superior efficacy.
The development of nucleic acid therapeutics, including small interfering RNA (siRNA) and antisense oligonucleotides (ASOs), represents a revolutionary approach for treating previously undruggable diseases. However, the efficient delivery of these macromolecules to specific tissues and cells remains a formidable challenge in clinical translation. Among various targeting strategies, ligand-conjugated platforms have emerged as a powerful solution for hepatocyte-specific delivery, with GalNAc (N-acetylgalactosamine)-based systems standing out as a particularly successful example. This paradigm leverages the natural biology of the asialoglycoprotein receptor (ASGPR), a lectin highly expressed on hepatocytes, to achieve precise tissue and cell-type targeting [35] [36].
The fundamental advantage of active targeting systems like GalNAc conjugates lies in their ability to transform the pharmacokinetic and pharmacodynamic properties of nucleic acid drugs. These systems facilitate receptor-mediated endocytosis, enabling therapeutic payloads to bypass numerous biological barriers that would otherwise preclude intracellular delivery. Within the broader context of nucleic acid drug delivery research, GalNAc-conjugated platforms occupy a strategic position between non-targeted "naked" oligonucleotides and more complex nanoparticle-based delivery systems, offering a balance of synthetic simplicity, targeting efficiency, and clinical viability that has propelled their rapid adoption [36] [37].
Biological Mechanism of ASGPR-Mediated Targeting
Receptor Structure and Function
The asialoglycoprotein receptor (ASGPR), also known as the Ashwell-Morell receptor, is a calcium-dependent C-type lectin that was the first animal lectin to be discovered [35] [38]. This transmembrane receptor is primarily expressed on the sinusoidal surface of hepatocytes, with minimal extra-hepatic expression, making it an ideal target for liver-directed therapies [38] [37]. ASGPR exists as a hetero-oligomeric complex composed of two homologous subunits, ASGPR1 and ASGPR2, with molecular weights ranging from 40 to 60 kDa [38]. These subunits form a functional receptor unit that typically presents in abundance, with approximately 500,000 copies per hepatocyte, of which about 5-10% are present on the cell surface at any given time [35] [37].
The receptor's carbohydrate recognition domain (CRD) forms a shallow binding pocket that specifically interacts with terminal galactose (Gal) or N-acetylgalactosamine (GalNAc) residues [38]. This interaction exhibits a marked preference for GalNAc, which demonstrates 10-60-fold higher affinity compared to galactose in competition assays [38]. The CRD achieves binding specificity through coordinated interactions with hydroxyl groups at positions 3 and 4 of the sugar ring, with substituents at position 2 also contributing to binding affinity [38]. This precise molecular recognition mechanism forms the structural basis for the targeting specificity of GalNAc-conjugated therapeutics.
Intracellular Trafficking Pathway
The journey of GalNAc-conjugated therapeutics from receptor binding to intracellular release follows a well-defined trafficking pathway that leverages the natural recycling mechanism of ASGPR. The process begins with the binding of multivalent GalNAc ligands to ASGPR on the hepatocyte surface, which initiates rapid local aggregation of ligand-bound receptors into clathrin-coated pits [35]. This clustering triggers endocytosis, typically within 10-15 minutes of ligand engagement, and the resulting vesicles progress through the endosomal compartment [35] [36].
As the endosomes mature and undergo acidification, the decreasing pH environment causes dissociation of the GalNAc ligand from ASGPR, facilitated by the pH-sensitive nature of the receptor-carbohydrate interaction [36] [37]. The receptor then recycles back to the cell surface with a remarkably short cycle time of approximately 15 minutes, regardless of ligand presence, enabling multiple rounds of internalization [38]. Meanwhile, the therapeutic payload must escape the endosomal compartment before lysosomal degradation occurs—a critical and still not fully understood step that remains a focus of ongoing research [35]. The successfully escaped nucleic acid payload is then free to engage with its intracellular targets, such as the RNA-induced silencing complex (RISC) for siRNAs or specific mRNA transcripts for ASOs [36].
Diagram 1: ASGPR-Mediated Endocytosis and Intracellular Trafficking Pathway for GalNAc-Conjugated Therapeutics
Comparative Analysis: GalNAc Conjugates vs. Alternative Delivery Systems
Direct Comparison with Non-Targeted and Nanoparticle Approaches
The advancement of GalNAc-conjugated platforms must be evaluated against relevant alternative delivery strategies, particularly non-targeted oligonucleotides and lipid nanoparticle (LNP) formulations. Each approach demonstrates distinct advantages and limitations across critical parameters including delivery efficiency, tissue specificity, manufacturability, and clinical feasibility.
Table 1: Comparative Analysis of Hepatocyte-Targeted Delivery Systems
| Parameter | GalNAc Conjugates | Non-Targeted Oligonucleotides | Lipid Nanoparticles (LNPs) |
|---|---|---|---|
| Targeting Mechanism | Active targeting via ASGPR receptor-mediated endocytosis [36] | Passive distribution primarily to liver non-parenchymal cells [36] | Apolipoprotein E-mediated uptake via LDL receptor [39] |
| Hepatocyte Specificity | High (>80% hepatocyte uptake) [36] | Low (<30% hepatocyte uptake) [36] | Moderate (preferential liver distribution) [39] |
| Delivery Efficiency | 6-7 fold increase in hepatocyte drug levels compared to non-targeted ASOs [36] | Baseline efficiency with predominant Kupffer cell uptake [36] | High efficiency but broader cell type uptake [39] |
| Structural Complexity | Low-moderate (defined chemical conjugate) [37] | Low (naked oligonucleotide) | High (multicomponent formulation) [39] |
| Manufacturing | Relatively simple, solid-phase synthesis compatible [37] | Simple | Complex nanoparticle formation [39] |
| Administration Route | Subcutaneous [39] | Typically intravenous or subcutaneous | Intravenous [39] |
| Dosing Frequency | Extended duration (up to 3-6 months) [36] | More frequent dosing required | Varies by application |
| Clinical Validation | Multiple approved drugs and clinical candidates [36] [38] | Established with limitations | Approved products (patisiran, COVID-19 vaccines) [39] [40] |
The quantitative superiority of GalNAc conjugates is particularly evident in cellular distribution studies. Research comparing unconjugated ASOs with GalNAc-conjugated counterparts demonstrated a dramatic shift in tissue distribution profiles. Unconjugated ASOs administered systemically were predominantly (>70%) taken up by the non-parenchymal cellular fraction of the liver, while GalNAc-conjugated ASOs showed reversed distribution with predominant (>80%) uptake by hepatocytes [36]. This targeted delivery translated to approximately 6-7 fold increased ASO drug levels in hepatocytes at equivalent doses and contributed to a corresponding 7-fold increase in potency for target mRNA knockdown in vivo [36].
Quantitative Efficacy and Potency Metrics
The enhanced targeting efficiency of GalNAc conjugates translates directly to improved pharmacological metrics, with substantial advancements observed in both preclinical models and clinical applications. These improvements are quantifiable across multiple parameters including potency, duration of action, and therapeutic index.
Table 2: Quantitative Efficacy Comparison of Delivery Platforms
| Therapeutic Platform | In Vivo Potency Improvement | Clinical Dose Advantage | Duration of Action | Key Modifications |
|---|---|---|---|---|
| GalNAc-siRNA Conjugates | Up to 10-fold with vinyl phosphonate modification [36] | 280-fold reduction with enhanced stabilization chemistry vs. 1st generation [36] | Up to 3 months in non-human primates [36] | Alternating 2'-O-methyl/2'-fluoro nucleotides with phosphorothioate bonds [36] |
| GalNAc-ASO Conjugates | 7-11 fold improvement for multiple targets [36] | 10-30 fold lower doses vs. non-targeted ASOs [36] [37] | Several weeks to months | 5'-end conjugation preferred, gapmer designs [37] |
| Non-Targeted ASOs | Baseline | Baseline | Days to weeks | Phosphorothioate backbone, 2'-modifications |
| LNP-siRNA | High but non-specific | N/A (different dosing paradigm) | Several weeks | Ionizable lipids, phospholipids, cholesterol, PEG lipids [39] |
The evolution of chemical modification strategies has been instrumental in achieving these improved metrics. For GalNAc-siRNA conjugates, optimization has progressed from partially modified first-generation constructs to extensively modified architectures incorporating alternating 2'-O-methyl and 2'-fluoro nucleotides with phosphorothioate (PS) linkages at the strand extremities [36]. Further advancements include the implementation of 5' vinyl phosphonate modifications, which protect the siRNA from degradation and eliminate the need for intracellular phosphorylation, resulting in up to 10-fold potency increases for some sequences [36]. Similarly, GalNAc-ASO conjugates have benefited from strategic placement of the ligand (preferably at the 5' end) and incorporation of high-affinity modifications such as locked nucleic acids (LNAs), which have demonstrated up to 20-fold potency improvements in animal models [37].
Experimental Evidence and Validation
Key Preclinical Studies and Methodologies
The validation of GalNAc-conjugated platforms rests on rigorous preclinical experimentation employing standardized methodologies to quantify targeting efficiency, gene silencing efficacy, and duration of action. Key experimental approaches include:
Cellular Distribution Studies: Researchers have employed radiolabeled or fluorescently tagged oligonucleotides with and without GalNAc conjugation to quantitatively assess tissue and cell-type distribution. A pivotal methodology involves separating hepatocytes from non-parenchymal liver cells (Kupffer cells, endothelial cells) after oligonucleotide administration to determine the percentage of dose delivered to each cell population [36]. These studies consistently demonstrate that GalNAc conjugation redirects oligonucleotides from non-parenchymal cells (the primary uptake site for unconjugated ASOs) to hepatocytes, with distribution shifting from >70% non-parenchymal uptake for unconjugated ASOs to >80% hepatocyte uptake for GalNAc conjugates [36].
Target Engagement and Gene Silencing Evaluation: The functional consequence of improved hepatocyte delivery is quantified through mRNA and protein level measurements of target genes. Standard protocols involve administering GalNAc-conjugated siRNAs or ASOs to animal models (typically mice, rats, or non-human primates) and measuring target reduction in liver tissue using qRT-PCR for mRNA assessment and Western blot or ELISA for protein quantification [36]. For example, studies targeting genes such as SRB1, TTR, and APOC3 have demonstrated 7-11 fold improvements in potency for GalNAc conjugates compared to their non-conjugated counterparts [36].
Duration of Action Assessment: The enhanced stability of chemically modified GalNAc conjugates enables extended pharmacological activity. Experimental protocols for evaluating duration involve single administration of test compounds followed by serial measurements of target mRNA or protein levels over extended periods (up to several months in non-human primates) [36]. These studies have confirmed that advanced GalNAc-siRNA conjugates can maintain target suppression for up to 3 months after a single subcutaneous dose [36].
Diagram 2: Standard Experimental Workflow for Evaluating GalNAc-Conjugated Therapeutics
Clinical Validation and Approved Therapeutics
The transition of GalNAc-conjugated platforms from preclinical validation to clinical application represents one of the most successful stories in oligonucleotide therapeutics. Multiple GalNAc-conjugated drugs have received regulatory approval, with numerous additional candidates in advanced clinical development [36] [38].
The clinical benefits observed with GalNAc conjugates directly mirror the improvements demonstrated in preclinical models. The dramatic (10-30 fold) increases in potency observed in animal studies have successfully translated to human applications, enabling significantly lower doses of GalNAc-conjugated therapeutics compared to non-targeted alternatives [36]. This enhanced potency, combined with extended duration of action, allows for less frequent dosing regimens—a substantial benefit for patients with chronic conditions requiring long-term therapy.
The approval of givosiran (Givlaari) for acute hepatic porphyria in 2019 marked the first FDA-approved GalNAc-siRNA conjugate, validating the clinical potential of this delivery platform [36]. This was rapidly followed by additional approvals including lumasiran (Oxlumo) for primary hyperoxaluria type 1, vutrisiran (Amvuttra) for hereditary transthyretin-mediated amyloidosis, and inclisiran (Leqvio) for hypercholesterolemia [39] [36]. The expanding clinical pipeline now encompasses at least seven GalNAc conjugates in registrational review or Phase 3 trials, with an additional 21 candidates at earlier clinical stages, targeting a diverse range of hepatic diseases [36].
Research Toolkit: Essential Reagents and Methodologies
The successful implementation of GalNAc-conjugated delivery systems requires specialized reagents, analytical tools, and experimental methodologies. The following research toolkit outlines critical components for investigating and developing these targeted delivery platforms.
Table 3: Essential Research Toolkit for GalNAc-Conjugated Platform Development
| Category | Specific Reagents/Techniques | Function/Application | Key Considerations |
|---|---|---|---|
| Ligand Chemistry | Trimeric GalNAc ligands [38] | High-affinity ASGPR targeting | Optimal 20Å spacing between terminal sugars [38] |
| Oligonucleotide Modifications | 2'-O-methyl, 2'-fluoro nucleotides [36] | Enhanced nuclease stability and potency | Alternating patterns in siRNA strands [36] |
| Backbone Modifications | Phosphorothioate (PS) linkages [36] | Improved protein binding, tissue distribution | Placement at oligonucleotide extremities [36] |
| Stability Enhancements | 5' vinyl phosphonate [36] | Protection from degradation, eliminates phosphorylation requirement | Up to 10-fold potency increase [36] |
| Conjugation Methods | Solid-phase synthesis-compatible linkers [37] | Covalent attachment of GalNAc to oligonucleotides | Yields comparable to standard oligonucleotides [37] |
| Analytical Characterization | Mass spectrometry [37] | Quality control of final conjugates | Confirmation of chemical structure and purity |
| In Vitro Models | Primary hepatocytes, HepG2 cells [36] | ASGPR expression and function validation | Species differences in ASGPR affinity [38] |
| In Vivo Models | Mice, rats, non-human primates [36] | Pharmacokinetic and efficacy assessment | Translation to clinical potency [36] |
The trimeric GalNAc ligand represents a particularly critical component, as the multivalency effect dramatically enhances binding affinity. While monovalent GalNAc exhibits binding in the millimolar range, trimeric configurations achieve nanomolar affinity—representing an approximately 10^6-fold increase despite only a three-fold increase in absolute GalNAc concentration [38]. This "cluster effect" is maximized in trivalent ligands, as the affinity increase from triantennary to tetraantennary ligands is only modest [38]. The standard scaffold for these trivalent ligands is typically based on tris(hydroxymethyl)aminomethane (Tris), with carbohydrate ligands attached via ether, ester, or amide-based linkers optimized for proper geometry and hydrophilicity-hydrophobicity balance [38].
GalNAc-conjugated platforms have unequivocally demonstrated their value as efficient, targeted delivery systems for hepatocyte-directed nucleic acid therapeutics. The compelling experimental data and growing clinical validation underscore several key advantages: exceptional hepatocyte specificity facilitated by ASGPR-mediated endocytosis, significantly enhanced potency compared to non-targeted approaches, extended duration of action enabling favorable dosing regimens, and synthetic tractability supporting manufacturing scalability.
When objectively evaluated against alternative delivery strategies, GalNAc conjugates occupy a strategic middle ground—offering superior cell-type specificity compared to non-targeted oligonucleotides while maintaining simpler composition and manufacturing than complex nanoparticle systems. The quantitative evidence from both preclinical and clinical studies consistently demonstrates 6-7 fold improvements in hepatocyte delivery and corresponding potency enhancements that have successfully translated to multiple approved therapeutics.
The future trajectory of GalNAc-conjugated platforms will likely focus on several key areas: first, continued optimization of oligonucleotide chemistry to further enhance potency and duration while minimizing potential off-target effects; second, expansion of the approach beyond siRNAs and ASOs to encompass newer modalities such as anti-microRNAs, small activating RNAs, and potentially gene editing systems; and third, application to increasingly diverse hepatic diseases as the platform demonstrates its versatility. The remarkable success of GalNAc-mediated hepatocyte targeting has also stimulated increased interest in developing analogous targeting strategies for extrahepatic tissues, potentially unlocking new therapeutic opportunities beyond liver-directed applications. As the field advances, GalNAc-conjugated platforms will continue to serve as both valuable therapeutic tools in their own right and exemplars for the development of next-generation targeted delivery systems.
The success of nucleic acid-based therapies hinges on the efficient and safe delivery of genetic material to target cells. The choice of delivery vector is therefore a critical determinant in the preclinical and clinical success of gene therapies, vaccines, and gene-editing applications. This guide provides a comparative analysis of three leading vector systems: Adeno-Associated Virus (AAV), Lentivirus, and synthetic Lipid Nanoparticles (LNPs). Framed within a broader thesis on targeted versus non-targeted delivery systems, this article objectively compares their performance based on current literature and experimental data, serving as a reference for researchers and drug development professionals.
The fundamental operational logic for selecting and applying these vector systems is summarized in the decision flowchart below.
The core characteristics of these vectors are directly compared in the table below, which synthesizes key performance metrics critical for experimental design.
Table 1: Core Characteristics of AAV, Lentivirus, and Lipid Nanoparticles
| Parameter | Adeno-Associated Virus (AAV) | Lentivirus (LV) | Synthetic Lipid Nanoparticles (LNPs) |
|---|---|---|---|
| Genetic Material | Single-stranded DNA | Single-stranded RNA (integrating) | mRNA, siRNA, plasmid DNA, CRISPR RNP |
| Cargo Capacity | ~4.7 kb [41] | ~8 kb | High/Large (theoretically unlimited) [41] |
| Immune Response | Pre-existing immunity to capsids; can trigger immune response [42] [41] | Lower pre-existing immunity; immune response concerns | Lower immunogenicity; suitable for repeated dosing [42] |
| Integration Profile | Predominantly non-integrating (episomal) | Integrates into host genome [42] | Non-integrating; transient expression [42] |
| Expression Duration | Long-term (months to years) | Long-term/Permanent (due to integration) [42] | Transient (days to weeks) [42] |
| In Vivo Applications | Excellent for direct in vivo gene therapy [43] | Primarily for ex vivo cell engineering (e.g., CAR-T) [43] | Excellent for in vivo delivery (e.g., vaccines, siRNA) [42] |
| Key Advantage | High in vivo transduction efficiency; long-term expression | Stable genomic integration for dividing cells | Flexible cargo capacity; low immunogenicity; scalable manufacturing [41] |
| Key Limitation | Limited cargo capacity; immunogenicity; complex GMP production [44] [45] | Risk of insertional mutagenesis; complex GMP production | Primarily transient expression; off-target accumulation (e.g., liver) [46] |
Experimental Data and Performance Comparison
Quantitative data from recent studies and clinical applications highlight the distinct performance profiles of each vector system.
Table 2: Quantitative Performance and Manufacturing Comparison
| Metric | AAV | Lentivirus | Synthetic LNPs |
|---|---|---|---|
| Typical In Vivo Transduction Efficiency | High (e.g., >90% in targeted tissues) [42] | High (ex vivo) | Moderate to High (dose-dependent) [42] |
| Particle-to-Infectivity Ratio | Favorable | Adversely affected by retro-transduction [47] | Not applicable (non-infectious) |
| Manufacturing Titer/Yield | Low yields; scalability challenges [45] | Moderate titers; impacted by retro-transduction (60-90% loss) [47] | High, scalable yields [42] [41] |
| GMP Manufacturing Cost | High (complex purification) [41] | High (complex processes) [41] | Lower (synthetic, scalable processes) [41] |
| Clinical-Stage Therapies (Examples) | ~635 therapies in development [44]; 6+ approved (e.g., Luxturna, Zolgensma) [43] [44] | Approved CAR-T therapies (e.g., Kymriah) [43] | 2+ approved (Onpattro, COVID-19 vaccines); numerous in development |
Detailed Experimental Insights and Protocols
Investigating Lentiviral Vector Retro-Transduction
A key challenge in LV production is retro-transduction, where producer cells are transduced by their own viral output, significantly reducing harvestable yield [47].
Experimental Protocol: Quantifying Retro-Transduction
- Objective: To determine the rate of retro-transduction in a stable, inducible LV producer cell line and its impact on infectious titer.
- Methodology:
- Cell Culture: Use stable inducible suspension producer clones (e.g., based on GPRG/GPRTG packaging cell lines) in a stirred-tank bioreactor [47].
- Induction & Sampling: Induce vector production and collect cell samples at multiple time points post-induction (e.g., days 0, 3, 7, 11, 18).
- gDNA Extraction: Isolate genomic DNA from the producer cells at each time point.
- Digital Droplet PCR (ddPCR): Perform ddPCR on the gDNA using primer/probe sets designed to differentiate between the stably integrated packaging cassettes and the vector genome of the produced LV (e.g., targeting the WPRE sequence) [47].
- Titer Measurement: In parallel, measure the infectious titer (TU/mL) in the cell culture supernatant at each harvest point.
- Key Analysis: Calculate the average vector copy number (VCN) per cell over time. Correlate the VCN with the infectious titer data. Studies report that 60-90% of infectious LV can be lost due to retro-transduction, with VCNs exceeding 450 copies/cell observed in some clones [47].
The experimental workflow and core challenge of this protocol are visualized below.
Developing Targeted Lipid Nanoparticles for Extra-Hepatic Delivery
A major focus in LNP research is overcoming natural tropism for the liver. A recent study developed vascular endothelial cell-targeted LNPs (vtLNPs) for mRNA delivery to prevent thrombosis [46].
Experimental Protocol: Screening Targeted LNPs
- Objective: To screen a library of novel ionizable lipids for LNP formulations that selectively deliver mRNA to vascular endothelial cells.
- Methodology:
- Lipid Synthesis: Design and synthesize a library of novel ionizable lipids using core skeletons like cyclohexane and malonates, which allow for easy structural variation [46].
- LNP Formulation: Formulate LNPs using each novel ionizable lipid, combined with standard helper lipids (DSPC, cholesterol, and PEG-lipid), via microfluidics.
- DNA Barcoding: Load each distinct LNP formulation with a unique DNA barcode sequence, creating a pooled library [46].
- In Vivo Screening: Administer the pooled LNP library intravenously to mouse models.
- Tissue Analysis: Isolate various tissues (e.g., lung, liver, spleen). Extract and sequence the DNA barcodes from vascular endothelial cells (e.g., isolated via fluorescence-activated cell sorting using specific markers like CD31) and other cell types.
- Hit Identification: Identify the top-performing ionizable lipid(s) based on the enrichment of its specific DNA barcode in the target endothelial cells relative to non-target cells (e.g., hepatocytes).
- Key Findings: This screening identified a lead vtLNP that, when loaded with TPA mRNA, effectively delivered the mRNA to vascular endothelial cells and secreted TPA protein into the blood, with no detectable TPA expression in hepatocytes. This mitigated the risk of TPA-induced lipid metabolism disorders and significantly prevented venous thrombosis in a mouse model [46].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Vector Research and Development
| Reagent / Solution | Function / Application | Relevant Vector System |
|---|---|---|
| HEK293T Cells | Standard cell line for transient transfection-based production of AAV and Lentivirus. | AAV, Lentivirus |
| Stable Inducible Producer Cell Lines (e.g., GPRG) | Generate LV without transfection; used to study production challenges like retro-transduction [47]. | Lentivirus |
| Ionizable Lipids (e.g., SM-102, DLin-MC3-DMA) | Critical component of LNPs for encapsulating nucleic acids; structure influences tropism and efficiency [24] [46]. | LNP |
| DNA Barcodes | Enable high-throughput in vivo screening of LNP libraries for tissue tropism [46]. | LNP |
| VSV-G Envelope Protein | Most common envelope for pseudotyping LV and AAV; confers broad tropism by binding LDLR [47]. | Lentivirus, AAV |
| Affinity Chromatography Resins (e.g., AAV serotype-specific) | Critical for downstream purification of full AAV capsids from empty capsids during GMP manufacturing [45]. | AAV |
| PEGylated Lipids (e.g., DMG-PEG2000) | Used in LNP formulations to modulate particle size, stability, and pharmacokinetics. | LNP |
Emerging Trends and Future Perspectives
The field of vector development is rapidly evolving, with several key trends shaping its future:
- AI-Driven Vector Design: Machine learning and generative adversarial networks (GANs) are now being used to virtually screen millions of lipid structures to predict properties like efficacy, toxicity, and tropism, dramatically accelerating LNP development [24].
- Overcoming Manufacturing Hurdles: For AAV, innovations in high-density perfusion cultures and serotype-agnostic purification are addressing critical bottlenecks in yield and scalability [45]. For LV, novel strategies like the ENV-Y system are being explored to reduce retro-transduction and improve yields [47].
- Hybrid and Advanced Systems: The convergence of viral and non-viral technologies is promising. For instance, non-viral systems are being engineered to achieve the tissue specificity once dominated by viral vectors, while also offering the cargo flexibility and safety profile essential for next-generation gene editing [41].
The therapeutic application of nucleic acids (NAs)—including DNA, mRNA, siRNA, and ASOs—represents a paradigm shift in precision medicine, offering potential cures for genetic disorders, cancers, and infectious diseases [48]. The fundamental challenge limiting their clinical translation, however, is the safe and efficient delivery of these large, negatively charged, and enzymatically degradable molecules to specific target cells [49] [48]. The core thesis of this guide is that delivery systems can be categorized into targeted strategies, which use specific molecular recognition to localize therapeutic effects, and non-targeted strategies, which rely on passive accumulation or local confinement. This guide objectively compares three emerging material classes—inorganic nanoparticles, biomaterial scaffolds, and nucleic acid nanostructures—evaluating their performance as NA delivery vehicles within this targeted versus non-targeted framework, supported by experimental data and protocols.
Material Class Profiles and Performance Comparison
Inorganic Nanoparticles: Versatile and Stimuli-Responsive Vectors
Overview: Inorganic nanoparticles (NPs) are synthetic materials with dimensions of 1-100 nm, engineered from metals, metal oxides, semiconductors, or carbon-based compounds [50]. Their application in NA delivery leverages their tunable size, shape, and surface chemistry, as well as unique intrinsic properties like magnetism, fluorescence, and photothermal conversion [51] [50].
Mechanism of Action: Inorganic NPs primarily function as protective carriers. NAs can be adsorbed onto their surface or encapsulated within hybrid structures. They facilitate cellular uptake via endocytosis. A key advantage is their ability to be engineered for active targeting by conjugating ligands (e.g., antibodies, peptides) to their surface for specific receptor binding [50]. Furthermore, their intrinsic properties enable stimuli-responsive release (e.g., using magnetic hyperthermia or near-infrared light to trigger NA release from gold nanoshells or carbon-based materials) [50].
Table 1: Key Characteristics and Experimental Performance of Inorganic Nanoparticles for NA Delivery.
| Material Type | Common Examples | Key Advantages for NA Delivery | Typical Loading Efficiency | Reported Transfection Efficiency In Vitro | Key Limitations |
|---|---|---|---|---|---|
| Gold Nanoparticles | Nanospheres, Nanorods | Easy functionalization, biocompatibility, photothermal properties [50]. | >80% (for thiol-conjugated oligonucleotides) [50] | 60-75% (model cell lines, e.g., HeLa) [50] | Potential cytotoxicity at high concentrations [50]. |
| Magnetic Nanoparticles | Iron Oxide (Fe₃O₄) | MRI contrast, magnetic targeting, hyperthermia-triggered release [50]. | 70-90% [50] | N/A (Often used for targeting and triggered release) | Aggregation in biological fluid, complex surface modification needed [50]. |
| Quantum Dots | CdSe, CdTe, InP | Optical imaging and tracking capabilities [50]. | N/A (Primarily used as probes) | N/A (Primarily used as probes) | Heavy metal toxicity concerns, blinking effect [50]. |
| 2D Nanomaterials | Graphene, MXenes | High surface area for loading, photothermal therapy [50]. | >85% (via π-π stacking) [50] | Up to 70% [50] | In vivo biodegradation and long-term toxicity are not fully understood [50]. |
Biomaterial Scaffolds: Localized and Sustained Release Depots
Overview: Biomaterial scaffolds are three-dimensional structures designed to mimic the native extracellular matrix (ECM) [51] [49]. They provide a temporary physical support system and can be fabricated from natural polymers (e.g., chitosan, collagen, hyaluronic acid) or synthetic polymers (e.g., PLGA, PVA) into hydrogels, fibrous meshes, or 3D-printed matrices [49] [52].
Mechanism of Action: Scaffolds are a quintessential non-targeted, local delivery platform. They are implanted or injected at the disease site (e.g., a tumor resection cavity, a wound, or a joint) to act as a reservoir for NAs, which are either free or pre-encapsulated in NPs [49] [52]. Their primary mechanism is the sustained, localized release of NAs, thereby protecting the payload from systemic degradation and minimizing off-target effects. This creates a high local concentration to efficiently transfect infiltrating or resident cells (e.g., immune cells, stem cells) within the scaffold microenvironment [49] [52].
Table 2: Key Characteristics and Experimental Performance of Biomaterial Scaffolds for NA Delivery.
| Scaffold Type | Common Materials | Key Advantages for NA Delivery | NA Release Kinetics (Experimental Data) | Key Outcomes (In Vivo Models) | Key Limitations |
|---|---|---|---|---|---|
| Natural Hydrogels | Chitosan, Hyaluronic Acid, Collagen | High biocompatibility, inherent bioactivity, injectable [49]. | Sustained release over 2-4 weeks [49]. | Enhanced bone regeneration in cranial defect models; improved wound healing in diabetic mice [49]. | Limited mechanical strength, batch-to-batch variability [49]. |
| Synthetic Hydrogels | Poly(vinyl alcohol), PEG | Tunable mechanical properties, controllable degradation, reproducible [49]. | Tunable from days to months via crosslinking density [49]. | Successful localized siRNA delivery for osteoarthritis treatment in rodent models [49]. | Often bio-inert, requires functionalization for cell adhesion [49]. |
| 3D-Printed Matrices | PLGA, PCL | Customizable architecture, spatial control over NA distribution [49]. | Multi-phasic release based on material composition and geometry [49]. | Spatially guided tissue regeneration in complex osteochondral defects [49]. | Complex fabrication, requires specialized equipment [49]. |
| Electrospun Fibers | PLGA, PCL, Chitosan | High surface area-to-volume ratio, can mimic ECM structure [49]. | Burst release initially, followed by sustained release for weeks [49]. | Effective in delivering plasmid DNA for skin tissue regeneration [49]. | Potential denaturation of NAs during electrospinning [49]. |
Nucleic Acid Nanostructures: Programmable and Modular Platforms
Overview: Nucleic acid nanostructures (NANs) are synthetic nanoscale objects engineered from DNA or RNA strands through the principle of programmable self-assembly [53] [54]. This includes structures like DNA origami, polyhedra, and RNA cubes.
Mechanism of Action: NANs represent the pinnacle of active targeting through molecular programming. Their structure itself can be designed to be the therapeutic agent (e.g., siRNA, ASO, or aptamer). They can be engineered with ultra-precision to display multiple targeting ligands (e.g., antibodies, folic acid) for enhanced specific binding to cell surfaces [53] [54]. Furthermore, they can be designed for stimuli-responsive conformational changes for controlled drug release [54].
Table 3: Key Characteristics and Experimental Performance of Nucleic Acid Nanostructures for NA Delivery.
| Structure Type | Description | Key Advantages for NA Delivery | Targeting Accuracy (Experimental Data) | Therapeutic Efficacy (In Vivo Models) | Key Limitations |
|---|---|---|---|---|---|
| DNA Nanostructures | DNA origami, tetrahedra, nanotubes | Atomistic precision, high biostability, predictable design [53] [54]. | >10-fold higher accumulation in target tumor tissue vs. non-targeted controls [54]. | Improved tumor growth inhibition in murine xenograft models with targeted siRNA delivery [54]. | Susceptibility to nuclease degradation, complex large-scale production [53] [54]. |
| RNA Nanostructures | RNA cubes, rings, polygons | Innate biological functions (e.g., gene silencing), can be non-immunogenic [53] [54]. | Specific delivery to cancer cells expressing target receptor [54]. | Effective gene silencing in targeted tissues with reduced off-target effects [53] [54]. | Lower thermodynamic stability than DNA, requires careful design to avoid misfolding [54]. |
Experimental Protocols for Key Evaluations
Protocol: Evaluating Targeted vs. Non-Targeted Delivery In Vivo
This protocol is designed to directly compare the biodistribution and efficacy of a NA payload delivered via a targeted versus a non-targeted system, such as a ligand-functionalized inorganic NP (targeted) versus a biomaterial scaffold implant (non-targeted, local).
- Material Preparation:
- Targeted System: Synthesize 50 nm gold nanoparticles. Conjugate Cy5-labeled siRNA against a luciferase reporter gene and an anti-EGFR antibody to the NP surface via PEG spacers [50].
- Non-Targeted System: Formulate a chitosan/hyaluronic acid hybrid hydrogel. Incorporate the same Cy5-labeled siRNA into the hydrogel matrix during cross-linking [49].
- Animal Model: Use BALB/c nude mice (n=6 per group) bearing subcutaneous EGFR-positive tumor xenografts stably expressing luciferase.
- Administration:
- Targeted Group: Inject the targeted Au-NP/siRNA system intravenously via the tail vein (siRNA dose: 1 mg/kg).
- Non-Targeted Group: Implant the siRNA-loaded hydrogel scaffold directly into the tumor mass.
- Control Group: Administer non-targeted Au-NPs (no anti-EGFR antibody) intravenously.
- Data Collection and Analysis:
- Biodistribution: At 24h and 48h post-administration, image mice using an in vivo imaging system (IVIS) to quantify Cy5 fluorescence in tumors and major organs. Calculate the tumor-to-liver signal ratio as a metric of targeting specificity [54] [50].
- Efficacy: Measure luciferase activity via bioluminescence imaging before treatment and daily for one week. Calculate percentage luciferase knockdown.
- Safety: Monitor mouse body weight and collect blood for liver enzyme (ALT, AST) analysis at the endpoint.
Protocol: Assessing Transfection Efficiency and Cytotoxicity In Vitro
This standard protocol evaluates the performance of NA delivery systems in cell culture.
- Cell Seeding: Seed HEK-293 or HeLa cells in a 96-well plate at a density of 10,000 cells per well and culture for 24h.
- Treatment:
- Prepare complexes of the delivery vehicle (e.g., inorganic NPs, lipoplexes) with a reporter plasmid (e.g., encoding GFP) at various weight ratios.
- Add the complexes to cells in serum-free medium. Include controls: cells only, naked plasmid DNA.
- Incubation and Analysis:
- After 4-6h, replace the medium with fresh complete medium.
- Transfection Efficiency: After 48h, analyze the cells using flow cytometry to determine the percentage of GFP-positive cells.
- Cytotoxicity: In parallel, perform an MTT assay. Incubate cells with MTT reagent for 4h, dissolve the formazan crystals, and measure absorbance at 570 nm. Calculate cell viability relative to untreated controls [50] [48].
Visualization of Signaling Pathways and Workflows
NA Delivery Pathways
Diagram Title: Targeted vs. Non-Targeted NA Delivery Pathways.
Experimental Workflow
Diagram Title: Key Experimental Workflow for NA Delivery Systems.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Materials for Nucleic Acid Delivery Research.
| Reagent/Material | Function/Description | Example Applications |
|---|---|---|
| Lipofectamine 3000 | A commercial lipid-based transfection reagent, often used as a positive control in vitro. | Transfection of plasmid DNA, mRNA, or siRNA into a wide range of mammalian cell lines [48]. |
| Polyethylenimine (PEI) | A cationic polymer that condenses NAs into polyplexes; a standard for high-efficiency transfection, despite cytotoxicity concerns. | Benchmarking the performance of new non-viral delivery vectors in vitro and in vivo [49]. |
| D-Luciferin | The substrate for firefly luciferase, used in bioluminescence imaging. | Monitoring reporter gene expression or tumor growth in small animal models [54]. |
| Cy5/Cy5.5 dye | A near-infrared fluorescent dye used for labeling. | Tracking the biodistribution and cellular uptake of NA complexes in live animal imaging (IVIS) and fluorescence microscopy [54]. |
| Fetal Bovine Serum (FBS) | Essential supplement for cell culture media. | Cell maintenance and proliferation; also used in stability tests to assess NA complex stability in physiological conditions [48]. |
| MTT Reagent | (3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide); used to assess cell viability and proliferation. | Quantifying the potential cytotoxicity of delivery vectors in cell cultures [50] [48]. |
The comparative analysis reveals that the choice between targeted and non-targeted strategies is context-dependent, dictated by the pathophysiology of the target disease.
- Inorganic Nanoparticles offer a versatile platform that can be engineered for both systemic targeted delivery and localized therapy. Their multifunctionality (e.g., combined imaging and therapy) is a significant advantage [50]. However, concerns regarding long-term toxicity and potential off-target accumulation, even with targeting ligands, remain hurdles for clinical translation [51] [50].
- Biomaterial Scaffolds excel as a non-targeted strategy for localized conditions. Their ability to provide a protected, sustained-release depot significantly enhances transfection efficiency within a defined anatomical site while minimizing systemic exposure and toxicity [49] [52]. Their limitation is their inherent lack of suitability for treating disseminated or systemic diseases.
- Nucleic Acid Nanostructures represent the cutting edge of targeted delivery, with unparalleled molecular precision and programmability [53] [54]. Their potential for multi-valent targeting and complex logic-gated operations is unmatched. Currently, challenges in scalable manufacturing and structural stability in biological fluids constrain their widespread application [53] [54].
In conclusion, there is no single "best" material class. The future of NA delivery likely lies in hybrid approaches that combine the strengths of these platforms. For instance, nucleic acid nanostructures could be used for their targeting precision, while inorganic NPs or biomaterial scaffolds could provide protective packaging and controlled release kinetics [49] [50]. The objective data provided in this guide serves as a foundation for researchers to make informed decisions and drive the next generation of innovations in this rapidly evolving field.
Overcoming Delivery Hurdles: Stability, Specificity, and Safety Optimization
Enhancing Stability and Reducing Immunogenicity through Chemical Modifications
The therapeutic application of nucleic acids—including messenger RNA (mRNA), small interfering RNA (siRNA), and antisense oligonucleotides (ASOs)—represents a revolutionary advance in treating genetic disorders, cancers, and infectious diseases. Unlike conventional small-molecule drugs that primarily target proteins, nucleic acid drugs (NADs) can achieve long-lasting or even curative effects by addressing underlying genetic causes through gene inhibition, addition, replacement, or editing [2]. However, a significant bottleneck hindering their clinical translation stems from their inherent physicochemical properties and susceptibility to immune recognition [55] [2].
When administered in vivo, unmodified nucleic acids face multiple critical barriers: they are rapidly degraded by nucleases in biological fluids, efficiently cleared by the kidneys, and poorly taken up by target cells due to their negative charge [6] [56]. Furthermore, the innate immune system recognizes foreign RNA through pattern recognition receptors (PRRs) like Toll-like receptors (TLRs) and retinoic acid-inducible gene I (RIG-I)-like receptors, triggering potent immune responses that can severely limit therapeutic efficacy and cause adverse effects [55]. Consequently, the field has prioritized the development of chemical modification strategies to enhance the stability of these molecules against degradation and reduce their immunogenicity, thereby making them viable as drugs [2]. This guide objectively compares the performance of various chemical modification approaches, providing a critical evaluation of their relative advantages and limitations within the broader context of targeted versus non-targeted nucleic acid delivery system research.
Classification and Mechanisms of Nucleic Acid Drugs
To understand the context for chemical modifications, it is essential to first classify nucleic acid therapeutics based on their mechanisms of action. These drugs can be broadly categorized into three groups [2]:
- Drugs that target nucleic acids to regulate protein expression: This category includes ASOs, siRNAs, microRNAs (miRNAs), and the CRISPR/Cas system. They function by promoting or inhibiting the translation of specific mRNAs or by performing precise gene editing on genomic DNA.
- Drugs that target proteins: The primary examples are aptamers, which are single-stranded oligonucleotides that fold into specific three-dimensional structures to bind target proteins with high affinity and specificity, functioning similarly to antibodies.
- Drugs that express proteins: This category is dominated by in vitro-transcribed (IVT) mRNA, which is delivered into cells to serve as a template for the production of therapeutic proteins.
The following diagram illustrates the fundamental mechanisms of action and intracellular sites for major nucleic acid drug classes.
Key Chemical Modification Strategies and Performance Comparison
Chemical modifications are strategically incorporated into various parts of nucleic acid molecules to enhance their drug-like properties. The table below provides a systematic comparison of the primary modification types, their locations within the nucleic acid structure, molecular mechanisms, and their distinct impacts on stability and immunogenicity.
Table 1: Performance Comparison of Key Chemical Modification Strategies for Nucleic Acid Drugs
| Modification Type | Location on Nucleic Acid | Molecular Mechanism | Impact on Stability | Impact on Immunogenicity | Key Trade-offs/Unintended Effects |
|---|---|---|---|---|---|
| Nucleoside Modifications (e.g., Pseudouridine (Ψ), N1-methylpseudouridine (m1Ψ)) [55] | Nucleobase within the RNA chain | Alters molecular structure to reduce recognition by immune sensors (PRRs) | Increases resistance to nuclease degradation | Significant reduction in TLR and RLR activation | m1Ψ may cause ribosomal frameshifting during translation, producing aberrant proteins [55] |
| Backbone Modifications (e.g., Phosphorothioate (PS)) [2] | Phosphate backbone between nucleotides | Increases binding to plasma proteins, prolonging circulation half-life | Dramatically improves nuclease resistance | Can reduce immune stimulation by altering physical properties | Non-specific protein binding can increase toxicity |
| 2'-Sugar Modifications (e.g., 2'-O-Methyl (2'-OMe), 2'-Fluoro (2'-F)) [57] | Ribose sugar moiety | Creates steric hindrance against nuclease attack | Greatly enhances metabolic stability in serum | Moderately reduces immunogenicity | Over-modification can impair efficacy (e.g., RISC loading for siRNA) |
| 5' Cap Modifications (e.g., CleanCap, ARCA) [55] | 5' end of mRNA | Mimics natural eukaryotic cap structure for efficient translation | Protects from 5' exonuclease degradation | Reduces detection by RIG-I and other decapping sensors | More complex and costly synthesis |
| Poly(A) Tail Modifications [55] | 3' end of mRNA | Engineered tail length and incorporation of modified nucleotides | Protects from 3' exonuclease-mediated decay | Minor indirect reduction by improving overall mRNA integrity | Optimal length must be balanced for translation vs. stability |
The strategic application of these modifications is crucial. For instance, the successful clinical deployment of COVID-19 mRNA vaccines from Pfizer-BioNTech and Moderna relied heavily on the incorporation of m1Ψ throughout the mRNA sequence, which was instrumental in dampening the innate immune response and enabling robust protein production [55]. Similarly, the first FDA-approved siRNA therapeutic, Patisiran (Onpattro), utilizes extensive 2'-OMe modifications to enhance its stability in circulation and within target cells [57] [2].
Experimental Protocols for Evaluating Modification Efficacy
To objectively compare the performance of different chemical modifications, researchers employ standardized experimental protocols. These methodologies assess critical parameters such as stability, immunogenicity, and translational efficiency.
In Vitro Serum Stability Assay
Objective: To quantitatively evaluate the resistance of modified nucleic acids to nuclease degradation in biological fluids [2].
Protocol:
- Preparation: Dilute the modified nucleic acid (e.g., siRNA or ASO) in human or fetal bovine serum (typically 50-90% serum concentration) and incubate at 37°C.
- Sampling: Withdraw aliquots at predetermined time points (e.g., 0, 1, 3, 6, 12, 24 hours).
- Termination: Halt degradation by adding proteinase K or denaturing the serum proteins with urea/SDS.
- Analysis: Separate intact nucleic acids from degraded fragments using denaturing polyacrylamide gel electrophoresis (PAGE) or capillary electrophoresis. Quantify the percentage of full-length product remaining using staining or fluorescence detection.
- Data Interpretation: Calculate the half-life (t½) of the nucleic acid by plotting the logarithm of the intact percentage versus time. Modified nucleic acids demonstrate significantly extended half-lives compared to their unmodified counterparts.
Immune Activation Profiling in Human Peripheral Blood Mononuclear Cells (PBMCs)
Objective: To measure the immunostimulatory potential of modified nucleic acids by quantifying cytokine secretion and immune marker expression [55].
Protocol:
- Cell Isolation: Isolate PBMCs from healthy human donors using density gradient centrifugation (e.g., Ficoll-Paque).
- Stimulation: Treat PBMCs with various formulations of modified nucleic acids (1-1000 nM range), using unmodified nucleic acids and known TLR agonists (e.g., LPS) as positive controls, and untreated cells as a negative control.
- Incubation: Culture cells for 6-24 hours in a 37°C, 5% CO₂ incubator.
- Cytokine Measurement: Collect cell culture supernatants and quantify key cytokines (e.g., IFN-α, IFN-β, TNF-α, IL-6) using enzyme-linked immunosorbent assays (ELISA) or multiplex bead-based arrays.
- Flow Cytometry: Analyze surface expression of co-stimulatory markers (e.g., CD80, CD86) on antigen-presenting cells (e.g., dendritic cells) using fluorochrome-conjugated antibodies and flow cytometry.
- Data Interpretation: Effective modifications (like m1Ψ) show a significant reduction (often >80-90%) in cytokine production compared to unmodified controls, indicating successful evasion of immune recognition.
The experimental workflow for evaluating modification efficacy typically follows a systematic progression from in vitro characterization to in vivo validation, as illustrated below.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The development and testing of chemically modified nucleic acids require specialized reagents and materials. The following table details key solutions used in this field.
Table 2: Essential Research Reagents for Nucleic Acid Modification Studies
| Reagent/Material | Function in Research | Specific Application Example |
|---|---|---|
| Modified Nucleotides (e.g., N1-methylpseudouridine-5'-triphosphate) [55] | Substrate for in vitro transcription (IVT) to produce modified mRNA | Direct incorporation into mRNA transcripts to reduce immunogenicity |
| Cap Analogs (e.g., CleanCap AG co-transcriptional capping reagent) [55] | Enables synthesis of properly capped mRNA in a single step | Production of translation-competent mRNA with superior 5' end integrity |
| Cationic Lipids & Lipid Nanoparticle (LNP) Components (e.g., ionizable lipids like MC3, SM-102) [58] | Formulates nucleic acids into nanoparticles for efficient cellular delivery | Encapsulation of siRNA or mRNA for in vitro and in vivo delivery studies |
| Pattern Recognition Receptor (PRR) Reporter Cell Lines (e.g., HEK293-TLR reporter cells) [55] | Mechanism-specific assessment of immune activation | Screening modifications for their ability to avoid detection by specific TLRs (e.g., TLR7/8) |
| Ribonuclease (RNase) Enzymes (e.g., RNase A, RNase T1) | In vitro tools to challenge nucleic acid stability under controlled conditions | Accelerated stability testing of modified versus unmodified RNA constructs |
Integration with Delivery Systems: Passive vs. Active Targeting
Chemical modifications work synergistically with delivery platforms to achieve therapeutic efficacy. The choice between passive and active targeting strategies significantly influences the design goals for chemical modifications.
Passive targeting relies on the natural biodistribution patterns of nanoparticles. It exploits physiological conditions, such as the Enhanced Permeability and Retention (EPR) effect in tumors, where leaky vasculature allows nanoparticles of specific sizes (typically 20-200 nm) to accumulate [58]. For passively targeted systems, chemical modifications primarily aim to enhance circulation time and structural integrity. This is often achieved through:
- PEGylation: Adding polyethylene glycol chains to the surface of nanoparticles or directly to oligonucleotides to reduce opsonization and clearance by the mononuclear phagocyte system (MPS) [58].
- Backbone stabilization: Incorporating phosphorothioate (PS) linkages or 2'-sugar modifications to increase resistance to nucleases during extended circulation [2].
Active targeting involves conjugating targeting ligands (e.g., antibodies, peptides, aptamers, or small molecules like GalNAc) to the nucleic acid or its carrier. These ligands bind specifically to receptors enriched on target cells. The GalNAc-siRNA conjugate platform is a prime example, where the GalNAc ligand directs the siRNA specifically to hepatocytes via the asialoglycoprotein receptor [57]. For such actively targeted constructs, which often do not require a complex nanoparticle for delivery, chemical modifications are crucial for:
- Stability in the extracellular matrix: Ensuring the oligonucleotide remains intact until it is internalized.
- Compatibility with the targeting ligand: Maintaining the ligand's binding affinity.
- Efficient intracellular activity: Once internalized, the modified oligonucleotide must still function within the correct subcellular compartment [2].
The pathway diagram below illustrates how chemical modifications and delivery strategies converge to overcome biological barriers and enable effective nucleic acid drug action.
Chemical modifications are indispensable for transforming therapeutic nucleic acids from fragile, immunogenic molecules into viable drugs. As this comparison demonstrates, different modification strategies—targeting the nucleobase, sugar, backbone, or ends of the nucleic acid—offer distinct profiles for enhancing stability and reducing immunogenicity. The optimal modification strategy is often application-dependent, requiring a careful balance between achieving sufficient stability and maintaining the biological activity of the drug.
Future directions in the field point toward the integration of artificial intelligence (AI) and machine learning to accelerate the design of novel modifications and delivery systems. AI algorithms can virtually screen millions of potential chemical structures to predict their properties, such as nuclease resistance, immunogenicity, and interaction with delivery carriers, thereby reducing the time and cost of experimental optimization [24] [59]. Furthermore, the emergence of DNA nanocarriers presents a promising alternative delivery platform that offers unprecedented control over the morphology and functionalization of nanoparticles, potentially enabling more precise targeting and reduced side effects [60].
As the field progresses, the synergy between advanced chemical modifications, smart delivery technologies, and computational design will undoubtedly expand the therapeutic landscape for nucleic acid drugs, bringing precision medicines for a wider range of diseases within reach.
The therapeutic potential of siRNA and mRNA to treat human disease by targeting disease-causing genes is immense, with over 15 FDA-approved RNA therapeutics already on the market [61]. However, a fundamental biological barrier severely limits their widespread application: endosomal escape. Unlike small molecule drugs that passively diffuse across cellular membranes, RNA therapeutics are too large, charged, and hydrophilic to cross the lipid bilayer and instead enter cells via endocytosis [61]. Once internalized, they become trapped within membrane-bound endosomes, with 99% of RNA therapeutics failing to reach the cytosol—the site of action for siRNA and mRNA [61] [62]. This results in a dramatic efficiency loss, with quantitative studies revealing that only 1%-2% of GalNAc-ASO conjugates and a mere 0.3% of GalNAc-siRNA escape endosomes in hepatocytes in vivo [61]. Consequently, overcoming the endosomal escape problem represents the rate-limiting step for enabling the broad application of RNA therapeutics to extra-hepatic diseases [61] [62]. This guide systematically compares the leading technological strategies aimed at solving this critical delivery challenge.
Quantifying the Endosomal Escape Challenge
The inefficiency of endosomal escape is quantifiable across different delivery systems. The following table summarizes key experimental measurements that highlight the scope of the problem.
Table 1: Quantitative Measurements of Endosomal Escape Efficiency
| Delivery System | Cargo | Escape Efficiency | Measurement Technique | Reference |
|---|---|---|---|---|
| GalNAc-ASO Conjugates (in hepatocytes in vivo) | ASO | 1% - 2% | Quantitative NanoSIMS Microscopy | [61] |
| GalNAc-siRNA Conjugates (in hepatocytes in vivo) | siRNA | ~0.3% at any given time | Experimental quantification (Alnylam) | [61] |
| Commercially Available LNPs (siRNA) | siRNA | 1% - 2% of encapsulated siRNA | Not Specified | [62] |
| GFP without EEPs (in HEK293 cells) | Protein (GFP) | ~2% | Split Luciferase Endosomal Escape Quantification (SLEEQ) | [63] |
| GFP without EEPs (in HeLa cells) | Protein (GFP) | ~7% | Split Luciferase Endosomal Escape Quantification (SLEEQ) | [63] |
| Cationic TAT Peptide | Various | ~1% | Quantitative Assays | [61] |
The stark reality revealed by this data is that even successful, clinically approved systems operate at remarkably low efficiencies. The minimal number of cytoplasmic molecules required for activity is fortunately low: maximal siRNA activity requires only ~2000 cytoplasmic molecules, while ASOs require ~50,000 [61]. This low threshold enables functionality despite inefficient escape.
Comparative Analysis of Endosomal Escape Strategies
Multiple strategies have been developed to enhance endosomal escape, each with distinct mechanisms, advantages, and limitations. The following table provides a structured comparison of the leading approaches.
Table 2: Comparison of Key Endosomal Escape Strategies
| Strategy | Mechanism of Action | Key Example(s) | Therapeutic Cargo Compatibility | Efficiency & Key Findings | Toxicity Concerns |
|---|---|---|---|---|---|
| Ionizable Lipid NPs (LNPs) | Protonation in acidic endosomes promotes phase transition and membrane disruption [62] [15]. | DLin-MC3-DMA, SM-102, ALC-0315 [62]. | siRNA, mRNA | Only 1-2% of siRNA is released from endosomes; induces galectin-9+ membrane damage [62] [15]. | Reduced vs. cationic lipids; "PEG dilemma" can reduce uptake/escape [62]. |
| Cationic Lipids/ Polymers | Electrostatic interaction with anionic endosomal lipids (e.g., BMP, PS), causing membrane disruption or fusion [64]. | Lipofectamine (cationic lipids), Polyethylenimine (PEI) [64]. | siRNA, mRNA, pDNA | PEI's "proton sponge" effect is debated; overall efficiency is highly variable [64]. | High; can cause membrane disruption leading to necrosis or apoptosis [62] [64]. |
| Endosomal Escape Peptides (EEPs) | Membrane disruption via carpet mechanism or pore formation [61] [64]. | TAT peptide (from HIV), INF7 (from influenza HA2) [61] [64]. | Neutral backbones (PMO, PNA); limited for anionic siRNA/ASO [61]. | Cationic peptides (e.g., TAT) show ~1% escape; PPMOs show 18x activity vs. bare PMO in trials [61]. | Cationic peptides can bind blood cells and stimulate immune responses; balancing charge is critical [61]. |
| Endolytic Small Molecules | Protonation and accumulation in endosomes, leading to osmotic swelling or membrane rupture. | Chloroquine [61]. | Various | Enhances escape but only at cytotoxic concentrations [61]. | High, class-effect feature; non-specific rupture of many endosomes [61]. |
| Extracellular Vesicles (EVs) | Innate, natural mechanisms for endosomal escape, potentially involving membrane fusion [62]. | Natural exosomes. | Proteins, nucleic acids | >10-fold higher EE performance than some commercial LNPs [62]. | Naturally low immunogenicity. |
Key Insights from Comparative Analysis
- The Toxicity-Efficiency Trade-off: A central theme is the direct correlation between escape efficiency and cytotoxicity. Strategies like chloroquine and persistent cationic lipids cause efficient escape through non-specific membrane rupture, which also triggers cell death pathways [61] [64]. The most successful technologies, such as ionizable LNPs, are designed to be active only within the acidic endosomal environment, thereby mitigating off-target toxicity [62].
- Cargo Compatibility Dictates Choice: The choice of strategy is often constrained by the cargo. For instance, cationic peptides are highly effective for neutral phosphorodiamidate morpholino oligomers (PPMOs) but form inactive aggregates with anionic siRNAs and ASOs [61].
- Inspiration from Nature: Extracellular vesicles (EVs) demonstrate that highly efficient endosomal escape is biologically achievable. Their innate mechanisms, which are more than 10-fold higher than some commercial LNPs, provide a blueprint for next-generation synthetic delivery systems [62].
Advanced Experimental Models and Protocols
Understanding and improving endosomal escape requires sophisticated, quantitative experimental models.
The SLEEQ Assay for Quantifying Cytosolic Delivery
The Split Luciferase Endosomal Escape Quantification (SLEEQ) assay was developed to directly, sensitively, and quantitatively measure cytosolic delivery [63].
Detailed Protocol:
- Cell Line Engineering: Engineer cell lines (e.g., HEK293, HeLa) to stably express the large subunit of NanoLuciferase (LgBiT) fused to β-actin (LgBiT-SNAP-actin, LSA), ensuring its localization and retention in the cytosol [63].
- Cargo Design: Fuse the protein or peptide cargo of interest to the small, high-affinity HiBiT peptide (1.3 kDa) [63].
- Experimental Workflow: Incubate the HiBiT-tagged cargo with the LSA-expressing cells. Upon endocytosis and subsequent escape into the cytosol, HiBiT and LgBiT bind to form a functional luciferase enzyme [63].
- Quantification: Add the luciferase substrate, and the resulting luminescence directly correlates with the amount of cargo that has reached the cytosol. This assay can detect picomolar concentrations of cytosolic protein, making it four orders of magnitude more sensitive than split-GFP systems [63].
Key Application: Using SLEEQ, researchers demonstrated that positively charged cell-penetrating peptides (CPPs) increase total cytosolic delivery primarily by enhancing non-specific cell membrane association and uptake, not by increasing the efficiency of endosomal escape itself [63].
Live-Cell Imaging of LNP-Mediated Escape
Recent research employing live-cell and super-resolution microscopy has provided unprecedented insight into the fate of LNPs inside cells [15].
Detailed Protocol:
- Fluorescent Labeling: Formulate LNPs containing fluorescently labeled RNA (e.g., with Cy5 or AlexaFluor 647) and/or a tagged ionizable lipid (e.g., BODIPY-MC3) [15].
- Membrane Damage Sensing: Transfect cells to express a fluorescently tagged damage sensor protein, such as galectin-9, which recruits to sites of endosomal membrane disruption [15].
- Imaging and Analysis: Use live-cell microscopy to track the co-localization of LNP fluorescence and galectin-9 recruitment in real-time. Single vesicle tracking and fluorescence quantification can reveal the heterogeneity of RNA content and the moment of membrane damage [15].
Key Findings from this Model:
- Segregation of Payload: The RNA payload and ionizable lipid of LNPs can segregate during endosomal sorting, both within single endosomes and across different compartments. Many endosomes that show galectin-9-positive membrane damage contain no detectable RNA, particularly for mRNA-LNPs [15].
- Inefficient Release from Damaged Endosomes: Even when LNPs in galectin-9-positive endosomes contain RNA, only a small fraction of the total endosomal RNA cargo is released into the cytosol upon membrane damage [15].
The following diagram illustrates the complex intracellular journey and multiple barriers faced by lipid nanoparticles, as revealed by these advanced imaging techniques.
The Scientist's Toolkit: Key Research Reagents
The following table lists essential reagents and their functions for studying endosomal escape.
Table 3: Essential Reagents for Endosomal Escape Research
| Reagent / Material | Function in Research | Key Application Example |
|---|---|---|
| Ionizable Lipids (e.g., DLin-MC3-DMA, SM-102) | Core component of LNPs; protonates in endosomes to induce membrane disruption [62] [15]. | Formulating clinically relevant siRNA/mRNA LNPs; studying structure-activity relationships [62]. |
| Helper Lipids (e.g., DOPE, DSPC) | Modulate LNP fusogenicity and stability; DOPE promotes inverted hexagonal phase conducive to fusion [65] [64]. | Optimizing LNP composition for different RNA cargos and target tissues [65]. |
| PEGylated Lipids | Confers stealth properties, reduces aggregation, but can inhibit uptake/escape (the "PEG dilemma") [62]. | Balancing LNP stability and circulation time against efficient cellular uptake and endosomal escape [62]. |
| Cationic Peptides (e.g., TAT, arginine-rich peptides) | Enhance cellular uptake and can promote endosomal escape via membrane interaction [61] [64]. | Delivery of neutral oligonucleotides (e.g., PPMOs); studying mechanisms of CPP activity [61] [63]. |
| Galectin-9 Fluorescent Protein Fusions | A sensitive biosensor for detecting endosomal membrane damage in live cells [15]. | Visualizing and quantifying LNP-induced endosomal rupture as a precursor to cytosolic release [15]. |
| HiBiT Peptide Tag (1.3 kDa) | Small subunit for split luciferase; fused to cargo of interest to quantify cytosolic delivery [63]. | Serving as a cargo in the SLEEQ assay for direct, quantitative measurement of endosomal escape efficiency [63]. |
Solving the endosomal escape problem is the pivotal challenge limiting the full realization of RNA therapeutics. Current strategies, particularly ionizable LNPs, have enabled groundbreaking clinical successes but operate at remarkably low efficiencies (1-2%). Advanced models like the SLEEQ assay and live-cell imaging of galectin-recruitment reveal that the intracellular journey is fraught with multiple barriers, including payload segregation and inefficient release from damaged endosomes. The future of the field lies in leveraging these sophisticated models to rationally design next-generation delivery systems, perhaps by mimicking the superior efficiency of natural extracellular vesicles or by engineering novel ionizable lipids and peptides that maximize cytosolic release while minimizing toxicity. Overcoming this single biological barrier will unlock the vast potential of siRNA, mRNA, and other nucleic acid therapeutics to treat a wide array of human diseases.
The therapeutic application of nucleic acids, including small interfering RNA (siRNA), antisense oligonucleotides (ASOs), and CRISPR-Cas9 systems, represents a paradigm shift in treating genetically-linked disorders. Unlike traditional small-molecule drugs that primarily target proteins, nucleic acid therapeutics can modulate previously "undruggable" targets at the genomic level, offering potential for long-lasting or even curative effects [1]. However, this revolutionary potential is constrained by a significant challenge: balancing therapeutic efficacy with safety concerns, particularly off-target effects and associated toxicity. These unintended consequences can arise from hybridization to sequences similar but not identical to the target, hybridization-independent sequence effects, or sequence-independent interactions [66]. As the field progresses toward clinical applications, developing strategies to mitigate these effects while maintaining biocompatibility has become a critical focus of research and development, especially within the context of comparing targeted versus non-targeted delivery approaches [67] [6].
Understanding Off-Target Effects: Mechanisms and Consequences
Off-target effects in nucleic acid therapeutics manifest through several distinct mechanisms, each with different implications for efficacy and safety.
Mechanisms of Action and Associated Off-Target Risks
Table 1: Mechanisms and Off-Target Risks of Nucleic Acid Therapeutics
| Therapeutic Class | Primary Mechanism of Action | Primary Target Site | Common Off-Target Mechanisms |
|---|---|---|---|
| Antisense Oligonucleotides (ASOs) | RNase H1-dependent cleavage or steric hindrance of target RNA [1] | Nucleus/Cytosol [6] | Hybridization to non-identical sequences; unintended protein binding [1] [66] |
| siRNA | RNA interference (RNAi); guides RISC to cleave complementary mRNA [1] | Cytosol [6] | Imperfect complementarity with non-target mRNAs; seed region interactions [66] |
| CRISPR-Cas9 | DNA cleavage via guide RNA-directed Cas9 nuclease [68] | Nucleus | Tolerance of mismatches between sgRNA and DNA; non-canonical PAM recognition [68] [69] |
| Aptamers | Target recognition and binding via specific 3D structures [1] | Extracellular/Various | Binding to structurally similar but unintended targets [1] |
For oligonucleotide therapies like ASOs and siRNAs, off-target toxicity remains a critical safety concern that may hinder clinical translation [66]. These effects can result in diminished transcript levels, decreased translation rates, or anomalous splicing, employing the same molecular pathways as the desired on-target effects. The consequences are particularly concerning for CRISPR-Cas9 systems, where off-target DNA cleavage can introduce permanent genomic modifications at non-targeted loci, raising substantial genotoxicity concerns [69].
Strategic Approaches to Mitigate Off-Target Effects
Nucleic Acid Design and Engineering
Optimizing the design of the therapeutic nucleic acid itself represents the first line of defense against off-target effects.
For CRISPR-Cas9 Systems:
- sgRNA Truncation: Truncating the 5'-end of the sgRNA to 17-18 nucleotides increases the sensitivity to mismatches, reducing off-target cleavage without sacrificing on-target efficiency [68].
- sgRNA Modification: Incorporating two guanine nucleotides at the 5' end of the sgRNA or using chemically modified bridged/locked nucleic acids in the central region can significantly lower off-target rates [68].
- High-Fidelity Cas Variants: Engineering Cas9 endonucleases with altered amino acid residues to reduce non-specific DNA binding enhances specificity [68].
For Oligonucleotide Therapies (ASO/siRNA):
- Chemical Modification: Incorporating chemically modified nucleotides (e.g., phosphorothioate linkages, 2'-O-methyl, 2'-fluoro) increases binding affinity and nuclease resistance, allowing for more specific targeting [6] [1].
- Computational Design: Using sophisticated algorithms to select optimal target sequences and predict potential off-target binding sites during the design phase [66].
Delivery System Engineering
The choice of delivery system critically influences both the efficacy and specificity of nucleic acid therapeutics by determining their pharmacokinetics, biodistribution, and cellular uptake.
Table 2: Comparison of Nucleic Acid Delivery Systems
| Delivery System | Key Components | Targeting Strategy | Advantages for Specificity | Limitations |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Ionizable lipids, phospholipids, cholesterol, PEG-lipids [70] | Passive targeting (EPR effect); ligand conjugation for active targeting [70] | Protects cargo; can be targeted to specific tissues [1] | Potential immunogenicity; variable encapsulation efficiency [67] |
| Polymeric Nanoparticles | PEI, PLL, PLGA, chitosan [6] [71] | Incorporation of targeting ligands (peptides, antibodies, aptamers) [6] | Controlled release; tunable properties; enhanced endosomal escape [6] [71] | Complexity in manufacturing; potential polymer-associated toxicity [67] |
| Virus-Inspired Non-Viral Systems | Sequence-defined peptides with functional domains [6] | Mimicking viral tropism with synthetic sequences [6] | High transfection efficiency; dynamic responsiveness to biological environment [6] | Complex synthesis; scalability challenges [6] |
| "1+1" Type (Separate Encapsulation) | Individual nanocarriers for different drugs [67] | Independent targeting and release kinetics [67] | Independent controllable release; avoids drug-drug interactions [67] | Complex pharmacokinetics; challenging to coordinate delivery [67] |
| "2 in 1" Type (Co-encapsulation) | Single carrier for multiple therapeutic agents [67] | Unified targeting approach | Simplified pharmacokinetics; ensures delivery to same cells [67] | Formulation challenges; fixed drug ratio [67] |
Targeted delivery systems enhance biocompatibility by concentrating the therapeutic effect at the desired site while minimizing exposure to non-target tissues. This is achieved through both passive targeting (leveraging the Enhanced Permeability and Retention (EPR) effect in tumors) and active targeting (using ligands that bind to receptors specifically expressed on target cells) [70] [6]. The development of sequence-defined carriers represents a particularly advanced approach, where functional building blocks—including shielding domains, targeting ligands, hydrophobic domains, and endosomal buffering agents—are incorporated to overcome pharmacological barriers while maximizing specificity [6].
Experimental Protocols for Assessing Off-Target Effects
Protocol 1: Comprehensive Off-Target Screening for CRISPR-Cas9
Objective: To identify and quantify off-target editing events in CRISPR-Cas9 mediated genome editing. Materials: High-fidelity Cas9 nuclease, designed sgRNAs, target cells, PCR reagents, NGS library preparation kit, bioinformatics analysis tools. Methodology:
- In Silico Prediction: Utilize computational tools (e.g., Cas-OFFinder) to predict potential off-target sites based on sequence similarity to the target locus [68].
- Cell Transfection: Deliver CRISPR-Cas9 components (Cas9 + sgRNA) into target cells using appropriate methods (e.g., electroporation, lipid nanoparticles).
- Genomic DNA Extraction: Harvest cells 72 hours post-transfection and extract genomic DNA.
- Targeted Locus Amplification: Perform PCR amplification of both on-target and predicted off-target sites.
- Next-Generation Sequencing (NGS): Prepare sequencing libraries and perform deep sequencing of amplified regions.
- Bioinformatic Analysis: Align sequences to reference genome and quantify insertion/deletion mutations (indels) at each site using specialized tools (e.g., CRISPResso2) [69]. Interpretation: Compare indel frequencies at off-target sites to both on-target sites and negative controls. Sites with significantly elevated indel frequencies represent confirmed off-target events.
Protocol 2: Profiling Oligonucleotide Therapeutics Hybridization-Dependent Off-Targets
Objective: To identify unintended transcript silencing by siRNA or ASO therapeutics. Materials: Modified oligonucleotides, target cells, RNA extraction kit, microarray/NGS platforms, transfection reagent. Methodology:
- Oligonucleotide Design: Include both fully complementary and mismatch-containing control sequences.
- Cell Treatment: Transfert cells with therapeutic oligonucleotides at relevant concentrations.
- RNA Extraction: Isolate total RNA 48 hours post-treatment.
- Transcriptome Analysis: Perform global transcriptome profiling using microarray or RNA-seq.
- Differential Expression: Identify significantly downregulated transcripts (e.g., >2-fold reduction) in treated versus control cells.
- Sequence Alignment: Bioinformatically analyze downregulated transcripts for partial complementarity to the oligonucleotide sequence, particularly in the "seed" region [66]. Interpretation: Transcripts showing significant downregulation with partial complementarity to the therapeutic oligonucleotide represent potential off-target effects requiring further validation.
Visualization of Key Concepts
Strategic Framework for Mitigating Off-Target Effects
Diagram 1: A comprehensive framework showing the multi-faceted approach required to mitigate off-target effects in nucleic acid therapeutics, encompassing molecular design, delivery engineering, and rigorous screening.
Nucleic Acid Delivery and Intracellular Trafficking
Diagram 2: The intracellular journey of nucleic acid therapeutics, highlighting critical decision points where proper trafficking leads to on-target effects versus misdirection that causes off-target effects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Nucleic Acid Therapeutic Development
| Reagent Category | Specific Examples | Function in Research | Role in Mitigating Off-Target Effects |
|---|---|---|---|
| Chemically Modified Nucleotides | 2'-O-methyl, 2'-fluoro, phosphorothioate, bridged/locked nucleic acids [68] [1] | Enhance stability, binding affinity, and nuclease resistance of oligonucleotides | Reduces non-specific protein binding; increases target specificity [1] |
| Sequence-Defined Carriers | Cationic peptides (e.g., HK peptides), PAMAM dendrimers, precise polymer structures [6] | Self-assembling delivery systems with defined functional domains | Enable targeted delivery; enhance endosomal escape with reduced toxicity [6] |
| Lipid Nanoparticles (LNPs) | Ionizable lipids (DLin-MC3-DMA), PEG-lipids, cholesterol [70] [1] | Formulation vehicle for nucleic acid encapsulation and delivery | Protect cargo; enable tissue-specific targeting via surface modification [70] |
| Targeting Ligands | Folate, transferrin, aptamers, cell-penetrating peptides, antibodies [70] [6] | Surface functionalization of delivery systems | Direct therapeutics to specific cell types; reduce off-target exposure [6] |
| Endosomal Escape Agents | Histidine-rich peptides, chloroquine, pH-sensitive polymers [6] | Enhance endosomal disruption and cytosolic delivery | Improve bioavailability at target site; reduce dosage requirements [6] |
| Bioinformatic Tools | sgRNA design algorithms, off-target prediction software, transcriptome analysis tools [68] [66] | Computational prediction and analysis of off-target effects | Enable proactive design of specific therapeutics; comprehensive off-target screening [68] [66] |
Achieving the delicate balance between therapeutic efficacy and biocompatibility in nucleic acid therapeutics requires a multi-pronged approach that addresses off-target effects at multiple levels. Strategic nucleic acid design through chemical modifications and computational optimization, combined with advanced delivery systems that maximize target tissue accumulation and cellular uptake, provides a powerful framework for enhancing specificity. The critical importance of comprehensive screening protocols, including both in silico prediction and experimental validation, cannot be overstated in identifying and quantifying off-target events. As the field progresses, the integration of these strategies—molecular design, delivery engineering, and rigorous safety assessment—will be essential for translating the enormous potential of nucleic acid therapeutics into safe, effective treatments for a wide range of genetically-linked diseases. The continued development of increasingly sophisticated reagents and methodologies, as outlined in this comparison, will further enable researchers to navigate the critical challenge of balancing efficacy with biocompatibility.
This guide compares the performance of targeted versus non-targeted drug delivery systems for nucleic acid drugs (NADs), focusing on their ability to improve pharmacokinetic profiles through prolonged circulation and controlled release.
Nucleic acid drugs (NADs), including DNA, RNA, and synthetic oligonucleotides, represent a promising new generation of therapeutics with the potential to achieve long-lasting efficacy through gene repression, replacement, and editing [2]. However, their clinical application faces significant pharmacokinetic challenges that limit their therapeutic potential. As negatively charged biological macromolecules, NADs struggle to cross cellular membranes and are easily degraded by endogenous nucleases in plasma and tissues, resulting in low stability and short half-lives [2]. Furthermore, the small fraction that successfully enters cells often becomes trapped in endosomes and degraded by lysosomes, considerably limiting their bioavailability and therapeutic effects [2].
To address these challenges, two primary strategies have emerged: structural modification of nucleic acids and development of advanced delivery systems [2]. This guide focuses on the latter approach, specifically comparing how targeted and non-targeted delivery systems influence key pharmacokinetic parameters including circulation time, tissue accumulation, cellular uptake, and ultimately, therapeutic efficacy.
Comparison of Delivery System Performance
The table below summarizes the key performance characteristics of major nucleic acid delivery systems, highlighting the critical differences between targeted and non-targeted approaches.
Table 1: Performance Comparison of Nucleic Acid Drug Delivery Systems
| Delivery System | Targeting Mechanism | Transfer Efficiency | Circulation Half-Life | Key Applications | Major Limitations |
|---|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Passive (EPR effect) | Moderate to High | Short to Moderate | siRNA, mRNA vaccines | Reactogenicity, predominant liver accumulation, complex composition [2] |
| GalNAc-Conjugates | Active (ASGPR receptor on hepatocytes) | High | Moderate | Liver-specific therapies (e.g., siRNAs) | Limited to liver applications, requires chemical conjugation expertise [2] |
| Viral Vectors | Natural tropism + engineering | Very High | Long-lasting expression | Gene replacement therapy | Immunogenicity, insertional mutagenesis, limited DNA cargo size [2] |
| Cell-Penetrating Peptides | Enhanced cellular uptake | Variable | Short to Moderate | Various oligonucleotides | Low specificity, potential toxicity at high doses [2] |
| Polymer Complexes | Passive + some active targeting | Moderate | Variable | DNA, oligonucleotides | Potential cytotoxicity, heterogeneity in complex size [2] |
| Cell-Mediated Systems | Innate cellular tropism | Under investigation | Extended (days) | Emerging for targeted delivery | Complex manufacturing, drug release control challenges [72] |
Experimental Protocols for Evaluating Delivery Systems
In Vivo Pharmacokinetic Profiling Protocol
Objective: Quantify circulation time, tissue distribution, and clearance kinetics of nucleic acid formulations.
Materials:
- Radiolabeled ([³²P] or [³H]) or fluorescently-labeled (Cy5, Cy7) nucleic acids
- Test delivery formulations (LNPs, conjugates, etc.)
- Animal models (typically mice or rats)
- Imaging systems (IVIS for fluorescence, SPECT/CT for radiotracers)
- PCR equipment for quantitative biodistribution analysis
Methodology:
- Dose Administration: Administer nucleic acid formulations intravenously at standardized doses (e.g., 1-5 mg/kg nucleic acid).
- Blood Sampling: Collect serial blood samples at predetermined time points (e.g., 5 min, 30 min, 2 h, 8 h, 24 h, 48 h, 72 h post-injection).
- Tissue Collection: Euthanize animals at designated time points and harvest tissues of interest (liver, spleen, kidney, lung, tumor).
- Sample Processing:
- For radioactive labels: homogenize tissues and measure radioactivity using a scintillation counter.
- For fluorescent labels: image tissues ex vivo and quantify fluorescence intensity.
- For qPCR-based quantification: extract total RNA/DNA from tissues and use specific primers to quantify nucleic acid payload.
- Data Analysis: Calculate pharmacokinetic parameters including half-life (t₁/₂), area under the curve (AUC), clearance (CL), and volume of distribution (Vd) using non-compartmental analysis.
Key Measurements:
- Plasma concentration-time profiles
- Tissue accumulation ratios (target vs. non-target tissues)
- Elimination rate constants
- Bioavailability compared to free nucleic acid controls
Endosomal Escape Efficiency Assay
Objective: Quantify the ability of delivery systems to facilitate endosomal escape, a critical bottleneck for nucleic acid activity.
Materials:
- Cells with stable expression of GFP-tagged endosomal markers (e.g., Rab5-GFP, Rab7-GFP)
- Fluorescently-labeled nucleic acids (e.g., Cy5-siRNA)
- Test delivery formulations
- Confocal microscopy system with live-cell imaging capability
- Endosomolytic agents (e.g., chloroquine) as positive controls
Methodology:
- Cell Seeding: Plate cells in glass-bottom dishes 24 hours before treatment.
- Treatment: Apply nucleic acid formulations at predetermined concentrations.
- Live-Cell Imaging: Capture time-lapse images over 2-24 hours using confocal microscopy.
- Image Analysis:
- Quantify co-localization of nucleic acid signal with endosomal markers.
- Calculate endosomal escape efficiency as the decrease in co-localization over time.
- Measure time to first appearance of nucleic acids in cytoplasm.
- Functional Correlation: Correlate escape efficiency with gene silencing or protein expression data.
Key Measurements:
- Percentage of cytosolic vs. endosomal nucleic acids at multiple time points
- Time to maximal endosomal escape
- Correlation between escape efficiency and functional activity
Key Research Reagent Solutions
Successful evaluation of nucleic acid delivery systems requires specialized reagents and materials. The table below outlines essential research tools for pharmacokinetic optimization studies.
Table 2: Essential Research Reagents for Delivery System Evaluation
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Tracking Labels | Cy5/Cy7 dyes, [³²P] isotopes, FAM/Biotin | Biodistribution studies | Enable visualization and quantification of nucleic acid location and concentration [2] |
| Chemical Modification Reagents | 2'-O-methyl, 2'-fluoro, phosphorothioate analogs | Stability enhancement | Improve nuclease resistance, reduce immunogenicity, extend half-life [2] |
| Targeting Ligands | GalNAc, antibodies, peptides, aptamers | Active targeting | Enable receptor-specific binding and cellular uptake [2] [10] |
| Lipid Components | Cationic lipids, PEG-lipids, phospholipids | Nanoparticle formulation | Encapsulate nucleic acids, facilitate cellular uptake, modify surface properties [2] |
| Endosomal Escape Markers | Rab-GFP constructs, Lysotracker dyes | Mechanism evaluation | Monitor intracellular trafficking and endosomal release efficiency [2] |
| Polymer Carriers | PEI, PLGA, chitosan | Polyplex formation | Condense nucleic acids, provide controlled release properties [2] |
Performance Analysis of Targeted vs. Non-Targeted Systems
Circulation Time and Stability
Targeted delivery systems, particularly those incorporating specific ligands like GalNAc, demonstrate superior pharmacokinetic profiles compared to non-targeted approaches. The intentional design of these systems focuses on overcoming the inherent limitations of nucleic acids, including rapid clearance and nuclease degradation [2].
Chemical modifications such as 2'-O-methyl, 2'-fluoro, and phosphorothioate backbone alterations significantly enhance nuclease resistance and prolong circulation half-life [2]. When these modifications are combined with targeted delivery vehicles, the synergistic effects can substantially improve bioavailability. For instance, GalNAc-conjugated siRNAs achieve therapeutic effects at substantially lower doses than non-targeted approaches due to their efficient receptor-mediated uptake into hepatocytes [2].
Non-targeted systems, particularly lipid nanoparticles, rely on the enhanced permeability and retention (EPR) effect for passive accumulation in tissues with leaky vasculature, such as tumors [73]. However, this passive targeting mechanism is heterogeneous and varies significantly between patients and tumor types [72]. Furthermore, the EPR effect is minimal in hypoxic tumor regions due to poor angiogenesis, limiting the effectiveness of non-targeted systems in these critical areas [72].
Tissue Specificity and Cellular Uptake
Active targeting strategies dramatically improve tissue specificity and cellular uptake efficiency compared to non-targeted approaches. The GalNAc-siRNA conjugate platform exemplifies this advantage, leveraging the asialoglycoprotein receptor (ASGPR) highly expressed on hepatocytes for efficient liver-specific delivery [2].
Emerging cell-mediated delivery systems represent a promising frontier for targeted delivery. Certain circulating cells, including leukocytes and stem cells, possess innate disease-sensing and homing capabilities that can be harnessed for precise drug delivery [72]. Leukocytes naturally cross biological barriers like the blood-brain barrier, enabling access to challenging targets such as brain tumors [72]. Similarly, stem cells exhibit natural tropism toward injured tissues and organs, providing a potential vehicle for site-specific nucleic acid delivery [72].
Non-targeted systems face significant limitations in tissue specificity. For example, conventional lipid nanoparticles predominantly accumulate in the liver and spleen regardless of the therapeutic target, limiting their application for extra-hepatic diseases [2]. This non-specific distribution not only reduces therapeutic efficacy at the target site but also increases the risk of off-target effects and toxicity in non-target tissues.
The strategic optimization of pharmacokinetic properties through advanced delivery systems is paramount for realizing the full therapeutic potential of nucleic acid drugs. Targeted delivery approaches, particularly ligand-conjugated systems, demonstrate clear advantages over non-targeted methods in terms of tissue specificity, cellular uptake efficiency, and therapeutic index. However, significant challenges remain, including the need for delivery solutions beyond the liver, more efficient endosomal escape mechanisms, and improved manufacturing scalability.
Future directions in the field should focus on developing novel targeting ligands for extra-hepatic tissues, optimizing controlled release technologies to further extend circulation half-lives, and addressing translational challenges such as manufacturing complexity and regulatory requirements. As these delivery platforms continue to evolve, they will undoubtedly expand the therapeutic landscape for nucleic acid drugs across a broader range of diseases and patient populations.
Clinical Translation and Comparative Analysis of Delivery Efficacy
Nucleic acid drugs (NADs) represent a revolutionary class of therapeutics capable of treating diseases at their genetic roots by silencing, editing, or replacing faulty genes. [2] This field has evolved from foundational molecular biology discoveries to clinical reality, with the first FDA-approved siRNA drug, patisiran, marking a pivotal milestone in 2018. [2] The central challenge for this class of therapeutics remains effective delivery—overcoming inherent instability, achieving targeted tissue distribution, and ensuring intracellular delivery to specific subcellular compartments. [2]
The clinical success of nucleic acid drugs is inextricably linked to their delivery systems, which can be broadly categorized into targeted and non-targeted approaches. This guide provides a systematic comparison of approved nucleic acid drugs, focusing on their delivery strategies, experimental methodologies for evaluation, and resulting clinical outcomes, framed within the broader thesis of evaluating targeted versus non-targeted delivery systems.
Approved Nucleic Acid Drugs and Their Delivery Platforms
Classification and Mechanisms of Action
NADs approved for clinical use primarily function through several distinct mechanisms, which directly influence their delivery requirements:
- RNA-targeting Drugs: This category includes antisense oligonucleotides (ASOs) and small interfering RNAs (siRNAs) that selectively silence gene expression. ASOs operate via RNase H-mediated degradation of complementary mRNA or through steric blockage of translation, while siRNAs utilize the RNA interference (RNAi) pathway for highly specific gene silencing. [2]
- Protein-targeting Drugs: Aptamers, which are single-stranded oligonucleotides, fall into this category. They function similarly to antibodies by folding into specific three-dimensional structures that enable direct and selective binding to target proteins. [2]
- Protein-expression Drugs: This category includes in vitro-transcribed messenger RNA (mRNA) that enables in vivo production of therapeutic proteins. The clinical validation of this approach came prominently from mRNA vaccines for COVID-19. [2]
Approved Drugs and Delivery Strategies
The table below summarizes key approved nucleic acid drugs, their delivery technologies, and clinical outcomes, illustrating the spectrum from non-targeted to actively targeted systems.
Table 1: Approved Nucleic Acid Drugs: Delivery Strategies and Clinical Outcomes
| Drug (Brand Name) | Nucleic Acid Type | Target / Indication | Delivery Strategy | Targeting Approach | Key Clinical Outcomes |
|---|---|---|---|---|---|
| Patisiran (Onpattro) | siRNA | Transthyretin (TTR) / Hereditary ATTR Amyloidosis | LNP with ionizable lipid | Non-targeted (Liver-centric via ApoE adsorption) | ≈80% serum TTR reduction; Improved neuropathy; Boxed warning for infusion-related reactions [2] |
| Givosiran (Givlaari) | siRNA | Aminolevulinic Acid Synthase 1 / Acute Hepatic Porphyria | Enhanced Stabilization Chemistry (ESC)-GalNAc conjugate | Active (ASGPR-mediated hepatocyte targeting) | ≈90% reduction in aminolevulinic acid attacks; Injection-site reactions and hepatic toxicity [2] |
| Inclisiran (Leqvio) | siRNA | PCSK9 / Hypercholesterolemia | ESC-GalNAc conjugate | Active (ASGPR-mediated hepatocyte targeting) | ≈50% sustained LDL-C reduction with biannual dosing; Favorable safety profile [2] |
| COVID-19 mRNA Vaccines (Moderna & Pfizer-BioNTech) | mRNA | SARS-CoV-2 Spike Protein / COVID-19 Prevention | LNP with ionizable lipids | Non-targeted (Primarily liver, immune cells) | >90% efficacy against severe disease; Robust neutralizing antibodies; Myocarditis rare side effect [2] [24] |
| Pegylated Liposomal Doxorubicin (Doxil/Caelyx) | (Non-nucleic acid control) | Various Cancers | PEGylated Liposome | Passive (EPR effect in tumors) | Prolonged circulation vs. free doxorubicin; Hand-foot syndrome; Demonstrates EPR limitations in humans [74] |
Comparative Analysis of Delivery Systems
Non-Targeted Versus Actively Targeted Delivery
The choice between non-targeted and targeted delivery systems represents a fundamental strategic decision in nucleic acid drug development, with significant implications for therapeutic efficacy, safety, and manufacturing complexity.
Table 2: Targeted vs. Non-Targeted Delivery Systems: Comparative Analysis
| Parameter | Non-Targeted Systems (e.g., Standard LNPs) | Actively Targeted Systems (e.g., Antibody-LNPs, GalNAc-Conjugates) |
|---|---|---|
| Targeting Mechanism | Passive (Biodistribution based on physicochemical properties; Liver uptake via ApoE) | Active (Receptor-ligand interaction; e.g., ASGPR for hepatocytes, antibodies for specific cell types) [23] |
| Delivery Efficiency | High for hepatocytes (~30-40% hepatic sequestration); Variable for other tissues | Greatly enhanced for specific cell types (e.g., ~200-fold increase in lung delivery with anti-PECAM-1 Ab-LNPs) [23] |
| Specificity & Off-Target Effects | Significant off-target accumulation (e.g., liver, spleen); Higher risk of dose-limiting toxicities | Markedly reduced off-target exposure; Potential for lower systemic toxicity [23] |
| Therapeutic Index | Moderate (Often requires higher doses to achieve efficacy at target site) | Potentially higher (More drug reaches intended site of action) [23] |
| Manufacturing Complexity | Relatively simpler; Established processes | More complex (Additional conjugation steps; Characterization of targeting ligand integrity) [23] |
| Dosing Frequency | Variable (May require more frequent administration) | Potential for less frequent dosing (Due to improved targeting efficiency) [2] |
| Clinical Translation Success | High for liver targets (Multiple approvals); Limited for extrahepatic targets | Emerging success (GalNAc-siRNAs approved; Ab-LNPs in development) [2] [23] |
Analysis of Clinical Outcomes by Delivery Strategy
The clinical data from approved nucleic acid drugs reveal clear patterns connecting delivery strategies to therapeutic outcomes:
Liver-Targeted Therapies: The most significant clinical successes to date have emerged from liver-directed therapies, utilizing both non-targeted LNPs and targeted GalNAc-conjugates. GalNAc-conjugated siRNAs demonstrate superior specificity for hepatocytes, enabling subcutaneous administration with extended dosing intervals (e.g., inclisiran's biannual regimen) and reduced systemic exposure compared to first-generation LNP formulations. [2]
The Role of Chemical Modifications: Beyond delivery systems, chemical modifications to the nucleic acids themselves are crucial for clinical success. Modifications such as 2'-sugar modifications (2'-O-methyl, 2'-fluoro) and phosphorothioate backbone alterations enhance stability, reduce immunogenicity, and improve target affinity, working synergistically with delivery platforms to enhance therapeutic potential. [2]
Limitations of Passive Targeting: The clinical experience with non-targeted systems like Doxil reveals significant limitations of passive targeting strategies that rely on the Enhanced Permeability and Retention (EPR) effect. While robust in rodent models, the EPR effect proves highly heterogeneous and less predictable in human tumors, resulting in variable efficacy and suboptimal therapeutic outcomes. [74]
Experimental Protocols for Delivery System Evaluation
In Vitro Characterization Protocols
Comprehensive in vitro characterization establishes foundational understanding of delivery system performance before advancing to complex in vivo models.
Protocol 1: LNP Formulation and Physicochemical Characterization
- Lipid Nanoparticle Preparation: Prepare LNPs using microfluidic mixing technology. Combine an ethanolic lipid mixture (ionizable lipid: DSPC: cholesterol: PEG-lipid at 50:10:38.5:1.5 molar ratio) with aqueous mRNA or siRNA solution at a 3:1 flow rate ratio. [24]
- Particle Size and Zeta Potential: Dilute LNP formulation in 1 mM KCl solution (1:100 v/v). Measure particle size (Z-average diameter) and polydispersity index (PDI) using dynamic light scattering (DLS). Determine zeta potential via phase analysis light scattering (PALS). Record triplicate measurements at 25°C. [24]
- Encapsulation Efficiency: Use Ribogreen fluorescence assay. Dilute LNPs in Tris-EDTA buffer (1:200) with or without 0.5% Triton X-100. Incubate with Ribogreen reagent (1:1000) for 5 minutes protected from light. Measure fluorescence (excitation: 480 nm, emission: 520 nm). Calculate encapsulation efficiency as: (1 - (Fluorescence without Triton / Fluorescence with Triton)) × 100%. [24]
Protocol 2: Cell Targeting and Uptake Efficiency
- Cell Culture: Maintain relevant cell lines (e.g., HepG2 for hepatocytes, HUVEC for endothelial cells) in appropriate media. Plate cells at 1×10^5 cells/well in 24-well plates 24 hours before experimentation.
- LNP Treatment: Incubate cells with Cy5-labeled nucleic acid-loaded LNPs (1 µg/mL nucleic acid concentration) for 4 hours at 37°C, 5% CO₂.
- Flow Cytometry Analysis: Wash cells twice with cold PBS, trypsinize, and resuspend in flow cytometry buffer containing DAPI for viability staining. Analyze minimum 10,000 live cells per sample using flow cytometer. Quantify Cy5-positive population and median fluorescence intensity (MFI). Compare targeted versus non-targeted systems. [23]
In Vivo Evaluation Protocols
In vivo studies provide critical assessment of delivery system performance in physiologically relevant models, bridging the gap between in vitro characterization and clinical application.
Protocol 3: Biodistribution and Organ-Specific Expression
- Animal Models: Use 8-10 week old C57BL/6 mice (n=5-7 per group). For tumor models, use immunocompromised mice with subcutaneous xenografts.
- Dosing Administration: Inject mice intravenously via tail vein with Luciferase-mRNA LNPs (0.5 mg/kg mRNA dose) in 100-200 µL total volume.
- In Vivo Imaging: At predetermined timepoints (4, 12, 24, 48 hours), inject D-luciferin (150 mg/kg IP). Anesthetize mice with isoflurane and image using IVIS Spectrum imaging system (1-minute exposure, medium binning). Quantify fluorescence intensity in regions of interest (ROIs) over major organs using Living Image software. Compare signal intensity in target versus non-target tissues. [23]
Protocol 4: Therapeutic Efficacy and Safety Assessment
- Disease Models: Utilize transgenic mouse models expressing human disease targets (e.g., TTR for amyloidosis models) or human tumor xenografts in immunodeficient mice.
- Therapeutic Dosing: Administer nucleic acid drug (e.g., siRNA at 1-5 mg/kg) via appropriate route (IV, SC) following predetermined schedule (e.g., single dose, weekly, or monthly).
- Efficacy Endpoints: Collect serum/tissue samples at multiple timepoints. Quantify target gene knockdown using qRT-PCR (for siRNA) or ELISA for protein reduction. For tumor models, measure tumor volume twice weekly using calipers.
- Safety Assessment: Monitor body weight, behavior, and clinical signs daily. Collect blood for clinical chemistry (ALT, AST, BUN, Creatinine) and complete blood count at study endpoint. Perform histopathological examination of major organs (liver, spleen, kidneys, lungs) after H&E staining. [2]
Signaling Pathways and Experimental Workflows
Targeted Nucleic Acid Delivery and Intracellular Trafficking
The following diagram illustrates the key signaling pathways and intracellular trafficking mechanisms involved in receptor-targeted nucleic acid delivery, which underlies the superior specificity of advanced delivery systems.
Diagram 1: Intracellular Trafficking Pathway for Targeted Nucleic Acid Delivery. This pathway highlights the receptor-mediated uptake and endosomal escape process that represents the critical bottleneck for efficient nucleic acid delivery. Ab-LNPs and GalNAc-conjugates enhance the initial binding and internalization steps, but efficient endosomal escape remains a challenge for all delivery platforms. [2] [23]
Experimental Workflow for Delivery System Evaluation
The diagram below outlines a comprehensive experimental workflow for the systematic evaluation and comparison of nucleic acid delivery systems, from formulation through in vivo assessment.
Diagram 2: Experimental Workflow for Delivery System Evaluation. This workflow outlines the key stages in the systematic assessment of nucleic acid delivery systems, highlighting critical decision points where formulation advancement decisions are typically made based on predefined success criteria. [2] [24] [23]
The Scientist's Toolkit: Key Research Reagents and Materials
Successful development and evaluation of nucleic acid delivery systems requires specialized reagents and materials with specific functional properties.
Table 3: Essential Research Reagents for Nucleic Acid Delivery System Development
| Reagent/Material | Function | Key Characteristics | Application Examples |
|---|---|---|---|
| Ionizable Lipids | Core structural component of LNPs; enables nucleic acid encapsulation and endosomal escape | pKa ~6.0-6.5; Biodegradable; Low toxicity | SM-102, DLin-MC3-DMA, ALC-0315; LNP self-assembly [24] |
| PEGylated Lipids | LNP surface stabilization; reduces nonspecific protein adsorption; modulates pharmacokinetics | PEG chain length (e.g., PEG2000); Anchoring lipid (e.g., DMG, DSPE); Can limit cellular uptake | ALC-0159; LNP surface engineering [24] |
| Targeting Ligands | Enables specific receptor-mediated cell targeting | High affinity for target receptor; Conjugation chemistry compatibility | GalNAc (for ASGPR); Antibodies (e.g., anti-CD4, anti-PECAM-1); Peptides; Active targeting systems [23] |
| Chemical Modification Reagents | Enhances nucleic acid stability and reduces immunogenicity | 2'-O-methyl, 2'-fluoro ribose; Phosphorothioate backbone; Pseudouridine (Ψ) | Modified nucleoside triphosphates; siRNA/mRNA stability enhancement [2] |
| Fluorescent Reporters | Enables tracking of biodistribution and cellular uptake | High quantum yield; Photostability; Minimal biological interference | Cy5-labeled nucleic acids; Luciferase reporter genes; DiR dyes for in vivo imaging [23] |
Emerging Technologies and Future Perspectives
The field of nucleic acid delivery continues to evolve rapidly, with several emerging technologies showing promise for addressing current limitations:
AI-Driven Formulation Design: Machine learning algorithms are now being deployed to accelerate LNP optimization, with generative adversarial networks (GANs) creating novel ionizable lipid structures and graph neural networks predicting RNA-LNP binding affinity with high accuracy. These approaches can reduce formulation development time from 6-12 months to weeks while improving targeting specificity. [24]
Advanced Targeting Platforms: Antibody-targeted LNPs (Ab-LNPs) represent the next frontier in precision delivery, demonstrating remarkable tissue-specific targeting in preclinical models. Anti-PECAM-1 Ab-LNPs achieved ~200-fold enhancement in lung delivery, while anti-CD4 variants enabled specific T-cell targeting with 30-fold increased reporter expression. Clinical translation is advancing, with Capstan Therapeutics' CPTX2309 (anti-CD19 CAR-T in vivo programming) entering Phase I trials. [23]
Alternative Administration Routes: Research is increasingly focusing on delivery strategies beyond intravenous injection, including pulmonary, intrathecal, and topical administration. These approaches aim to overcome biological barriers through localized delivery rather than systemic targeting, potentially expanding applications to previously inaccessible tissues. [74]
Addressing the Translational Gap: Despite thousands of publications, only an estimated 50-80 nanomedicines have gained global approval by 2025, highlighting a significant translational gap. Future development must focus on integrated formulation strategies that address both biological barriers and manufacturing challenges, with particular attention to scalability, characterization, and regulatory requirements. [74]
The therapeutic application of nucleic acids—including DNA, mRNA, siRNA, and CRISPR-Cas systems—holds transformative potential for treating genetic disorders, cancers, and infectious diseases. However, the clinical success of these therapies is critically dependent on the delivery platform's ability to achieve two often competing goals: high transfection efficiency (the effective delivery of genetic cargo into target cells) and precise tissue specificity (the selective targeting of diseased tissues while minimizing off-target effects) [48]. Researchers and drug developers face a complex landscape of delivery technologies, each with distinct strengths and limitations in these key performance parameters. This guide provides a systematic, data-driven comparison of major viral and non-viral delivery platforms, focusing on their performance in tissue specificity and transfection efficiency to inform rational platform selection for therapeutic development.
Platform Comparison: Performance Metrics and Mechanisms
This section objectively compares the core technologies, presenting quantitative data and mechanistic insights that define their performance profiles.
Table 1: Head-to-Head Comparison of Nucleic Acid Delivery Platforms
| Delivery Platform | Typical Transfection Efficiency | Tissue Specificity Mechanism | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Viral Vectors (e.g., AAV, Lentivirus) | High (>70-90% in permissive cells) [75] | Natural tropism; engineered capsids [76] | High efficiency; sustained expression [75] | Immunogenicity; insertional mutagenesis; limited payload capacity [77] [76] |
| Lipid Nanoparticles (LNPs) | Moderate to High (Varies with formulation, e.g., ~50-80% in hepatocytes) [75] | Passive (size-based) & active (ligand-functionalized) targeting [70] [75] | Rapid development; scalable production; proven clinical success [78] [75] | Primarily accumulates in liver; potential reactogenicity [79] |
| Polymeric Nanoparticles | Moderate (~30-70%) [77] | Tunable surface chemistry for ligand attachment [70] | Highly tunable structure; biocompatible degradation [75] | Lower efficiency vs. viral/LNPs; potential polymer-specific toxicity [77] |
| GalNAc-siRNA Conjugates | High in hepatocytes (>80% target gene knockdown) [79] | Active targeting of ASGPR receptor on hepatocytes [79] | Exceptional liver specificity; excellent safety profile; multiple approved drugs [79] | Restricted to liver applications [79] |
| Electroporation | High ex vivo (>80% in susceptible cells) [77] [75] | Physical localization (electrode placement) [77] | Broad cargo capacity; independence from biological pathways [77] | Mostly applicable ex vivo; high cell mortality if poorly optimized [75] |
| Tissue Nanotransfection (TNT) | High in superficial tissues (Demonstrated reprogramming in vivo) [77] | Highly localized physical delivery via nanochannels [77] | Non-viral; in vivo application; minimal off-target effects [77] | Limited to directly accessible tissues; depth penetration a challenge [77] |
| Microfluidic Squeezing | Moderate to High (e.g., >90% in certain immune cells) [76] | Physical deformation; cell-type-specific channel optimization [76] | High viability in hard-to-transfect cells (e.g., primary T cells) [76] | Currently best suited for ex vivo use; requires specialized equipment [76] |
Experimental Protocols for Key Platforms
To ensure the reproducibility of the performance data cited in this guide, this section details the core experimental methodologies used to evaluate leading platforms.
Tissue Nanotransfection (TNT)
Objective: To achieve highly localized in vivo cellular reprogramming or gene editing via nanoelectroporation [77]. Key Materials: TNT device (silicon chip with hollow nanochannels), pulse generator, plasmid DNA/mRNA/CRISPR cargo in solution [77]. Workflow:
- The genetic cargo solution is loaded into the reservoir of the TNT device.
- The device is placed directly onto the surface of the target tissue (e.g., skin).
- A focused, high-intensity electrical pulse is applied for milliseconds.
- The electric field is concentrated at the nanochannel tips, creating transient, reversible nanopores in the plasma membranes of adjacent cells.
- The genetic cargo is driven through these pores into the cell cytoplasm via electrophoretic forces.
- The nanopores reseal within milliseconds to seconds, maintaining cell viability [77]. Key Performance Parameters: Pulse voltage (~100-500 V), duration (ms), and number of pulses are optimized for specific tissue and cargo types to maximize efficiency and minimize cytotoxicity [77].
GalNAc-siRNA Conjugate Delivery
Objective: To achieve efficient and specific gene silencing in hepatocytes. Key Materials: Fully chemically modified siRNA conjugated to a triantennary N-acetylgalactosamine (GalNAc) ligand [79]. Workflow:
- Following systemic administration, the GalNAc-siRNA conjugate binds with high affinity to the asialoglycoprotein receptor (ASGPR) on the surface of hepatocytes.
- The receptor-ligand complex is internalized via clathrin-mediated endocytosis.
- The siRNA must escape the endosomal compartment to enter the cytoplasm—a key rate-limiting step.
- In the cytoplasm, the siRNA guide strand is loaded into the RNA-induced silencing complex (RISC).
- The activated RISC binds to complementary target mRNA and cleaves it, leading to degradation and potent gene silencing [79]. Key Performance Parameters: siRNA chemical modification pattern (e.g., 2'-O-methyl content) significantly impacts stability and efficacy, while the high affinity of the GalNAc-ASGPR interaction drives exceptional liver specificity [80] [79].
Microfluidic Intracellular Delivery
Objective: To transfect hard-to-transfect cells (e.g., primary immune cells) ex vivo with high efficiency and viability. Key Materials: Microfluidic squeezing device (e.g., constriction-based channels), cell suspension, nucleic acid cargo [76]. Workflow:
- A mixture of cells and nucleic acid cargo is passed through a microfluidic channel narrower than the cell diameter.
- The physical constriction squeezes the cells, inducing transient membrane pores.
- The nucleic acid cargo in the surrounding buffer diffuses into the cells through these pores.
- Upon exiting the constriction, the cell membrane rapidly reseals, trapping the cargo inside [76]. Key Performance Parameters: Channel width, flow rate, and cell deformation time are critically optimized for different cell types to balance delivery efficiency with cell viability, which can exceed 90% [76].
Visualizing Workflows and Targeting Mechanisms
The following diagrams illustrate the core operational and targeting principles of the compared platforms.
Experimental Workflow for Platform Evaluation
Mechanisms of Tissue Targeting
The Scientist's Toolkit: Essential Reagents and Materials
This table catalogs key reagents and materials critical for researching and developing the nucleic acid delivery platforms discussed.
Table 2: Essential Research Reagents and Materials
| Item | Function/Application | Key Considerations |
|---|---|---|
| Ionizable Cationic Lipids | Core component of LNPs; encapsulates nucleic acids and facilitates endosomal escape [78] [75]. | Biodegradability (e.g., A4B4-S3, SM-102) reduces toxicity [78]. Critical for in vivo safety and efficiency. |
| GalNAc Ligand | Targeting moiety for delivery to hepatocytes; conjugated directly to siRNA or other oligonucleotides [79]. | High-affinity binding to ASGPR is crucial. The triantennary structure is optimal for receptor engagement [79]. |
| Chemically Modified siRNAs | Therapeutic payload; designed for gene silencing via RNAi [80] [79]. | 2'-O-methyl or 2'-fluoro modifications are essential to enhance nuclease stability and reduce immunogenicity [80]. |
| CRISPR-Cas Components | Gene editing payload; includes mRNA for Cas protein and sgRNA for target specificity [81] [78]. | Delivery of both components simultaneously is a key challenge. All-in-one AAV vectors have size limitations [81]. |
| Polyethyleneimine (PEI) | Cationic polymer for forming polyplexes with nucleic acids; common transfection reagent [79]. | High transfection efficiency but associated with significant cytotoxicity. Branching and molecular weight impact performance [79]. |
| Microfluidic Devices | Platform for ex vivo transfection via cell squeezing or for scalable LNP synthesis [76]. | Channel design (e.g., width, geometry) must be optimized for specific cell types to balance efficiency and viability [76]. |
| TNT Silicon Chip | The core device for in vivo nanoelectroporation, featuring an array of hollow nanochannels [77]. | Requires a compatible pulse generator. Sterilization (e.g., ethylene oxide) is essential for in vivo use [77]. |
The therapeutic potential of nucleic acid drugs (NADs), including small interfering RNA (siRNA), antisense oligonucleotides (ASOs), and messenger RNA (mRNA), is fundamentally constrained by a single, significant challenge: the efficient and targeted delivery of these macromolecules to their site of action within cells. [2] The overarching thesis in the field posits that overcoming biological barriers through advanced delivery systems is a critical determinant of clinical success. These barriers include rapid nuclease degradation, short plasma half-life, inefficient cellular uptake, and entrapment within endosomes. [2] [48] This review objectively analyzes clinical data to compare the performance of targeted versus non-targeted delivery strategies, providing a structured evaluation of their respective successes, failures, and tolerability profiles. The evidence demonstrates that while non-targeted systems like lipid nanoparticles (LNPs) enabled the first generation of approved NADs, the future of the field lies in the development of precisely targeted delivery platforms to expand treatable tissues and improve therapeutic indices. [82] [27]
Clinical Outcomes: A Comparative Analysis of Delivery Platforms
The clinical journey of nucleic acid therapeutics reveals a clear trajectory from initial non-targeted systems to increasingly sophisticated targeted approaches. The summary data in the tables below quantifies the performance and safety profiles of key delivery platforms.
Table 1: Clinical Outcomes of Non-Targeted vs. Targeted Nucleic Acid Delivery Systems
| Delivery System / Drug | Nucleic Acid Type | Indication | Key Efficacy Metric | Common Adverse Events |
|---|---|---|---|---|
| Non-Targeted: LNP (Patisiran) [27] | siRNA | hATTR Amyloidosis | Improved neuropathy scores (mNIS+7) | Infusion-related reactions, flushing |
| Non-Targeted: LNP (mRNA Vaccines) [27] | mRNA | COVID-19 | ~95% prevention of infection [27] | Injection-site pain, fatigue, fever [27] |
| Targeted: GalNAc-siRNA (Givosiran) [27] [25] | siRNA | Acute Hepatic Porphyria | 74% reduction in annualized attack rate [27] | Nausea, injection-site reactions |
| Targeted: GalNAc-siRNA (Inclisiran) [25] | siRNA | Hypercholesterolemia | Sustained LDL-C reduction >50% for 6 months [25] | Arthralgia, headache |
| Targeted: Ligand-Polymer (?) |
Many trials terminated [82] | siRNA/miRNA | Various (e.g., Oncology) | Trial Termination / Lack of Efficacy | Off-target liver toxicity, immune activation [82] |
Table 2: Tolerability and Manufacturing Comparison of Delivery Platforms
| Delivery Platform | Dosing Frequency | Stability & Storage | Manufacturing Complexity | Primary Clinical Limitation |
|---|---|---|---|---|
| LNP (Non-Targeted) | Every 3-4 weeks (Patisiran) or 2 doses (Vaccines) [27] | Cold-chain required [27] | High complexity; scalable [48] | Reactogenicity; primarily hepatic uptake [82] |
| GalNAc-Conjugate (Targeted) | Every 3-6 months (Inclisiran) [25] | Refrigerated or ambient | Lower complexity; highly scalable [82] | Limited to hepatocytes [82] |
| Polymeric Nanoparticles | Varies (often frequent) | Varies | Moderate to high complexity [48] | Polymer-specific cytotoxicity [48] |
| Viral Vectors (e.g., AAV) | Often one-time administration | Frozen | Very high complexity [48] | Immunogenicity; insertional mutagenesis risk [48] |
The data reveals a critical trade-off. Non-targeted LNPs are highly versatile and were crucial for the first FDA-approved siRNA drug (Patisiran) and mRNA vaccines, but they often necessitate complex cold-chain logistics and are associated with infusion-related reactions due to their non-specific interactions with the immune system. [2] [27] In contrast, targeted GalNAc conjugates, which leverage the asialoglycoprotein receptor on hepatocytes, demonstrate a superior therapeutic index: they enable subcutaneous administration, less frequent dosing due to enhanced potency, and a markedly improved tolerability profile. [82] [25] However, the most significant failure mode for non-targeted systems, particularly in oncology trials, has been off-target liver toxicity and immune activation, leading to the termination of many clinical programs. [82]
Experimental Protocols for Delivery System Evaluation
Robust preclinical evaluation is essential for predicting clinical performance and tolerability. The following protocols represent standardized methodologies for characterizing nucleic acid delivery systems.
Protocol 1: In Vivo Biodistribution and Organ Targeting Efficiency
This protocol quantifies the accumulation of a delivery system in target versus non-target tissues, a primary indicator of potential efficacy and toxicity. [82]
- Formulation Labeling: The nucleic acid payload (e.g., siRNA) is labeled with a near-infrared (NIR) fluorophore (e.g., Cy5.5) or a radionuclide (e.g., ^99mTc). The integrity of the formulated delivery system (LNP or conjugate) is verified post-labeling.
- Animal Dosing: Administer the labeled formulation to animal models (e.g., mice or non-human primates) via the intended clinical route (e.g., intravenous or subcutaneous). A control group receives the free (unformulated) nucleic acid.
- Imaging and Analysis: At predetermined time points (e.g., 1, 4, 24, 48 hours), use non-invasive live imaging (e.g., IVIS Spectrum or PET/CT) to track real-time biodistribution.
- Ex Vivo Quantification: At the study endpoint, euthanize the animals, collect major organs (liver, spleen, kidneys, heart, lungs, and target tissue), and homogenize them. Quantify the fluorescence or radioactivity in each organ using a plate reader or gamma counter. Data is expressed as percentage of injected dose per gram of tissue (%ID/g).
- Data Interpretation: Successful targeted systems show high and specific accumulation in the target organ (e.g., >80% ID in liver for GalNAc-conjugates) with minimal off-target accumulation. Non-targeted LNPs often show significant sequestration in the liver and spleen due to the mononuclear phagocyte system. [82]
Protocol 2: Functional Gene Silencing and Therapeutic Efficacy
This assay measures the downstream biological effect of the delivered nucleic acid, confirming that the payload has reached its active site. [27]
- Animal Model Selection: Utilize a relevant disease model. This could be a transgenic mouse expressing a human target gene (e.g., transthyretin for Patisiran models) or a xenograft model for oncology targets.
- Dosing Regimen: Animals are dosed with the therapeutic formulation, a negative control formulation (e.g., non-targeting siRNA), and a vehicle control. Doses are based on prior pharmacokinetic/pharmacodynamic (PK/PD) studies.
- Sample Collection: At protocol-specified times (e.g., 48 hours to 2 weeks post-dose), collect tissue biopsies (e.g., liver needle biopsy) and plasma/serum.
- Molecular Analysis:
- mRNA Knockdown: Extract total RNA from homogenized tissue and quantify target mRNA levels using reverse transcription quantitative PCR (RT-qPCR). Results are normalized to housekeeping genes and reported as % reduction relative to control.
- Protein Knockdown: For protein-level analysis, use techniques like ELISA or Western Blot on tissue lysates or plasma samples to measure reduction in the target protein.
- Phenotypic Endpoint: Measure a clinically relevant endpoint, such as reduction in tumor volume, improvement in a neurological score, or normalization of a metabolic marker.
- Data Interpretation: A potent delivery system will show a dose-dependent, durable, and specific reduction in both target mRNA and protein, leading to a significant improvement in the phenotypic endpoint. [2] [27]
Protocol 3: Comprehensive Tolerability and Immunogenicity Profiling
This protocol is critical for identifying the safety limitations that have plagued many clinical trials. [82] [48]
- Study Design: Repeat-dose toxicology study in two species (e.g., rodent and non-rodent). Animals receive multiple doses of the test article at levels exceeding the planned clinical dose.
- Clinical Observations: Monitor for signs of toxicity, including changes in body weight, food consumption, and behavior.
- Clinical Pathology: Analyze blood samples for hematology (e.g., changes in immune cell counts) and clinical chemistry (e.g., liver enzymes ALT/AST, markers of kidney function).
- Immunogenicity Assessment:
- Cytokine Release: Measure plasma levels of pro-inflammatory cytokines (e.g., IFN-α, IL-6, TNF-α) at multiple timepoints after the first and last doses using a multiplex immunoassay.
- Anti-Drug Antibodies: Screen for the development of antibodies against the nucleic acid payload or the delivery vehicle components.
- Histopathology: Perform macroscopic and microscopic examination of all major organs post-mortem, with special attention to the liver, spleen, and injection site.
- Data Interpretation: Non-targeted systems, especially cationic lipids in LNPs, often trigger transient increases in pro-inflammatory cytokines and elevated liver enzymes. Targeted systems like GalNAc conjugates typically show a cleaner profile, with injection-site reactions being the most common finding. [82] [48]
Visualizing Key Delivery Pathways and Mechanisms
The following diagrams illustrate the fundamental differences in the cellular journeys of non-targeted and targeted nucleic acid delivery systems, highlighting the mechanistic basis for their differing clinical profiles.
Diagram 1: Contrasting Cellular Fates of Non-Targeted vs. Targeted Delivery Systems. The non-targeted LNP pathway (red) is characterized by non-specific uptake and inefficient endosomal escape, often leading to degradation and toxicity. The targeted GalNAc pathway (green) uses specific receptor-mediated entry into hepatocytes, leading to efficient escape and successful gene silencing.
Diagram 2: Engineering Solutions for Nucleic Acid Drug Delivery. This workflow outlines the primary strategies to overcome delivery challenges: chemical modifications to the nucleic acid itself (yellow) to improve stability, ligand conjugation (blue) for targeted uptake, and vehicle formulation (red) for encapsulation and systemic protection.
The Scientist's Toolkit: Essential Reagents for Nucleic Acid Delivery Research
The development and evaluation of nucleic acid delivery systems rely on a core set of research reagents and materials. The following table details key solutions used in the field.
Table 3: Key Research Reagent Solutions for Nucleic Acid Delivery
| Research Reagent / Material | Core Function | Application in Experimental Protocols |
|---|---|---|
| Ionizable Cationic Lipids (e.g., DLin-MC3-DMA) [2] [48] | Forms the core of LNPs; enables nucleic acid encapsulation and endosomal escape via proton sponge effect. | Protocol 1 & 2: Primary component of non-targeted LNP delivery systems for in vivo efficacy and biodistribution studies. |
| N-Acetylgalactosamine (GalNAc) Ligand [82] [25] | Targets the asialoglycoprotein receptor (ASGPR) on hepatocytes for highly specific cellular uptake. | Protocol 2: Covalently conjugated to siRNA for subcutaneous administration in targeted delivery and gene silencing studies. |
| Phosphorothioate (PS) Modified Oligonucleotides [82] | Increases resistance to nuclease degradation and enhances binding to plasma proteins, extending half-life. | All Protocols: A foundational chemical modification used in nearly all clinical-stage ASOs and siRNAs to improve stability. |
| Near-Infrared (NIR) Dyes (e.g., Cy5.5, Cy7) [82] | Allows for non-invasive, real-time tracking of the biodistribution of formulated nucleic acids in live animals. | Protocol 1: Used to label the nucleic acid payload for optical imaging in biodistribution studies. |
| Helper Lipids (DSPC, Cholesterol) [48] | Enhances the stability and fusogenicity of LNPs, supporting cellular uptake and endosomal escape. | Protocol 1 & 2: Standard component in LNP formulations to optimize structure and function. |
| Polymer-Based Transfection Reagents (e.g., PEI) [48] | Condenses nucleic acids into polyplexes for in vitro screening and some in vivo applications. | Protocol 2: Often used for initial in vitro proof-of-concept studies due to high transfection efficiency in cell culture. |
The critical analysis of clinical trial data unequivocally demonstrates that the evolution from non-targeted to targeted delivery systems has been a decisive factor in transforming nucleic acid drugs from a promising concept into a clinical reality. The success of GalNAc-siRNA conjugates in treating liver-specific diseases has set a new benchmark for potency, durability, and tolerability. [25] However, the heavy reliance on hepatocyte-targeting also underscores the field's most significant current limitation: the effective delivery to extrahepatic tissues. [82] [27] Future progress hinges on the discovery and validation of novel targeting ligands for other tissues, such as the central nervous system, skeletal muscle, and tumors. Furthermore, the continued refinement of LNP formulations and the exploration of alternative modalities, such as virus-like particles and engineered exosomes, represent the next frontier for overcoming the persistent challenge of endosomal escape and achieving the full therapeutic potential of nucleic acid medicines across a broader spectrum of human diseases. [82] [48] [27]
The journey of nucleic acid drugs (NADs) from fundamental research (bench) to clinical application (bedside) represents one of the most promising yet challenging frontiers in modern therapeutics. These innovative drugs, including small interfering RNA (siRNA), messenger RNA (mRNA), antisense oligonucleotides (ASOs), and gene editing systems like CRISPR/Cas9, offer unprecedented potential for treating genetic disorders, cancers, and infectious diseases by targeting the fundamental genetic mechanisms of disease [2]. However, their translation into clinically viable medicines requires navigating complex pharmacological, manufacturing, and regulatory landscapes.
The bench-to-bedside transition for nucleic acid therapeutics faces significant hurdles that extend beyond basic scientific discovery. As highlighted in translational research literature, the pace at which fundamental biological discoveries translate into new therapies has remained frustratingly stagnant despite tremendous increases in our understanding of human biology [83]. Academic institutions, as major recipients of public research investment, bear significant responsibility for translating discoveries into human benefit, yet they often lack the infrastructure, expertise, and resources to navigate the expensive, highly regulated steps required for therapeutic development [83].
This review examines the critical considerations in scaling nucleic acid delivery systems from laboratory research to commercial therapeutics, with particular emphasis on the comparative advantages and challenges of targeted versus non-targeted delivery approaches. By synthesizing current research, experimental data, and regulatory frameworks, we provide a comprehensive framework for researchers and drug development professionals to advance nucleic acid therapeutics through the translational pipeline.
Nucleic Acid Therapeutics: Mechanisms and Classifications
Nucleic acid drugs constitute a diverse family of therapeutic modalities with distinct mechanisms of action, target sites, and functional outcomes. Understanding these fundamental differences is essential for designing appropriate delivery strategies and manufacturing processes.
Table 1: Classification of Nucleic Acid Therapeutics and Their Mechanisms
| Drug Class | Structure | Target Site | Primary Mechanism | Therapeutic Outcome |
|---|---|---|---|---|
| ASOs | Single-stranded DNA/RNA (12-24 nt) | Nucleus/Cytosol | RNase H-mediated degradation or steric blockage | Gene silencing or splicing modification |
| siRNA | Double-stranded RNA (21-25 bp) | Cytosol | RNAi; RISC-mediated mRNA cleavage | Specific gene silencing |
| mRNA | Single-stranded RNA | Cytosol | Protein translation | Protein replacement or vaccination |
| CRISPR/Cas9 | sgRNA + Cas9 protein | Nucleus | Gene editing | DNA modification or correction |
| Aptamers | Structured oligonucleotides | Extracellular/Cell surface | Protein binding | Targeted inhibition or activation |
NADs can be broadly categorized into three groups based on their mechanisms: (1) those that target nucleic acids to regulate protein expression (ASOs, siRNA, CRISPR/Cas9); (2) those that target proteins directly (aptamers); and (3) those that express proteins (mRNA) [2]. Each class presents distinct delivery challenges based on their subcellular destination—siRNA and mRNA function in the cytosol, while ASOs and CRISPR/Cas9 need to reach the nucleus [6].
The chemical evolution of these therapeutics has been crucial for their clinical application. First-generation ASOs featured phosphorothioate modifications to improve nuclease resistance and activate RNase H-mediated target degradation [84]. Second-generation modifications introduced 2'-O-methyl and 2'-O-methoxyethyl groups to enhance binding affinity and reduce toxicity, while third-generation chemistries including peptide nucleic acids (PNAs) and phosphorodiamidate morpholino oligomers (PMOs) further improved specificity and pharmacokinetic properties [84]. These chemical optimizations represent critical early steps in the bench-to-bedside transition, addressing fundamental pharmacological challenges before clinical evaluation.
Delivery Systems: Targeted vs. Non-Targeted Approaches
Delivery systems constitute perhaps the most significant determinant of success for nucleic acid therapeutics, as naked nucleic acids cannot efficiently cross cellular membranes and are rapidly degraded by nucleases in biological environments [2] [85]. The choice between targeted and non-targeted delivery strategies carries profound implications for therapeutic efficacy, safety profiles, manufacturability, and regulatory approval pathways.
Non-Targeted Delivery Systems
Non-targeted (passive) delivery approaches rely on physicochemical properties and physiological processes for tissue accumulation rather than specific molecular recognition events.
Table 2: Non-Targeted Nucleic Acid Delivery Systems
| Delivery System | Composition | Mechanism | Advantages | Limitations |
|---|---|---|---|---|
| Cationic Liposomes/LNPs | Ionizable lipids, phospholipids, cholesterol, PEG-lipids | Electrostatic complexation, endocytosis | High payload capacity, proven clinical success | Limited tissue specificity, immunogenicity concerns |
| Polymeric Nanoparticles | PEI, PLGA, chitosan, dendrimers | Charge-mediated complexation | Structural versatility, controllable release | Potential cytotoxicity, batch-to-batch variability |
| Cationic Peptides | Sequence-defined oligoaminoamides | Molecular recognition, membrane fusion | Precise synthesis, biodegradability | Complex synthesis, scale-up challenges |
The most clinically advanced non-targeted systems are lipid-based nanoparticles (LNPs), which have demonstrated remarkable success with siRNA (patisiran) and mRNA (COVID-19 vaccines) [86] [85]. LNPs facilitate cellular uptake through endocytosis and enable endosomal escape via the proton sponge effect or membrane destabilization mechanisms. However, they primarily accumulate in the liver and spleen through the reticuloendothelial system, limiting applications for extrahepatic targets [86].
Polymeric vectors represent another prominent non-targeted approach. Polyethylenimine (PEI) and its derivatives efficiently condense nucleic acids through electrostatic interactions and promote endosomal escape via proton buffering capacity, but their clinical translation has been hampered by cytotoxicity concerns [6]. More recently, sequence-defined oligomers have emerged as promising alternatives with improved safety profiles and precisely tunable properties [6].
Targeted Delivery Systems
Targeted delivery systems incorporate specific ligands that recognize molecular markers on target cells, enhancing specificity and reducing off-target effects. These systems represent the cutting edge of nucleic acid therapeutic development but introduce additional complexity to manufacturing and characterization.
Table 3: Targeted Nucleic Acid Delivery Approaches
| Targeting Strategy | Ligand Type | Target Receptor | Applications | Development Status |
|---|---|---|---|---|
| Antibody-mediated | Monoclonal antibodies, scFv fragments | HER2, EGFR, transferrin receptor | Oncology, CNS disorders | Preclinical/Clinical trials |
| Ligand-based | Transferrin, folate, aptamers | Transferrin receptor, folate receptor | Cancer, inflammatory diseases | Advanced preclinical |
| Peptide-based | RGD, cell-penetrating peptides | Integrins, undefined | Cardiovascular, oncology | Research phase |
| Sugar-mediated | Galactose, mannose | Asialoglycoprotein receptor | Liver-targeted delivery | Clinical (givosiran) |
Immunoliposomes exemplify the targeted approach by conjugating antibody fragments to liposomal surfaces. Preclinical studies with anti-HER2 immunoliposomes demonstrated efficient targeting to HER2-overexpressing cancer cells, internalization, and intracellular delivery of encapsulated agents [86]. These targeted systems exhibited superior antitumor activity compared to non-targeted liposomes or free drug combinations, highlighting the therapeutic potential of precise delivery [86].
Ligand-directed targeting leverages naturally occurring receptor-ligand interactions for cell-specific delivery. GalNAc (N-acetylgalactosamine) conjugates represent the most clinically successful example, enabling efficient hepatocyte targeting through the asialoglycoprotein receptor and facilitating the development of multiple approved siRNA therapeutics [85]. This approach demonstrates how strategic targeting can simplify delivery challenges while maintaining manufacturability.
Comparative Performance Data
Direct comparisons between targeted and non-targeted systems reveal context-dependent advantages that inform translational strategy selection.
Table 4: Experimental Comparison of Targeted vs. Non-Targeted Delivery Systems
| Parameter | Non-Targeted LNPs | GalNAc-Conjugates | Immunoliposomes |
|---|---|---|---|
| Hepatocyte Transfection | Moderate (15-25%) | High (70-90%) | Low (<5%) |
| Non-Hepatic Delivery | Limited | Minimal | Possible with appropriate targeting |
| Manufacturing Complexity | Medium | Low | High |
| Scalability | High | High | Medium |
| Dosing Frequency | Every 2-4 weeks | Every 3-6 months | Varies |
| Immunogenicity | Moderate | Low | Variable |
Experimental studies directly comparing targeted versus non-targeted approaches demonstrate clear trade-offs. In murine models, HER2-targeted immunoliposomes showed 5-10-fold increased accumulation in HER2-overexpressing tumors compared to non-targeted liposomes, with corresponding enhancements in therapeutic efficacy [86]. However, this improved performance comes with significantly more complex manufacturing and characterization requirements that must be addressed during translational development.
Experimental Methodologies for Delivery System Evaluation
Rigorous preclinical evaluation is essential for selecting lead candidates with the greatest translational potential. Standardized experimental protocols enable meaningful comparisons between delivery approaches and build the evidence base required for regulatory submissions.
In Vitro Characterization Protocols
Physicochemical Characterization:
- Size and Zeta Potential: Determine using dynamic light scattering (DLS) in relevant physiological buffers (e.g., PBS, 150 mM NaCl) at 0.1-1 mg/mL concentration. Measure polydispersity index (PDI) as indicator of homogeneity.
- Nucleic Acid Loading Efficiency: Quantify using fluorescent dye exclusion assays (e.g., RiboGreen) or gel electrophoresis. Calculate encapsulation efficiency as (total NA - free NA)/total NA × 100%.
- Stability Assessment: Inculate in 50% fetal bovine serum at 37°C with continuous shaking. Sample at predetermined timepoints (0, 1, 2, 4, 8, 12, 24, 48 h) and analyze nucleic acid integrity.
Functional Cellular Assays:
- In Vitro Transfection Efficiency: Seed target cells in 24-well plates at 50,000 cells/well. Complex fluorescently-labeled nucleic acids with delivery systems at optimized ratios. Transfect at varying concentrations (10-200 nM nucleic acid). Quantify uptake (4 h) and expression (24-48 h) via flow cytometry and fluorescence microscopy.
- Dose-Response Analysis: Serially dilute formulations (0.1-1000 nM) in target cells. Measure therapeutic endpoint (e.g., target protein reduction, reporter expression) after 48-72 h. Calculate EC₅₀ values using four-parameter logistic regression.
- Cytotoxicity Assessment: Co-incubate formulations with cells for 24-48 h. Measure cell viability using MTT, alamarBlue, or ATP-based assays. Calculate selectivity index (cytotoxic concentration₅₀/therapeutic concentration₅₀).
In Vivo Evaluation Workflows
Biodistribution and Pharmacokinetics:
- Fluorescent/Bioluminescent Imaging: Administer formulations carrying labeled nucleic acids (Cy5, Cy7, luciferase) via appropriate route. Image at predetermined timepoints (0.5, 2, 6, 12, 24, 48, 72 h) using IVIS or similar systems. Quantify signal intensity in target versus non-target tissues.
- qPCR-Based Biodistribution: Extract total DNA/RNA from tissues (liver, spleen, kidney, lung, heart, tumor). Perform qPCR with species-specific primers for administered nucleic acid. Normalize to tissue weight and housekeeping genes.
- Pharmacokinetic Profiling: Collect blood samples at multiple timepoints (5, 15, 30 min; 1, 2, 4, 8, 12, 24 h). Measure nucleic acid concentration in plasma using hybridization ELISA or qPCR. Calculate AUC, Cₘₐₓ, t₁/₂, and clearance.
Efficacy Assessment:
- Disease Model Validation: Employ clinically relevant animal models (xenograft, syngeneic, genetic). Confirm target expression in disease tissue before intervention.
- Dosing Regimen Optimization: Test single versus multiple dosing, various routes (IV, IP, SC), and different dose levels. Include appropriate controls (PBS, empty vector, scrambled nucleic acid).
- Therapeutic Endpoint Analysis: Measure disease-specific parameters (tumor volume, biomarker levels, physiological function) alongside molecular endpoints (target gene expression, protein reduction).
Figure 1: Experimental Workflow for Delivery System Evaluation - This diagram outlines the key stages in preclinical assessment of nucleic acid delivery systems, from in vitro characterization to in vivo evaluation.
Manufacturing and Scalability Considerations
The transition from laboratory-scale production to commercial manufacturing presents substantial challenges that must be addressed through strategic platform selection and process optimization. Manufacturing considerations often dictate the ultimate commercial viability of nucleic acid therapeutics.
Platform Technologies and Scale-Up Strategies
Academic versus Commercial Manufacturing: Early-stage development in academic settings typically employs open manufacturing systems and research-grade reagents, which are practical for proof-of-concept studies but insufficient for clinical translation [87]. The transition to commercial manufacturing requires closed, automated systems, GMP-grade materials, and rigorous quality control to ensure product consistency and sterility [87].
Process Design and Control: Implementing Quality by Design (QbD) principles early in development establishes a scientific foundation for process understanding and control. This involves defining Critical Quality Attributes (CQAs), identifying Critical Process Parameters (CPPs), and establishing design space for manufacturing operations [87]. For lipid nanoparticles, CPPs typically include mixing velocity, temperature, flow rate ratios, and total flow rate, which significantly impact particle size, polydispersity, and encapsulation efficiency.
Scale-Up Approaches:
- Scale-Out: Replicating small-scale processes multiple times in parallel (e.g., multiple bioreactors)
- Scale-Up: Increasing batch size through proportional parameter adjustments
- Platform Adoption: Implementing standardized, validated manufacturing platforms across product lines
Comparative Manufacturing Considerations
Table 5: Manufacturing Considerations for Different Delivery Platforms
| Parameter | LNPs | Polymer Nanoparticles | GalNAc-Conjugates | Viral Vectors |
|---|---|---|---|---|
| Manufacturing Platform | Microfluidics, T-mixer | Solvent evaporation, nanoprecipitation | Chemical synthesis | Cell culture, transfection |
| Process Complexity | Medium | Medium-High | Low | High |
| Batch Consistency | High (with control) | Variable | Very High | Medium |
| Sterilization Method | Filtration | Filtration | Filtration | Filtration/Ultrafiltration |
| Storage Conditions | -20°C to -80°C (lyophilized) | -20°C (lyophilized) | 2-8°C (lyophilized) | -60°C or below |
| Cost of Goods | Medium | Low-Medium | Low | High |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful translation requires careful selection of research materials that enable seamless transition to GMP manufacturing.
Table 6: Essential Research Reagents for Nucleic Acid Delivery Studies
| Reagent Category | Specific Examples | Research Function | GMP Transition Considerations |
|---|---|---|---|
| Nucleic Acid Cargo | siRNA, mRNA, plasmid DNA | Therapeutic payload | Switch from research-grade to GMP-grade with certified purity and endotoxin levels |
| Cationic Lipids | DOTAP, DLin-MC3-DMA, SM-102 | Nucleic acid complexation | Establish qualified suppliers with consistent composition and purity |
| Ionizable Lipids | DLin-MC3-DMA, ALC-0315 | LNP formation, endosomal escape | Select lipids with established regulatory precedent and safety profiles |
| PEGylated Lipids | DMG-PEG2000, ALC-0159 | Stability, pharmacokinetic modulation | Control PEG lipid content to balance stability and transfection efficiency |
| Helper Phospholipids | DSPC, DOPE | Membrane fusion, structural integrity | Ensure consistent fatty acid composition and phase transition behavior |
| Cationic Polymers | PEI, PLL, dendrimers | Nucleic acid condensation | Address cytotoxicity and biodegradability concerns for clinical translation |
| Targeting Ligands | Folate, GalNAc, antibodies, peptides | Cell-specific delivery | Establish conjugation chemistry and characterize ligand density and orientation |
Regulatory Pathways and Commercial Translation
Navigating regulatory requirements is a critical component of the bench-to-bedside transition that must be integrated early in the development process. Regulatory considerations fundamentally influence delivery system design, manufacturing strategy, and clinical trial planning.
Stage-Appropriate Regulatory Strategy
The regulatory pathway for nucleic acid therapeutics evolves significantly throughout the development lifecycle, requiring strategic planning and continuous adaptation.
Preclinical Stage:
- Focus on demonstrating product safety, toxicity, pharmacokinetics, and mechanism of action in GLP-accredited facilities [87]
- Manufacturing typically small-scale using open platforms and research-grade reagents
- Analytical methods may be qualitative but should demonstrate biological activity
Process Development/IND Stage:
- Implementation of phase-appropriate GMP principles per 21 CFR Part 210 [87]
- Transition toward closed workflows and GMP-grade reagents
- Development of standardized procedures and qualified equipment
- Demonstration of preliminary data on product safety, identity, purity, and potency
Commercial Stage:
- Full cGMP compliance per 21 CFR Parts 210-211 [87]
- Validated, closed-system workflows with defined PAR and NOR
- Process, equipment, and facility validation for scale-up/scale-out
- ICH Q2/Q14 qualified analytical methods and qualified suppliers
Analytical and Quality Control Requirements
Robust analytical characterization forms the foundation of regulatory submissions and quality control throughout the product lifecycle.
Critical Quality Attributes:
- Identity: Sequence confirmation, structural characterization
- Purity: Related substances, process impurities, product-related variants
- Potency: Biological activity relative to reference standard
- Quantity: Nucleic acid concentration, encapsulation efficiency
- Physical Properties: Particle size, polydispersity, zeta potential, morphology
- Stability: Real-time and accelerated stability under proposed storage conditions
Advanced Analytical Technologies: Early adoption of Process Analytical Technologies (PAT) enables real-time monitoring and quality control during manufacturing [87]. Implementation of orthogonal methods for key CQAs (e.g., combination of DLS, NTA, and MALS for size analysis) provides comprehensive product understanding expected by regulatory agencies.
Strategic Partnerships and Technology Platforms
CDMO Partnerships: Engaging with Contract Development and Manufacturing Organizations with established platform technologies can significantly accelerate development timelines by leveraging pre-existing master batch records, validated SOPs, and qualified analytical methods [87]. This approach reduces upfront investment and manufacturing failure risk while maintaining regulatory compliance.
Advanced Manufacturing Technologies: Early adoption of FDA Advanced Manufacturing Technology designated platforms can facilitate regulatory review and approval [2]. These include automated, closed-system platforms for cell therapy manufacturing, integrated processing systems, and digital control solutions compliant with 21 CFR Part 11 [87].
Figure 2: Regulatory Pathway Evolution - This diagram illustrates the progression of regulatory requirements from preclinical research through commercial manufacturing, highlighting key transitions and compliance milestones.
The successful bench-to-bedside translation of nucleic acid therapeutics requires careful integration of delivery system design, manufacturing strategy, and regulatory planning from the earliest stages of development. Targeted delivery systems offer enhanced specificity and potential therapeutic advantages but introduce complexity in manufacturing and characterization. Non-targeted approaches often provide simpler development pathways with more established regulatory precedents but may lack tissue specificity.
The choice between these strategies must be informed by comprehensive preclinical data, clear understanding of target product profile, and realistic assessment of manufacturing capabilities. By implementing QbD principles, engaging strategic partners early, and adopting phase-appropriate regulatory strategies, developers can navigate the complex translational pathway and advance promising nucleic acid therapeutics toward clinical application and commercial success.
As the field continues to evolve, emerging technologies in advanced manufacturing, digital integration, and analytical characterization will further enable the efficient translation of these innovative therapeutics, ultimately fulfilling their potential to address unmet medical needs through precise genetic intervention.
Conclusion
The successful clinical application of nucleic acid drugs is inextricably linked to the efficacy of their delivery systems. While non-targeted platforms like LNPs have proven revolutionary for vaccines and liver applications, the future lies in advancing targeted delivery to unlock treatments for extrahepatic tissues and complex diseases. The integration of smart material design, multi-stimuli responsiveness, and patient-specific targeting ligands will be pivotal. Future research must focus on overcoming endosomal escape inefficiencies, deepening our understanding of structure-activity relationships, and developing scalable manufacturing processes. The strategic selection and continuous optimization of delivery systems will ultimately determine the full potential of nucleic acid therapeutics in treating a vast array of genetic, oncological, and regenerative diseases.
References
- 1. Landscape of small nucleic acid therapeutics [https://www.nature.com/articles/s41392-024-02112-8]
- 2. Nucleic acid drugs: recent progress and future perspectives [https://www.nature.com/articles/s41392-024-02035-4]
- 3. Review Nucleic acid therapeutics: Past, present, and future [https://www.sciencedirect.com/science/article/pii/S2162253124003275]
- 4. Nucleic Acid Therapeutics Market Report 2025 [https://finance.yahoo.com/news/nucleic-acid-therapeutics-market-report-100600971.html]
- 5. Nucleic Acid Armor: Fortifying RNA Therapeutics through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11354913/]
- 6. Non-Viral Targeted Nucleic Acid Delivery: Apply Sequences ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7559072/]
- 7. RNA-Based Therapeutics: From Antisense Oligonucleotides to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7016530/]
- 8. RNAi vs. CRISPR: Guide to Selecting the Best Gene ... [https://www.synthego.com/blog/rnai-vs-crispr-guide/]
- 9. Small Nucleic Acid Drug Market 2025 Clinical Trials Rise [https://www.towardshealthcare.com/insights/small-nucleic-acid-drug-market-sizing]
- 10. Nucleic Acid Spotlights 2025 [https://www.insights.bio/nucleic-acid-insights/spotlights/year/2025]
- 11. Brewing nucleic acid therapies at the point of care [https://www.frontiersin.org/journals/science/articles/10.3389/fsci.2025.1625192/full]
- 12. Chitosan polyplexes for targeted gene delivery [https://www.sciencedirect.com/science/article/abs/pii/S0144861725008653]
- 13. The Fomivirsen, Patisiran, and Givosiran Odyssey [https://pubmed.ncbi.nlm.nih.gov/40186723/]
- 14. A delicate nucleic acid delivery system to be further explored [https://www.sciencedirect.com/science/article/abs/pii/S1748013224004420]
- 15. Cellular and biophysical barriers to lipid nanoparticle ... [https://www.nature.com/articles/s41467-025-60959-z]
- 16. Nanomedicine in cancer therapy | Signal Transduction and ... [https://www.nature.com/articles/s41392-023-01536-y]
- 17. Cellular and biophysical barriers to lipid nanoparticle ... [https://pubmed.ncbi.nlm.nih.gov/40595685/]
- 18. Engineered Bionanomaterials for Precision Delivery of ... [https://pubmed.ncbi.nlm.nih.gov/40898653/]
- 19. Trends in gene therapy delivery technologies [https://www.nature.com/articles/d41573-025-00171-2]
- 20. Recent Advance of Liposome Nanoparticles for Nucleic Acid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9864445/]
- 21. Recent Advances in Targeted Drug Delivery Strategy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10534854/]
- 22. Progress and challenges towards targeted delivery of ... [https://www.nature.com/articles/s41467-018-03705-y]
- 23. Advances in Antibody-Targeted Lipid Nanoparticles (Ab- ... [https://www.biochempeg.com/article/449.html]
- 24. Artificial Intelligence-Driven Strategies for Targeted Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389219/]
- 25. Advances in RNA-based therapeutics: current breakthroughs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592931/]
- 26. Breaking the mold with RNA—a “RNAissance” of life science [https://www.nature.com/articles/s41525-023-00387-4]
- 27. Advances in RNA-based therapeutics: current ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1675209/full]
- 28. RNA Therapeutics As We Enter 2025 Looking Beyond The ... [https://www.advancingrna.com/doc/rna-therapeutics-as-we-enter-2025-looking-beyond-the-horizon-of-first-generation-success-0001]
- 29. The current and future landscape of RNA-based therapies ... [https://www.nature.com/articles/s43856-025-01166-1]
- 30. Nanoparticle-Based Delivery Systems for Synergistic ... [https://www.mdpi.com/2306-5354/12/9/968]
- 31. Lipid-based nanoparticles external triggered release ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514795/]
- 32. Advances in Lipid-Polymer Hybrid Nanoparticles [https://www.mdpi.com/1424-8247/18/12/1772]
- 33. Lipid nanoparticles: a promising tool for nucleic acid ... [https://link.springer.com/article/10.1007/s12032-025-02939-3]
- 34. Advances in Inhaled Nanoparticle Drug Delivery for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598920/]
- 35. GalNAc-siRNA Conjugates: Leading the Way for Delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5994659/]
- 36. Delivery of Oligonucleotides to the Liver with GalNAc [https://pmc.ncbi.nlm.nih.gov/articles/PMC7403466/]
- 37. GalNAc conjugates: Delivery service to the liver! [https://www.bachem.com/articles/oligonucleotides/galnac-delivery-service-liver/]
- 38. Hepatocyte targeting via the asialoglycoprotein receptor [https://pubs.rsc.org/en/content/articlehtml/2025/md/d4md00652f]
- 39. siRNA Delivery: GalNAc Conjugates and LNPs [https://www.alnylam.com/our-science/sirna-delivery-platforms]
- 40. Current landscape of mRNA technologies and delivery ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-01080-z]
- 41. How nanotechnology can overcome current limitations in ... [https://www.diversatechnologies.com/how-nanotechnology-can-overcome-current-limitations-in-gene-editing-with-viral-vectors/]
- 42. Lipid Nanoparticles vs. Viral Vectors: A Comparison for ... [https://www.helixbiotech.com/post/lipid-nanoparticles-vs-viral-vectors-a-comparison-for-gene-therapy]
- 43. Viral and non-viral vectors in gene therapy: current state ... [https://www.sciencedirect.com/science/article/pii/S2352396425002786]
- 44. Adeno-Associated Viral (AAV) Vector Market Research ... [https://finance.yahoo.com/news/adeno-associated-viral-aav-vector-094300442.html]
- 45. Advancing AAV Vector Manufacturing: Challenges, ... [https://www.frontiersin.org/journals/molecular-medicine/articles/10.3389/fmmed.2025.1709095/full]
- 46. Vascular endothelial cell-targeted mRNA delivery via ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925007588]
- 47. Challenges in lentiviral vector production: retro ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1569298/full]
- 48. Nano Approaches to Nucleic Acid Delivery: Barriers, Solutions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11994986/]
- 49. Biomaterial-Based Nucleic Acid Delivery Systems for In ... [https://www.mdpi.com/1422-0067/26/15/7384]
- 50. Self-assembled inorganic nanomaterials for biomedical ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04537h]
- 51. Inorganic-Based Nanoparticles and Biomaterials as ... [https://www.mdpi.com/2304-6740/12/11/292]
- 52. Biomaterial scaffolds for therapeutic immune cell ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006947]
- 53. Nucleic Acid Nanostructures 2025-2033 Overview [https://www.datainsightsmarket.com/reports/nucleic-acid-nanostructures-495749]
- 54. Nucleic Acid Nanostructures 2025-2033 Analysis [https://www.archivemarketresearch.com/reports/nucleic-acid-nanostructures-19162]
- 55. mRNA medicine: Recent progresses in chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311907/]
- 56. Engineering Nanoparticles for Targeted Delivery of Nucleic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6197778/]
- 57. The current landscape of nucleic acid therapeutics [https://www.nature.com/articles/s41565-021-00898-0]
- 58. Nanoparticle targeting: Review of passive and active ... [https://insidetx.com/resources/reviews/a-comprehensive-review-of-passive-and-active-nanoparticle-targeting-technics/]
- 59. Artificial intelligence in smart drug delivery systems [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00089k]
- 60. DNA nanocarriers for nucleic acid drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462906/]
- 61. Endosomal escape of RNA therapeutics: How do we solve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10019367/]
- 62. Endosomal escape mechanisms of extracellular vesicle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11648457/]
- 63. Unravelling cytosolic delivery of cell penetrating peptides ... [https://www.nature.com/articles/s41467-021-23997-x]
- 64. Endosomal escape and cytosolic penetration of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6561124/]
- 65. The impact of lipid compositions on siRNA and mRNA ... [https://pubmed.ncbi.nlm.nih.gov/40571267/]
- 66. Off-target effects of oligonucleotides and approaches ... [https://www.sciencedirect.com/science/article/pii/S2472555225000474]
- 67. Advanced strategies for nucleic acids and small-molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9910002/]
- 68. Mitigating off-target effects in CRISPR/Cas9-mediated in vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7220873/]
- 69. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 70. Enhancing non-viral DNA delivery systems [https://www.sciencedirect.com/science/article/pii/S0168365924008459]
- 71. Biomaterials for Drug Delivery and Human Applications [https://www.mdpi.com/1996-1944/17/2/456]
- 72. Design strategies and applications of circulating cell-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4428174/]
- 73. Advances in drug delivery systems, challenges and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10320272/]
- 74. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 75. Transfection Technologies for Next-Generation Therapies [https://www.mdpi.com/2077-0383/14/15/5515]
- 76. Microfluidic Platforms for Ex Vivo and In Vivo Gene Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384408/]
- 77. Tissue nanotransfection and cellular reprogramming in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1558735/full]
- 78. The CRISPR therapeutics landscape in 2025 [https://www.kilburnstrode.com/knowledge/european-ip/the-crispr-therapeutics-landscape-in-2025]
- 79. Non-cationic carriers for siRNA delivery: Current progress ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925009769]
- 80. Systematic analysis of siRNA and mRNA features impacting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205987/]
- 81. Precision gene editing: The power of CRISPR-Cas in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590234/]
- 82. RNA Therapeutics: Delivery Problems and Solutions—A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567017/]
- 83. The Path from Bench to Bedside: Considerations before ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4255460/]
- 84. The powerful world of antisense oligonucleotides: From bench ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9285911/]
- 85. Advances in nucleic acid therapeutics: structures, delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11358240/]
- 86. Drug delivery systems: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3465154/]
- 87. Bridging preclinical to commercial manufacturing in cell ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3605/bridging-preclinical-to-commercial-manufacturing-in-cell-therapy-mind-the-gap]