Peptide Nucleic Acids: Revolutionizing Therapeutics and Diagnostics with Next-Generation Biomolecules
This article provides a comprehensive overview of Peptide Nucleic Acid (PNA) technology, a synthetic nucleic acid analog with a unique polyamide backbone, and its groundbreaking applications in biomedicine.
Peptide Nucleic Acids: Revolutionizing Therapeutics and Diagnostics with Next-Generation Biomolecules
Abstract
This article provides a comprehensive overview of Peptide Nucleic Acid (PNA) technology, a synthetic nucleic acid analog with a unique polyamide backbone, and its groundbreaking applications in biomedicine. Tailored for researchers, scientists, and drug development professionals, we explore PNA's foundational chemistry, which confers exceptional binding affinity, specificity, and stability against enzymatic degradation. The scope spans methodological applications in antisense therapy, gene editing, and molecular diagnostics, alongside a critical analysis of delivery challenges and optimization strategies. Finally, we present a comparative validation against other oligonucleotide technologies and discuss the burgeoning market and clinical pipeline, offering a holistic view of PNA's potential to bridge the gap between laboratory innovation and clinical impact.
Unlocking the Structure and Mechanism: The Foundational Science of PNAs
Peptide Nucleic Acid (PNA) represents a fundamental redesign of natural nucleic acids, replacing the ubiquitous sugar-phosphodiester backbone with a synthetic backbone composed of repeating N-(2-aminoethyl)glycine units [1] [2]. First introduced by Nielsen and colleagues in 1991, this structural alteration creates a DNA/RNA mimic that retains the nucleobase spacing of natural nucleic acids but operates with a functionally distinct, electrostatically neutral pseudopeptide scaffold [2] [3]. The nucleobases (adenine, guanine, cytosine, and thymine) are attached to this backbone via a carboxymethyl linker, preserving the Watson-Crick base-pairing rules essential for molecular recognition [1] [4]. This application note elucidates the critical differences between the N-(2-aminoethyl)glycine and phosphodiester backbones, providing researchers with structured data, validated protocols, and practical tools for deploying PNA technology in therapeutic and diagnostic development.
Structural Backbone Comparison and Biophysical Consequences
The replacement of the deoxyribose-phosphodiester backbone with N-(2-aminoethyl)glycine units confers a unique set of biophysical and biological properties that make PNA a powerful tool for research and development.
Table 1: Comparative Analysis: N-(2-aminoethyl)glycine vs. Phosphodiester Backbone
| Characteristic | N-(2-aminoethyl)glycine PNA Backbone | Natural Phosphodiester Backbone |
|---|---|---|
| Chemical Structure | Repetitive pseudopeptide units; Polyamide chain [1] | Alternating sugar (deoxyribose) and phosphate groups [2] |
| Electrostatic Charge | Neutral [2] [3] [4] | Negatively charged (per phosphate group) |
| Hybridization Affinity | High affinity and stability (e.g., 15-mer PNA/DNA duplex Tm ~70°C) [1]. Less sensitive to ionic strength [2]. | Lower inherent stability (e.g., analogous DNA/DNA duplex Tm ~55°C) [1]. Stability is salt-dependent. |
| Sequence Specificity | Excellent mismatch discrimination; highly sequence-selective [2] [5] | Good specificity, but generally lower single-base mismatch discrimination than PNA |
| Biostability | Resistant to nucleases and proteases [1] [2] [4]; stable in biological fluids. | Susceptible to degradation by ubiquitous nucleases. |
| Solubility | Can have poor aqueous solubility due to neutral character; often requires chemical modification [4]. | Good aqueous solubility due to charged phosphate backbone. |
The neutral character of the PNA backbone is its most transformative feature. By eliminating the negative charges present on the phosphodiester backbone, PNA hybridizes with complementary DNA or RNA without electrostatic repulsion, leading to significantly higher thermal stability of the resulting duplexes [2] [4]. Furthermore, because enzymes like nucleases and proteases are highly specific for their natural substrates, the unnatural PNA backbone is not recognized, granting it remarkable stability against enzymatic degradation in serum and cell extracts [1] [4]. This combination of high binding affinity, superior specificity, and biostability makes PNA an exceptional candidate for developing robust antisense agents, diagnostic probes, and antigene therapeutics.
Experimental Protocols for PNA Utilization
Protocol 1: Solid-Phase Synthesis of PNA Oligomers
The peptide-like nature of the N-(2-aminoethyl)glycine backbone allows PNA oligomers to be synthesized using standard Solid-Phase Peptide Synthesis (SPPS) methodologies, either manually or via automated synthesizers [1] [4].
Key Materials:
- Resin: Merrifield resin or other suitable solid support [1].
- PNA Monomers: N-2-aminoethylglycine monomers with nucleobases (A, G, C, T), protected at the N-terminus with groups such as Boc (tert-butyloxycarbonyl) or Fmoc (9-fluorenylmethoxycarbonyl) [1] [4].
- Deprotection Reagents: Trifluoroacetic acid (TFA) for Boc removal, or piperidine for Fmoc removal [1].
- Cleavage Reagents: TFA or 4-trifluoromethyl salicylic acid (TFMSA) to cleave the oligomer from the resin and remove protecting groups [1].
- Purification & Analysis: Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) for purification; High-Resolution Mass Spectrometry (HRMS) with MALDI or TOF for characterization [1].
Workflow:
- Attachment: The C-terminus of the first PNA monomer is covalently attached to the solid-phase resin.
- Deprotection: The N-terminal protecting group (PG1) is removed using a suitable reagent like TFA.
- Coupling: The next PNA monomer is activated and coupled to the free N-terminus of the growing chain.
- Repetition: Steps 2 and 3 are repeated until the full-length sequence is assembled.
- Cleavage & Global Deprotection: The completed PNA oligomer is cleaved from the resin, and all remaining protecting groups (PG2) are removed using a strong acid cocktail like TFMSA/TFA.
- Purification & Characterization: The crude PNA is purified via RP-HPLC and its identity confirmed by HRMS [1].
Protocol 2: Evaluating PNA-DNA Hybridization Using UV Melting Curve Analysis (Thermal Denaturation)
This protocol determines the thermal melting temperature (T~m~), a key metric for assessing the affinity and specificity of a PNA oligomer for its complementary nucleic acid target.
Key Materials:
- Purified PNA Oligomer (from Protocol 1).
- Complementary DNA or RNA Target (purified).
- UV-Visible Spectrophotometer equipped with a temperature-controlled Peltier cell.
- Quartz Cuvettes with a path length suitable for nucleic acid analysis.
- Buffer: Typically a low-salt buffer (e.g., 10 mM sodium phosphate, pH 7.0) to highlight the salt-independent binding of PNA [2].
Workflow:
- Sample Preparation: Combine the PNA strand and its complementary DNA target in equimolar ratios in buffer to form a duplex. A typical concentration for each strand is 1-4 µM.
- Denaturation and Renaturation: Heat the sample to 90°C for 5 minutes and then cool slowly to room temperature to ensure proper duplex formation.
- Data Acquisition: Place the sample in the spectrophotometer and set the temperature ramp (e.g., from 20°C to 90°C at a rate of 0.5°C/min). Monitor the absorbance at 260 nm continuously.
- Data Analysis: Plot the absorbance versus temperature to generate a melting curve. The T~m~ is defined as the temperature at the midpoint of the transition from double-stranded to single-stranded states, which can be determined from the first derivative of the melting curve.
- Interpretation: A higher T~m~ indicates a more stable duplex. Compare the T~m~ of the PNA/DNA duplex with that of the native DNA/DNA duplex of the same sequence. The PNA/DNA duplex is expected to have a significantly higher T~m~, demonstrating enhanced binding affinity [1] [2]. The effect of single-base mismatches on T~m~ can also be quantified to evaluate specificity.
Diagram 1: PNA Synthesis and Analysis Workflow. This diagram outlines the key experimental steps for synthesizing PNA oligomers (top) and for evaluating their binding to complementary DNA targets (bottom).
Advanced Backbone Modifications for Enhanced Performance
While the standard PNA backbone possesses excellent properties, it can be rationally modified to address limitations such as ambiguous binding orientation, poor aqueous solubility, and suboptimal cellular uptake.
Table 2: Common Strategies for PNA Backbone Modification
| Modification Strategy | Example Structures | Impact on PNA Properties |
|---|---|---|
| Introduction of Chirality (αPNA) | PNA with D- or L-lysine side chains [2] [5] | Imparts a preferred handedness, enhances DNA binding specificity, and can improve solubility. D-lysine modifications often stabilize PNA-DNA duplexes [5]. |
| Conformational Constraint | Cyclopentyl, cyclohexyl, or proline-derived PNAs (e.g., pyrrolidine PNA) [1] [2] [5] | Pre-organizes the PNA backbone, reducing entropy loss upon binding. This often leads to increased binding affinity and enhanced mismatch discrimination [5]. |
| Cationic Functionalization | Phosphono PNA, Guanylated PNA [2] | Introduces positive charges to the backbone, significantly improving water solubility and enhancing cellular uptake through interactions with the negatively charged cell membrane [2]. |
| γ-Backbone Substitution | γ-substituted PNAs (e.g., from γ-lysine) [1] | Allows pre-organization of the backbone without steric clash with the target. Can dramatically improve binding affinity for both DNA and RNA targets. |
These modifications are synthesized by incorporating chemically altered monomers during solid-phase synthesis. For instance, a "chiral box" of three consecutive D-lysine-modified PNA units can enforce an exclusive antiparallel binding mode to DNA, which is the most stable orientation [5]. The choice of modification is application-dependent: constrained PNAs are ideal for targeting highly structured RNA, while cationic PNAs are better suited for cellular assays where uptake is a limiting factor.
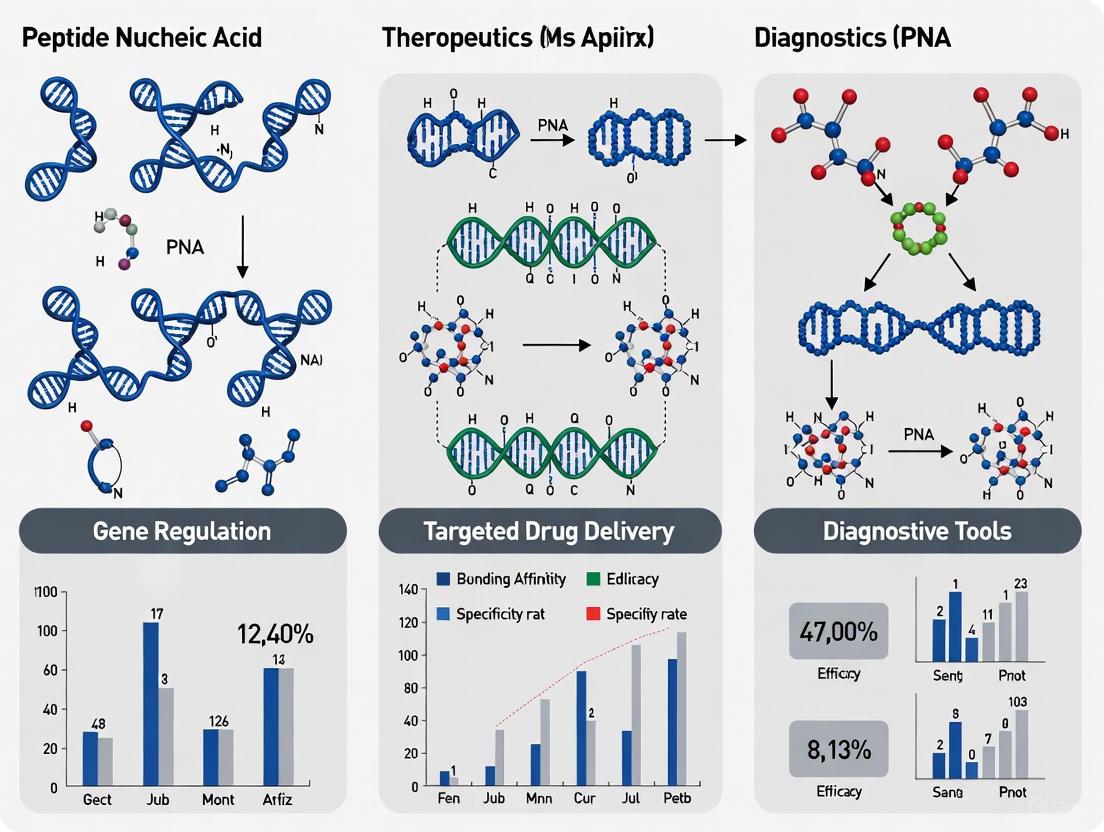
PNA Applications in Therapeutics and Diagnostics
The unique properties of the N-(2-aminoethyl)glycine backbone enable PNA to be deployed across a wide spectrum of biomedical applications.
Therapeutic Applications
- Antisense and Antigene Therapy: PNA binds to mRNA to block translation (antisense) or invades duplex DNA to form stable PNA-DNA-PNA triplexes, inhibiting transcription (antigene) [2] [4]. For example, antisense PNAs have been used to restore antibiotic sensitivity in methicillin-resistant S. aureus (MRSA) by targeting resistance genes [1].
- Anti-cancer and Anti-viral Agents: PNA oligomers have been designed to inhibit oncogenes like c-myc and bcl-2, or to target essential regions of viral genomes such as HIV-1 [1] [6]. A Tat-PNA conjugate demonstrated efficacy in inhibiting Hepatitis B virus replication in HepG2 cells [1].
- Splicing Modulation: Similar to other steric-blocking oligonucleotides, PNA can be designed to bind pre-mRNA and modulate splicing, potentially correcting defective splicing in genetic diseases [4].
Diagnostic Applications
- Biosensors and Mutation Detection: The superior mismatch discrimination of PNA makes it an excellent probe for detecting single-nucleotide polymorphisms (SNPs) and point mutations [2]. PNA-based fluorescence in situ hybridization (FISH) probes are used for the rapid identification of pathogens like S. aureus [1].
- PCR Clamping: A PNA oligomer designed to bind the wild-type DNA template with high affinity can block PCR amplification, enriching for the amplification of mutant sequences, which is useful for detecting oncogenic mutations in EGFR [1].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for PNA Work
| Reagent / Material | Function / Application | Notes |
|---|---|---|
| Boc- or Fmoc-Protected PNA Monomers | Building blocks for PNA oligomer synthesis [1]. | Available from specialized chemical suppliers (e.g., Panagene, Link Technologies). |
| Cell-Penetrating Peptides (CPPs) | Conjugation partners to enhance cellular delivery of PNA [4] [6]. | Common examples: Penetratin, Transportan, oligo-arginine (R~8~). |
| Cationic Lipids / Transfection Reagents | Alternative method for in vitro PNA delivery into cells [4]. | Useful for screening PNA activity prior to covalent CPP conjugation. |
| Endosomolytic Agents (e.g., Chloroquine) | Co-treatment to enhance endosomal escape of internalized PNA [4]. | Critical for improving biological efficacy of CPP-PNA conjugates that enter via endocytosis. |
| PNA-Resin | Solid support for PNA synthesis [1]. | Compatible with standard peptide synthesizers. |
Diagram 2: PNA Delivery Strategies. This diagram illustrates the three primary strategies for delivering PNA into cells: covalent conjugation to Cell-Penetrating Peptides (CPPs), encapsulation within Lipid Nanoparticles (LNPs), and complexation with cationic lipid reagents.
Peptide Nucleic Acids (PNAs) represent a powerful class of synthetic oligonucleotide analogues whose unique physicochemical properties—a neutral pseudopeptide backbone, elevated thermal stability with complementary nucleic acids, and pronounced resistance to enzymatic degradation—make them exceptionally suitable for advanced therapeutic and diagnostic applications. This application note details the experimental characterization of these core properties and provides standardized protocols for leveraging them in research and development. Aimed at scientists and drug development professionals, this document serves as a practical guide for incorporating PNA technology into novel biosensors, antisense therapeutics, and molecular genetic assays.
Property Analysis and Experimental Characterization
Neutral Charge and Its Consequences
The foundational feature of PNA is its backbone, composed of N-(2-aminoethyl)glycine units, which replaces the native sugar-phosphodiester backbone of DNA and RNA [7] [4]. This structural redesign eliminates the negatively charged phosphate groups present in natural nucleic acids.
Key Experimental Findings:
- Stronger Hybridization Affinity: The neutral backbone removes the electrostatic repulsion that occurs between two negatively charged DNA or RNA strands. This results in significantly higher affinity and stability of PNA-DNA and PNA-RNA duplexes compared to their natural counterparts [8] [9].
- Salt-Independent Hybridization: Unlike DNA-DNA duplexes, whose stability is highly dependent on ionic strength to shield the negative charges, PNA-nucleic acid hybridization is largely independent of salt concentration [10] [4]. This property is particularly advantageous for assays run under variable or low-salt conditions.
Table 1: Impact of Neutral Backbone on PNA Properties
| Property | Comparison to Natural Nucleic Acids | Experimental Implication |
|---|---|---|
| Binding Affinity | Higher affinity for complementary DNA/RNA [11] | Effective use of shorter probes (13-18 bases) [12] |
| Electrostatic Interaction | No electrostatic repulsion [7] | Hybridization efficiency is consistent across different buffer ionic strengths [10] |
| Solubility & Aggregation | Can form globular structures and aggregate due to hydrophobicity [7] | Requires modification (e.g., lysine conjugation, "miniPEG") for some applications [7] |
High Thermal Stability (Tm)
The thermal stability of a nucleic acid duplex is quantified by its melting temperature (Tm). PNA-containing duplexes consistently demonstrate higher Tm values than equivalent DNA-DNA or DNA-RNA duplexes.
Quantitative Data:
- A PNA-DNA duplex typically has a ~1°C higher Tm per base pair than the corresponding DNA-DNA duplex [11].
- PNA-RNA duplexes are even more stable, often exhibiting a Tm a few degrees higher than PNA-DNA duplexes [10] [11].
- In a representative study, a 10-mer PNA-RNA duplex was found to be more thermally stable than both the corresponding RNA-RNA duplex and the PNA-PNA duplex [10].
Experimental Protocol: UV-Monitored Thermal Denaturation
Principle: This protocol determines the melting temperature (Tm) and thermodynamic parameters of a PNA-nucleic acid duplex by measuring its absorbance at 260 nm as a function of temperature.
Reagents:
- Complementary PNA and DNA/RNA strands
- Phosphate buffer (10 mM, pH 7.0)
- Sodium Chloride (NaCl, 20 mM)
Procedure:
- Sample Preparation: Dissolve complementary PNA and nucleic acid strands in the desired buffer to a final concentration of 4 µM each strand [10].
- Denaturation and Annealing: Heat the sample to 95°C for 5 minutes and allow it to cool slowly to room temperature to ensure proper duplex formation.
- UV Spectrophotometry Measurement: Place the sample in a quartz cuvette in a UV-Vis spectrophotometer equipped with a temperature controller. Set the wavelength to 260 nm.
- Data Collection: Increase the temperature from a low (e.g., 20°C) to a high value (e.g., 95°C) at a controlled rate (e.g., 0.5-1.0°C/min) while continuously recording the absorbance.
- Data Analysis:
- Plot the absorbance vs. temperature to generate a melting curve.
- Normalize the data and fit it to a two-state model with sloping baselines to calculate the fraction of bound molecules (f) as a function of temperature [10].
- The Tm is defined as the temperature where f(T) = 0.5.
- Thermodynamic parameters (ΔH, ΔS) can be derived by fitting the data to the van't Hoff equation [10].
Nuclease and Protease Resistance
The unnatural polyamide backbone of PNA is not a substrate for enzymes that degrade natural biomolecules.
Key Evidence:
- PNAs are resistant to degradation by nucleases (DNases, RNases) and proteases [11] [7] [4].
- This resistance confers extended in vitro and in vivo stability, overcoming a major limitation of natural DNA and RNA oligonucleotides in therapeutic and diagnostic applications [7] [4].
Experimental Protocol: Serum Stability Assay
Principle: This protocol assesses the stability of PNA oligomers in biologically relevant media by incubating them with serum and analyzing integrity over time.
Reagents:
- PNA oligomer (and a control DNA oligomer)
- Fetal Bovine Serum (FBS) or human serum
- Proteinase K
- Phenol/Chloroform/Isoamyl Alcohol
- Denaturing Polyacrylamide Gel Electrophoresis (PAGE) system
Procedure:
- Incubation Setup: Dilute the PNA and control DNA in a solution containing 50% FBS. Incubate the mixture at 37°C.
- Sampling: Withdraw aliquots at predetermined time points (e.g., 0, 1, 2, 4, 8, 24 hours).
- Reaction Termination: For each aliquot, digest serum proteins by adding Proteinase K, followed by extraction with phenol/chloroform/isoamyl alcohol to isolate the nucleic acids.
- Analysis: Analyze the extracted oligomers using denaturing PAGE. The intact PNA will show a distinct band, while the degraded DNA control will show a smeared or disappearing band over time.
- Quantification: Use gel imaging software to quantify the intensity of the full-length band relative to the time-zero sample to determine the half-life of the oligomer.
Table 2: Summary of Key Physicochemical Properties and Applications
| Property | Structural Basis | Experimental Advantage | Primary Application Areas |
|---|---|---|---|
| Neutral Charge | N-(2-aminoethyl)glycine backbone [7] | Enhanced binding affinity and specificity; salt-independent hybridization [9] | Biosensors; Antisense/Antigene therapy; FISH probes [8] [13] |
| High Thermal Stability (Tm) | Lack of electrostatic repulsion and flexible backbone [8] | Superior mismatch discrimination; robust performance in assays [8] [10] | PCR clamping; Microarray probes; Gene targeting [8] [7] |
| Nuclease/Protease Resistance | Unnatural, synthetic backbone [7] | Long shelf-life and extended stability in biological fluids [4] | Therapeutic oligonucleotides; Diagnostic probes for complex samples [14] [7] |
Diagnostic and Therapeutic Workflows
The following diagrams illustrate how the key properties of PNA are integrated into practical research and diagnostic applications.
The Scientist's Toolkit: Research Reagent Solutions
Successful experimentation with PNAs requires a specific set of reagents and materials. The following table details key components for working with PNAs in a therapeutic context, particularly focusing on delivery, which is a recognized challenge.
Table 3: Essential Reagents for PNA-Based Research
| Reagent/Material | Function/Description | Application Notes |
|---|---|---|
| Custom PNA Oligomers | Synthetic PNA sequences, typically 13-20 bases in length [11]. | Can be synthesized via Fmoc/tBoc solid-phase peptide synthesis [15]. Often purchased from specialized vendors (e.g., Panagene). |
| Cell-Penetrating Peptides (CPPs) | Short cationic peptides (e.g., TP10, Tat, Penetratin) that facilitate cellular uptake of conjugated PNA [14] [7]. | Can be covalently linked to PNA. TP10 has been shown to be highly effective in comparative studies [14]. |
| Nuclear Localization Signal (NLS) | A peptide sequence (e.g., PKKKRKV) conjugated to PNA to direct it to the cell nucleus [14]. | Essential for antigene applications where the target is genomic DNA. |
| Cationic Lipids / Nanoparticles | Non-viral delivery vehicles that complex with neutral PNA to improve cellular uptake and in vivo bioavailability [7] [4]. | Used for both in vitro and in vivo delivery. Help overcome rapid excretion of free PNA. |
| Endosomolytic Agents (e.g., Chloroquine) | Compounds that disrupt endosomal membranes, enhancing the release of internalized PNA-CPP conjugates into the cytosol [4]. | Co-treatment can dramatically increase the biological efficacy of PNA. |
Concluding Remarks
The distinct physicochemical profile of PNAs—governed by their neutral charge, high thermal stability, and nuclease resistance—provides a compelling advantage over natural oligonucleotides for designing next-generation research tools and therapeutics. While challenges in cellular delivery persist, conjugation to CPPs and formulation in advanced nano-delivery systems provide robust solutions. By adhering to the standardized protocols and leveraging the recommended reagent toolkit outlined in this document, researchers can effectively harness the power of PNA technology to drive innovation in molecular diagnostics and gene-targeted therapies.
Peptide Nucleic Acids (PNAs) are synthetic oligonucleotide analogues that have emerged as powerful tools in therapeutic and diagnostic research. Their unique polyamide backbone, replacing the sugar-phosphate backbone of natural nucleic acids, confers exceptional binding affinity and stability towards DNA and RNA targets [4] [1]. This application note details the core mechanisms of action—splicing modulation and translational blockade—through which PNAs exert their biological effects, providing structured protocols and data for research scientists and drug development professionals.
Core Mechanism I: Splicing Modulation
Splicing modulation involves the targeted correction of aberrant pre-mRNA splicing, a process implicated in numerous genetic disorders and cancers [16] [17]. PNA molecules designed for this application are typically targeted to specific pre-mRNA sequences to influence splice site selection.
Mechanism of Action
RNA splicing is executed by the spliceosome, a dynamic complex of five small nuclear ribonucleoproteins (snRNPs: U1, U2, U4, U5, U6) and approximately 200 associated proteins [16] [17]. The process requires recognition of key cis-regulatory elements: the 5' splice site (5'ss), 3' splice site (3'ss), branch point sequence (BPS), and polypyrimidine tract (PPT) [16] [17] [18]. Splicing factors, including serine/arginine-rich (SR) proteins and heterogeneous nuclear ribonucleoproteins (hnRNPs), bind to enhancer or silencer elements (ESEs, ESSs, ISEs, ISSs) to either promote or repress exon inclusion [16] [17].
Splice-switching PNAs act by sterically blocking access to these critical regulatory sequences or splicing factor binding sites. By hybridizing to their target pre-mRNA with high affinity and specificity, they prevent the assembly of the spliceosomal complex, leading to altered exon inclusion or exclusion in the final mature mRNA [4] [18]. This can result in the restoration of a disrupted reading frame, exclusion of a pathogenic exon, or inclusion of a compensatory exon.
The following diagram illustrates the mechanistic basis of PNA-mediated splicing modulation.
Quantitative Data on Splicing Modulation
Table 1: Selected Examples of PNA-Mediated Splicing Modulation in Research
| Target Gene | Disease Model | PNA Target Site | Observed Splicing Effect | Reference |
|---|---|---|---|---|
| Dystrophin | Duchenne Muscular Dystrophy (mdx mice) | Mutation site in muscle stem cells | Genomic correction of point mutation, restoring reading frame | [4] |
| β-globin (IVS2-654) | β-thalassaemia (transgenic mouse) | Intronic mutation | Correction of aberrant splicing, induced DNA repair | [4] |
| COL7A1 | Dominant Dystrophic Epidermolysis Bullosa | Mutant allele | Inhibition of mutant transcript transcription | [4] |
| SMN2 | Spinal Muscular Atrophy | N/A | Exon inclusion to produce functional SMN protein (Conceptual, cf. Nusinersen) | [18] |
Experimental Protocol: PNA-Based Splicing Modulation
Objective: To evaluate the efficacy of a PNA oligomer in modulating splicing of a target pre-mRNA in cell culture.
Materials & Reagents:
- Splice-Switching PNA: Designed to target a specific splice site or splicing regulatory element.
- Cell-Penetrating Peptide (CPP): e.g., (RXR)4XB or Tat, for conjugation to PNA to enhance delivery [4].
- Cationic Transfection Reagent: For complexing with PNA-CPP conjugates if needed.
- Cell Line: Stably expressing the target pre-mRNA or a splicing reporter minigene.
- Control PNA: Scrambled sequence or sense-targeting PNA.
- Total RNA Extraction Kit, Reverse Transcription Kit, PCR Master Mix, Agarose Gel Electrophoresis System.
Method:
- PNA Design and Conjugation:
- Design a 15-18 mer anti-sense PNA to be complementary to the target pre-mRNA sequence (e.g., 5' or 3' splice site, ESE, or ISS).
- Synthesize the PNA oligomer using Fmoc/tBoc solid-phase protocols [1].
- Conjugate the PNA to a CPP (e.g., via a disulfide or non-cleavable maleimide linkage) to facilitate cellular uptake [4].
Cell Seeding and Transfection:
- Seed appropriate cells (e.g., HEK293, HeLa, or patient-derived fibroblasts) in a 12-well plate to reach 60-80% confluency at the time of transfection.
- Prepare PNA-CPP complexes in serum-free medium. A common working concentration is 1-10 µM. Incubate for 30 minutes.
- Replace cell culture medium with the complex-containing medium. Co-treat with 100 µM chloroquine to enhance endosomal escape, if necessary [4].
- Incubate cells for 24-48 hours. Include a negative control (untreated cells) and a scramble PNA control.
RNA Analysis:
- Harvest cells and extract total RNA using a commercial kit.
- Synthesize cDNA using a reverse transcription kit with oligo(dT) or random hexamer primers.
- Perform PCR with primers flanking the alternatively spliced region of interest.
- Analyze PCR products by agarose gel electrophoresis. A shift in product size indicates successful splicing modulation.
- For quantitative analysis, perform RT-qPCR with assays specific for different splice variants.
Troubleshooting:
- Low Efficiency: Optimize PNA concentration, transfection time, or try different CPPs.
- Cytotoxicity: Titrate down PNA concentration and check cell viability with MTT assay.
- No Splicing Change: Verify PNA target specificity and binding affinity via melting temperature (Tm) analysis.
Core Mechanism II: Translational Blockade
Translational blockade, primarily achieved through the antisense mechanism, involves the direct inhibition of mRNA translation into protein by obstructing the ribosomal machinery.
Mechanism of Action
PNAs designed for translational blockade are typically anti-sense oligomers targeted to the translational start site (AUG codon) or coding regions of an mRNA [4]. Due to their high-affinity hybridization and neutral backbone, PNA:RNA duplexes form stable, irreversible complexes that are not recognized by cellular enzymes like RNase H.
The mechanism is primarily steric hindrance. The bound PNA creates a physical barrier that prevents the scanning ribosomal pre-initiation complex from progressing along the mRNA, thereby blocking the initiation of translation [4]. Furthermore, the stable PNA:RNA duplex can also hinder the elongation phase of translation by obstructing the movement of the ribosome. This direct physical blockade leads to a potent and specific downregulation of the corresponding protein product.
The diagram below outlines the process of translational blockade by antisense PNAs.
Quantitative Data on Translational Blockade (Antisense)
Table 2: Selected Examples of PNA-Mediated Translational Blockade (Antisense)
| Target Gene/RNA | Disease Model | PNA Type / Conjugate | Observed Effect | Reference |
|---|---|---|---|---|
| miR-155 | Lymphomas (mice) | Antisense PNA | Inhibition of the oncomiR-155 | [4] |
| miR-221 | Breast Cancer (MCF-7 & MDA-MB-231 cells) | Antisense PNA | Inhibition of onco miR-221 | [4] |
| HBV RNA | Hepatitis B (mouse model) | Antisense PNA (targeting LTR) | Significant decline in HBV DNA levels | [4] |
| RAD51 | Multiple Myeloma (mouse model) | Antigene PNA | Inhibition of RAD51 protein expression | [4] |
| MYCN | Rhabdomyosarcoma | Antigene PNA | Reduction of MYCN expression | [4] |
| bcl-2 | Lymphocytic Lymphoma | 177Lu DOTA-anti-bcl-2-PNA-peptide | Inhibition of bcl-2 proteins | [1] |
Experimental Protocol: Assessing Antisense PNA Efficacy
Objective: To determine the protein knockdown efficiency of an antisense PNA in a mammalian cell line.
Materials & Reagents:
- Antisense PNA: Targeted to the AUG start codon region of the mRNA of interest.
- Control PNA: Mismatch or scrambled sequence PNA.
- Delivery Vehicle: CPP conjugate or cationic lipid-based transfection reagent.
- Cell Line: Endogenously or recombinantly expressing the target protein.
- Antibodies: Primary antibody against the target protein and a loading control (e.g., GAPDH, β-Actin).
- Western Blotting System (SDS-PAGE gel, transfer apparatus, ECL reagent).
Method:
- PNA Design and Preparation:
- Design a 15-17 mer PNA complementary to the region encompassing the AUG start codon of the target mRNA.
- Procure or synthesize the PNA, preferably conjugated to a CPP (e.g., R8) for efficient delivery.
Cell Treatment and Incubation:
- Seed cells in a 6-well plate and culture until 50-70% confluent.
- Treat cells with the PNA-CPP conjugate at a final concentration of 2-5 µM in serum-free or complete medium. Include untreated and scrambled PNA controls.
- Incubate cells for 48-72 hours to allow for turnover of the existing target protein.
Protein Analysis by Western Blot:
- Lyse cells using RIPA buffer supplemented with protease inhibitors.
- Quantify protein concentration using a BCA or Bradford assay.
- Separate equal amounts of protein (20-40 µg) by SDS-PAGE and transfer to a PVDF membrane.
- Block the membrane with 5% non-fat milk in TBST for 1 hour.
- Incubate with primary antibody (diluted as per manufacturer's instructions) overnight at 4°C.
- Wash the membrane and incubate with an HRP-conjugated secondary antibody for 1 hour at room temperature.
- Develop the blot using ECL reagent and visualize. Quantify band intensity relative to the loading control.
Troubleshooting:
- Inefficient Knockdown: Increase PNA concentration or treatment duration. Verify PNA binding affinity and delivery efficiency.
- Off-Target Effects: Perform RNA-Seq or profile a panel of unrelated proteins to confirm specificity of the antisense PNA.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for PNA-Based Splicing and Translation Research
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| PNA Oligomers | Core molecule for target engagement. | Custom synthesis via Fmoc/tBoc SPS [1]. Purify via RP-HPLC, characterize by MALDI-TOF MS. |
| Cell-Penetrating Peptides (CPPs) | Enhances cellular uptake of PNA. | Oligoarginine (R8), Tat peptide, (RXR)4XB [4]. Conjugate via maleimide chemistry. |
| Cationic Lipids / Transfection Reagents | Alternative delivery method for PNA. | Useful for in vitro delivery, especially of PNA without CPP conjugation. |
| Endosomolytic Agents | Promotes endosomal escape of internalized PNA. | Chloroquine; use as a co-treatment to enhance biological activity [4]. |
| Splicing Reporter Minigene | Validates splice-switching PNA activity. | Plasmid containing genomic region of interest with alternative exons; co-transfect with PNA. |
| Lipid Nanoparticles (LNPs) | Advanced in vivo delivery vehicle. | Composed of ionizable lipids, phospholipids, cholesterol, PEG-lipids for systemic PNA delivery [19]. |
The dual mechanisms of splicing modulation and translational blockade underscore the versatility and potency of PNAs as research tools and therapeutic agents. Their high binding affinity, specificity, and metabolic stability provide distinct advantages over other oligonucleotide chemistries. The protocols and data summarized herein offer a foundational framework for researchers developing PNA-based applications, from initial proof-of-concept studies to advanced pre-clinical investigations. Continued advancements in PNA delivery, particularly through CPP and LNP technologies, are poised to further unlock their potential in precision medicine.
Non-coding RNAs (ncRNAs) represent a vast category of functional RNA molecules that do not translate into proteins but play crucial regulatory roles in gene expression. Once considered "junk DNA," ncRNAs are now recognized as master regulators of cellular processes, influencing transcription, post-transcription, and epigenetic modifications [20] [21]. The two principal classes of ncRNAs include small ncRNAs (such as microRNAs and small interfering RNAs) and long non-coding RNAs (lncRNAs) exceeding 200 nucleotides in length [22] [23]. Dysregulation of ncRNA expression has been directly linked to numerous disease states, including cancer, cardiovascular disorders, and inflammatory diseases, making them attractive therapeutic targets [22] [24].
Peptide Nucleic Acids (PNAs) represent a powerful class of DNA/RNA mimics for targeting ncRNAs with high affinity and specificity. First reported in 1991, PNAs feature a structurally modified backbone where the sugar-phosphate unit is replaced by repeating N-(2-aminoethyl)glycine units, while retaining standard nucleobases [1]. This unique structure confers exceptional binding affinity and sequence specificity toward complementary DNA or RNA sequences. The absence of charged phosphate groups in PNAs increases their stability against enzymatic and chemical degradation while enabling stronger PNA/RNA duplex formation through Hoogsteen-like base pairing [1]. These properties make PNAs ideal candidates for developing ncRNA-targeted therapeutics and diagnostics.
Molecular Mechanisms of ncRNA Regulation
Major ncRNA Classes and Functions
Table 1: Major Classes of Non-Coding RNAs and Their Biological Functions
| ncRNA Class | Length | Key Characteristics | Primary Functions |
|---|---|---|---|
| microRNA (miRNA) | 20-24 nt | Single-stranded, derived from hairpin precursors, seed sequence (bases 2-8) for target recognition | Post-transcriptional gene silencing via mRNA degradation or translational repression; regulates development, differentiation, apoptosis [20] [22] |
| Long Non-coding RNA (lncRNA) | >200 nt | RNA polymerase II transcribed, often polyadenylated, low evolutionary conservation | Chromatin remodeling, epigenetic regulation, transcriptional activation/repression, nuclear organization [23] [25] |
| Circular RNA (circRNA) | Variable | Covalently closed loop structure, no 5' cap or 3' polyA tail | miRNA sponging, protein binding, translation templates; elevated stability [26] |
| Piwi-interacting RNA (piRNA) | 24-31 nt | 2'-O-methyl modification at 3' end, strong 5' uridine preference | Transposon silencing in germline, genome defense, epigenetic regulation [20] |
| Small Interfering RNA (siRNA) | 20-24 nt | Perfectly complementary to targets, derived from long double-stranded RNA | Post-transcriptional gene silencing, transcriptional gene silencing via heterochromatin formation [20] |
ncRNA Mechanisms in Gene Regulation
Non-coding RNAs employ diverse mechanisms to regulate gene expression at multiple levels. MicroRNAs typically function post-transcriptionally by guiding the RNA-induced silencing complex (RISC) to target mRNAs through imperfect base pairing, primarily with the 3'-untranslated region (3'-UTR) [20] [22]. This interaction leads to either mRNA degradation or translational repression, with perfect complementarity resulting in Ago2-mediated cleavage of the mRNA [20].
Long non-coding RNAs exhibit more complex and varied mechanisms, which can be categorized into four primary archetypes [23]:
- Signals: LncRNAs serving as molecular indicators of specific biological events, such as Xist expression marking the inactivated X chromosome [23]
- Decoys: LncRNAs that molecular "sponges" titrating transcription factors or regulatory proteins away from their targets
- Guides: LncRNAs directing ribonucleoprotein complexes to specific genomic locations to regulate gene expression
- Scaffolds: LncRNAs serving as platforms for assembling multiple effector molecules into functional complexes
LncRNAs achieve these functions through their ability to form intricate secondary and tertiary structures that facilitate specific interactions with DNA, RNA, and proteins [25]. For instance, numerous lncRNAs interact with chromatin-modifying complexes such as PRC2 (polycomb repressive complex 2), which catalyzes the repressive H3K27me3 histone modification [23] [25]. Other lncRNAs regulate protein function by modulating enzymatic activity or preventing post-translational modifications, as exemplified by lnc-DC, which controls STAT3 phosphorylation in dendritic cells [25].
Diagram 1: Molecular Mechanisms of ncRNA-mediated Gene Regulation. Non-coding RNAs employ diverse strategies including guide functions, molecular scaffolding, decoy mechanisms, and epigenetic regulation to control gene expression at multiple levels.
PNA Design Strategies for ncRNA Targeting
PNA Backbone Modifications for Enhanced Performance
The utility of PNAs for ncRNA targeting can be significantly enhanced through strategic backbone modifications that address inherent challenges such as solubility, binding affinity, and cellular delivery [1]. Four primary modification strategies have emerged:
- Introduction of chirality: Incorporating chiral centers in the PNA backbone improves sequence specificity and binding affinity. For instance, PNA monomers synthesized from γ-lysine with 99.5% enantiomeric purity demonstrate enhanced DNA base pairing recognition [1]
- Conformational rigidity: Adding structural constraints through cyclopentyl, cyclohexyl, or pyrrolidinyl modifications pre-organizes the PNA structure for optimal target binding, reducing entropic penalties upon duplex formation [1]
- Cationic group incorporation: Attaching positively charged groups such as aminoethyl or guanidinium residues significantly enhances water solubility and facilitates cellular uptake through interaction with negatively charged cell membranes [1]
- Nucleobase and linker modifications: Strategic alterations to nucleobases or the linker connecting them to the backbone can fine-tune binding specificity and affinity. Examples include N4-benzoylcytosine, 6-thioguanine, and hypoxanthine modifications that enhance RNA binding properties [1]
Table 2: PNA Backbone Modification Strategies and Their Functional Impacts
| Modification Type | Specific Examples | Key Functional Improvements |
|---|---|---|
| Chirality Introduction | γ-lysine monomers, Cyclic β-amino acids | Enhanced enantiomeric purity (up to 99.5%), improved DNA/RNA recognition, increased sequence specificity [1] |
| Conformational Rigidity | Cyclopentyl, Cyclohexyl, Pyrrolidinyl oxy-modifications | Pre-organized backbone structure, reduced entropic cost of binding, enhanced thermal stability of duplexes [1] |
| Cationic Modifications | Aminoethyl groups, Guanidinium linkages | Improved water solubility, enhanced cellular uptake, reduced aggregation tendency [1] |
| Nucleobase/Linker Alterations | N4-benzoylcytosine, 6-thioguanine, Hypoxanthine | Increased binding affinity, enhanced specificity, improved mismatch discrimination [1] |
| Terminal Modifications | Acridone, 5-aminouracil, Thio-pseudoisocytosine | Fluorophore incorporation, functional group presentation, diagnostic probe development [1] |
PNA-ncRNA Binding Mechanisms
PNAs bind to complementary ncRNA sequences through Watson-Crick base pairing, forming highly stable PNA-RNA duplexes with superior thermal stability compared to natural nucleic acid duplexes [1]. For example, 15-mer PNA/RNA duplexes exhibit melting temperatures of approximately 70°C, significantly higher than the 55°C observed for equivalent RNA/RNA duplexes [1]. This enhanced stability arises from the neutral polyamide backbone of PNAs, which eliminates electrostatic repulsion with the negatively charged RNA backbone.
The binding specificity of PNAs can be harnessed to target functional domains of ncRNAs:
- For miRNAs, PNAs can be designed to target the seed sequence (positions 2-8), preventing interaction with target mRNAs
- For structured lncRNAs, PNAs can be directed against key functional domains involved in protein binding or structural motifs
- For circRNAs, PNAs can block miRNA binding sites, preventing their sponge function
The high binding affinity of PNAs enables effective targeting of structured RNA regions that might be challenging for conventional antisense oligonucleotides, making them particularly valuable for tackling complex ncRNA structures.
Experimental Protocols
Protocol 1: Solid-Phase PNA Synthesis and Purification
Principle: PNAs are synthesized using solid-phase peptide synthesis methodology, employing Finoc (fluorenylmethyloxycarbonyl) or Boc (tert-butyloxycarbonyl) chemistry for sequential monomer addition [1].
Materials:
- Merrifield resin or other solid support
- PNA monomers with appropriate protecting groups (PG1 for N-terminus, PG2 for nucleobases)
- Coupling reagents: HBTU/HOBt or PyBOP
- Deprotection reagents: Trifluoroacetic acid (TFA), Piperidine
- Cleavage reagents: 4-Trifluoromethyl salicylic acid (TFMSA) or TFA
- Purification system: Reverse-phase HPLC
- Characterization: MALDI-TOF or ESI mass spectrometry
Procedure:
- Resin Preparation: Pre-swell the solid support (100 mg) in dichloromethane (DCM) for 30 minutes, then wash with dimethylformamide (DMF, 3 × 5 mL)
- First Monomer Attachment: Couple the C-terminal PNA monomer (0.2 mmol) to the resin using coupling reagents (0.19 M HBTU/HOBt) in the presence of diisopropylethylamine (DIPEA, 0.4 M) for 30-60 minutes
- Deprotection: Remove the N-terminal protecting group (PG1) using 20% Piperidine in DMF or TFA treatment (2 × 10 minutes)
- Chain Elongation: Sequentially couple additional PNA monomers using steps 2-3 until the full sequence is assembled
- Final Cleavage: Cleave the PNA oligomer from the resin using TFMSA or TFA cocktail containing appropriate scavengers (3 hours)
- Deprotection: Remove nucleobase protecting groups (PG2) simultaneously during cleavage or in a separate step
- Purification: Purify the crude PNA by reverse-phase HPLC using a C18 column and acetonitrile/water gradient
- Characterization: Verify identity by high-resolution mass spectrometry (HRMS) with MALDI or TOF detection
Quality Control:
- Purity assessment by analytical HPLC (>95% purity recommended)
- Mass confirmation by MS spectrometry
- Concentration determination by UV absorbance
Protocol 2: PNA Design and Testing for miRNA Inhibition
Principle: This protocol describes the design and evaluation of anti-miRNA PNAs to specifically inhibit miRNA function, potentially using miR-142-3p in hepatocellular carcinoma as a model system [26].
Materials:
- Target miRNA sequence (e.g., from miRBase database)
- PNA design software or manual sequence design
- Cell culture system relevant to disease model
- Transfection reagent compatible with PNAs
- RNA isolation kit
- qRT-PCR reagents for miRNA and target mRNA quantification
- Western blot equipment for protein analysis
- Luciferase reporter system for validation
Procedure:
- PNA Design:
- Identify the mature miRNA sequence (e.g., miR-142-3p) from miRBase
- Design complementary PNA sequence (15-18 mer) targeting the miRNA seed region
- Incorporate backbone modifications as needed (e.g., lysine residues for solubility)
- Include a fluorophore tag (e.g., FITC) for cellular uptake tracking if needed
Cell Culture and Transfection:
- Culture appropriate cell line (e.g., HepG2 for hepatocellular carcinoma) in recommended media
- Seed cells in 24-well plates at 50,000 cells/well and incubate for 24 hours
- Transfect with anti-miRNA PNA (50-100 nM) using suitable transfection reagent
- Include controls: scrambled PNA sequence, transfection reagent only
Efficacy Assessment:
- Extract total RNA 48 hours post-transfection using RNA isolation kit
- Perform qRT-PCR to measure:
- Target miRNA levels (significant reduction expected)
- Known target mRNA levels (e.g., YES1 and TWF1 for miR-142-3p) [26]
- Analyze protein expression of target genes by Western blot 72 hours post-transfection
Functional Validation:
- Perform luciferase reporter assay with 3'UTR of target genes
- Assess phenotypic effects: proliferation, apoptosis, migration as relevant
- For miR-142-3p, evaluate restoration of drug sensitivity (e.g., to lenvatinib) [26]
Expected Results: Effective anti-miRNA PNAs should reduce functional miRNA levels by >70%, increase target mRNA and protein expression, and produce measurable phenotypic changes consistent with miRNA inhibition.
Diagram 2: PNA Development Workflow for ncRNA Targeting. Comprehensive process from initial sequence design through synthesis, validation, and functional assessment in cellular models.
Protocol 3: lncRNA Targeting for Cancer Therapy Sensitization
Principle: This protocol describes targeting specific lncRNAs to sensitize cancer cells to therapeutics, using homologous recombination deficiency (HRD) in high-grade serous ovarian cancer (HGSC) as a model [27].
Materials:
- TCGA or other database with lncRNA expression and clinical data
- PNA sequences targeting identified lncRNAs (e.g., ENSG00000272172.1)
- Ovarian cancer cell lines (e.g., OVCAR, SKOV3)
- PARP inhibitor (e.g., Olaparib)
- Clonogenic survival assay reagents
- γH2AX immunofluorescence staining for DNA damage
- RNA-FISH probes for lncRNA localization
Procedure:
- Target Identification:
- Analyze TCGA ovarian cancer dataset for lncRNAs correlating with HRD scores
- Identify top candidates (e.g., ENSG00000272172.1, upregulated in HRD-positive tumors) [27]
- Design PNAs (15-20 mer) complementary to functional domains of target lncRNA
Therapeutic Sensitization Assessment:
- Culture HGSC cell lines with varying HRD status
- Transfect with lncRNA-targeting PNAs (100 nM) for 24 hours
- Treat with PARP inhibitor (e.g., 10 μM Olaparib) for 48-72 hours
- Assess combination effects:
- Clonogenic survival assay
- Apoptosis measurement (Annexin V/PI staining)
- DNA damage response (γH2AX foci formation)
Mechanistic Studies:
- Perform RNA-FISH to confirm lncRNA localization and PNA-mediated disruption
- Evaluate replication dynamics (DNA fiber assay)
- Assess HR efficiency (DR-GFP reporter assay)
- Examine key protein levels (BRCA1, RAD51) by Western blot
Expected Results: Effective lncRNA-targeting PNAs should enhance PARP inhibitor sensitivity, particularly in HRD-positive models, increase DNA damage markers, and disrupt replication dynamics consistent with HR pathway modulation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PNA-based ncRNA Targeting Studies
| Reagent Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| PNA Synthesis Reagents | Fmoc-PNA monomers, Merrifield resin, HBTU/HOBt coupling reagents | Solid-phase PNA oligomer synthesis | High coupling efficiency, orthogonal protecting groups, compatibility with standard peptide synthesizers [1] |
| PNA Delivery Systems | Cell-penetrating peptides (e.g., Tat, Penetratin), Lipid nanoparticles, Polymeric nanocarriers | Enhanced cellular PNA delivery | Improved bioavailability, endosomal escape capability, reduced toxicity [1] [21] |
| ncRNA Detection Tools | LNA-modified probes for FISH, qRT-PCR assays, RNA-seq libraries | Detection and quantification of target ncRNAs | High specificity and sensitivity, single-cell resolution, multiplexing capability [27] [28] |
| Functional Assessment Kits | Luciferase reporter vectors, miRNA mimic/inhibitor sets, Apoptosis/viability assays | Validation of ncRNA targeting efficacy | Quantitative readouts, high-throughput compatibility, established protocols [26] [22] |
| Bioinformatics Resources | miRBase, lncRNAdb, TCGA datasets, PNA design software | Target identification and PNA sequence design | Curated databases, predictive algorithms, clinical correlation data [27] [28] |
Applications in Therapeutics and Diagnostics
Therapeutic Applications of PNA-based ncRNA Targeting
PNA-mediated ncRNA targeting has demonstrated significant potential across multiple therapeutic areas:
Cancer Therapy:
- miRNA targeting: PNA-based inhibition of oncogenic miRNAs (e.g., miR-155, miR-21) restores tumor suppressor expression and reduces proliferation [1] [22]
- lncRNA modulation: Targeting deregulated lncRNAs (e.g., HOTAIR, MALAT1) affects cancer cell invasion, metastasis, and drug resistance [27] [22]
- Treatment sensitization: PNA-mediated lncRNA targeting can restore chemosensitivity, as demonstrated in hepatocellular carcinoma where miR-142-3p restoration overcame tyrosine-kinase-inhibitor resistance [26]
Antimicrobial Applications:
- Antisense PNAs: Specifically inhibit resistance genes in pathogens including P. aeruginosa, A. baumannii, and methicillin-resistant S. aureus, restoring antibiotic efficacy [1]
- Species-specific targeting: PNAs can be designed to target essential bacterial genes with high specificity, reducing collateral damage to microbiome [1]
Antiviral Therapeutics:
- HIV-1 replication inhibition: 15-base PNA oligomers targeting essential viral sequences effectively suppress HIV-1 replication [1]
- Hepatitis B inhibition: Tat-conjugated PNAs (Tat-PNA-DR) inhibited HBV replication in HepG2 cells in both in vitro and in vivo models [1]
Diagnostic Applications
The high specificity and stability of PNAs make them valuable tools for diagnostic applications:
Biomarker Detection:
- Fluorescent in situ hybridization (FISH): PNA-based probes enable specific detection of bacterial pathogens (e.g., S. aureus) and viral infections with enhanced signal-to-noise ratio [1]
- Mutation detection: PNA probes can distinguish single-nucleotide polymorphisms, enabling identification of cancer mutations (e.g., BCR-ABL T315I mutation) at single-cell level [1]
- Circulating biomarker detection: PNAs facilitate detection of circulating ncRNAs in plasma/serum, offering non-invasive diagnostic options [27]
Imaging Applications:
- Radiolabeled PNAs: ⁶⁴Cu-radiolabeled anti-miRNA PNAs enable radioimaging of inflammatory conditions like giant cell arteritis [1]
- Tumor imaging: ⁹⁹Tc-labeled antisense PNAs targeting survivin and c-myc mRNAs serve as effective tumor imaging agents [1]
Targeting non-coding RNAs with peptide nucleic acids represents a powerful strategy for regulating gene expression with significant implications for both therapeutic development and diagnostic applications. The unique properties of PNAs—including high binding affinity, biological stability, and specificity—make them particularly suitable for tackling the complex challenges of ncRNA targeting. As research continues to unravel the intricate networks of ncRNA regulation in health and disease, PNA-based approaches offer a versatile platform for translating these insights into clinical applications. The ongoing development of enhanced PNA designs, combined with improved delivery strategies, promises to further expand the utility of this approach across a broadening spectrum of human diseases.
From Bench to Bedside: PNA Applications in Therapy and Diagnostic Platforms
Antisense therapeutics represent a transformative approach in precision medicine, utilizing synthetic nucleic acids to modulate gene expression at the RNA level. These therapies function through sequence-specific binding to target RNA transcripts, enabling highly selective intervention in disease processes [29]. Within this domain, peptide nucleic acids (PNAs) have emerged as particularly promising agents due to their unique biochemical properties and potent mechanisms of action.
PNAs are synthetic nucleic acid analogs where the natural phosphodiester backbone is replaced by an uncharged N-(2-aminoethyl) glycine backbone [30] [1]. This fundamental structural modification confers significant advantages over natural oligonucleotides, including increased resistance to enzymatic degradation, exceptional thermal stability, and strong binding affinity to complementary DNA and RNA sequences [30] [1]. The neutral backbone eliminates electrostatic repulsion with target nucleic acids, allowing for more stable duplex formation compared to their natural counterparts [1].
The therapeutic potential of antisense PNAs spans two primary mechanisms: correcting aberrant splicing patterns in genetic disorders and silencing oncogenic transcripts in cancer. These applications leverage the fundamental principle of Watson-Crick base pairing to achieve precise targeting of disease-related RNAs, offering promising avenues for treating conditions that have historically proven challenging to address with conventional small-molecule therapeutics [30].
PNA Design and Synthesis Protocols
Backbone Modifications and Conjugation Strategies
The synthesis of therapeutic PNAs employs solid-phase peptide synthesis (SPPS) methodologies, allowing for the incorporation of various backbone modifications that enhance their drug-like properties [1]. The following protocols detail the essential procedures for PNA synthesis and quality control.
Protocol 1: Solid-Phase PNA Synthesis Using Fmoc Chemistry
- Resin Preparation: Load 100 mg of Rink amide resin (0.1 mmol/g loading capacity) into a solid-phase reaction vessel. Swell the resin in 5 mL of dimethylformamide (DMF) for 30 minutes with gentle agitation [1].
- Fmoc Deprotection: Drain the DMF and treat the resin with 5 mL of 20% piperidine in DMF for 10 minutes with continuous mixing. Drain and repeat this deprotection step for an additional 5 minutes [1].
- Monomer Coupling: Prepare a coupling solution containing 4 equivalents of Fmoc-PNA monomer, 4 equivalents of HBTU, and 8 equivalents of DIPEA in 3 mL of DMF. Add this solution to the resin and mix for 45-60 minutes at room temperature [1].
- Wash Cycle: After coupling completion, drain the coupling solution and wash the resin sequentially with DMF (3 × 5 mL), dichloromethane (2 × 5 mL), and again with DMF (2 × 5 mL) [1].
- Repetition: Repeat steps 2-4 for each additional monomer until the complete PNA sequence is assembled.
- Cleavage and Global Depprotection: Treat the resin with 5 mL of cleavage cocktail (95% trifluoroacetic acid, 2.5% water, 2.5% triisopropylsilane) for 2-3 hours at room temperature with gentle agitation. Filter the solution into cold diethyl ether to precipitate the crude PNA [1].
- Purification and Characterization: Purify the crude product by reverse-phase high-performance liquid chromatography (RP-HPLC) and characterize using high-resolution mass spectrometry (HRMS) with MALDI or TOF detectors [1].
Protocol 2: Quality Control and Validation of PNA Oligomers
- Purity Assessment: Analyze the purified PNA by analytical RP-HPLC using a C18 column with a water-acetonitrile gradient containing 0.1% TFA. Accept only batches with >95% purity by peak area integration [1].
- Sequence Verification: Confirm identity via electrospray ionization mass spectrometry (ESI-MS) or MALDI-TOF MS. Compare observed molecular weight with theoretical values [1].
- Binding Affinity Validation: Determine melting temperature (Tm) of PNA-RNA duplexes using UV spectrophotometry. A typical 15-mer PNA/RNA duplex should exhibit a Tm of approximately 70°C, significantly higher than the corresponding DNA/RNA duplex (~55°C) [1].
- Functional Validation: For splicing-modifying PNAs, validate efficacy using minigene splicing assays in appropriate cell lines. For oncogene-targeting PNAs, demonstrate dose-dependent reduction of target mRNA or protein in relevant cancer models [30].
Table 1: Research Reagent Solutions for PNA Synthesis and Application
| Research Reagent | Function/Application | Key Characteristics |
|---|---|---|
| Fmoc-PNA Monomers | Building blocks for PNA synthesis | Fmoc-protected; various nucleobases; Fmoc-protected monomers are more cost-effective than Boc alternatives [30] |
| Rink Amide Resin | Solid support for synthesis | Loading capacity 0.1-0.8 mmol/g; compatible with Fmoc chemistry [1] |
| HBTU | Coupling reagent | Activates carboxyl groups for amide bond formation [1] |
| TFMSA/TFA Cocktail | Cleavage and deprotection | Removes PNA from resin and cleaves side-chain protecting groups [1] |
| Cell-Penetrating Peptides | Delivery enhancement | Conjugated to PNAs to improve cellular uptake (e.g., Tat, Penetratin) [30] |
| PLGA Nanoparticles | Delivery vehicle | Biocompatible, biodegradable polymer for PNA encapsulation and delivery [31] |
Correcting Splicing Defects with PNA Therapeutics
Mechanisms of Splicing Modulation
Splice-switching PNAs function through steric blockade of pre-mRNA regulatory elements, redirecting the splicing machinery to alter exon inclusion or exclusion patterns [30]. These oligonucleotides target specific sequences including exon splicing enhancers (ESEs), exon splicing silencers (ESSs), and intronic splicing motifs to modulate splicing outcomes [32].
The therapeutic application of splicing correction encompasses several distinct approaches:
- Exon Inclusion: Blocking ESSs or intronic splicing silencers to promote inclusion of critical exons
- Exon Skipping: Masking ESEs to exclude problematic exons and restore reading frames
- Cryptic Exon Exclusion: Preventing inclusion of pseudo-exons generated by deep intronic mutations [29]
Protocol 3: In Vitro Splicing Correction Assay Using PNA
- Cell Line Selection: Culture HEK293T or disease-relevant cell lines in appropriate medium (DMEM + 10% FBS) at 37°C with 5% CO₂.
- PNA Transfection: At 60-70% confluence, transfect cells with 100-500 nM of splicing-corrective PNA using lipofectamine 3000 according to manufacturer's protocol. Include scrambled PNA sequence as negative control.
- RNA Isolation: 48 hours post-transfection, extract total RNA using TRIzol reagent. Quantify RNA concentration by spectrophotometry.
- RT-PCR Analysis: Perform reverse transcription with 1 μg total RNA using oligo(dT) or random hexamer primers. Conduct PCR with primers flanking the target splicing region (25-35 cycles).
- Gel Electrophoresis: Separate PCR products on 2-3% agarose gels. Visualize bands with ethidium bromide or SYBR Safe staining.
- Quantification: Analyze band intensities using densitometry software. Calculate percentage of corrected splicing as (corrected isoform/total isoforms) × 100%.
Table 2: Quantitative Comparison of Splicing Correction Approaches
| Application | Disease Target | PNA Design Strategy | Reported Efficacy | Key Challenges |
|---|---|---|---|---|
| Exon Skipping | Duchenne Muscular Dystrophy (DMD) | Target exon splicing enhancers in dystrophin pre-mRNA | Up to 60% dystrophin restoration in preclinical models [32] | Delivery to muscle tissue; durability of effect |
| Exon Inclusion | Spinal Muscular Atrophy (SMA) | Block intronic splicing silencer in SMN2 gene | Increased full-length SMN protein by >50% [29] | Blood-brain barrier penetration |
| Cryptic Exon Exclusion | Batten Disease (CLN7) | Target pseudo-exon recognition sequence in MFSD8 gene | Functional protein restoration in patient-derived neurons [29] | Ultra-rare mutation specificity |
| Oncogenic Splicing Switch | Osteosarcoma | Modulate INSR splicing from IR-A to IR-B isoform | Suppressed tumor progression in xenograft models [32] | Tumor-specific delivery; off-target effects |
Case Study: Correcting NF1 Splicing Defects in Glioma
In high-grade gliomas, the neurofibromin 1 (NF1) gene frequently undergoes aberrant splicing, leading to inclusion of exon 23a and production of a less active tumor suppressor isoform [33]. This splicing alteration occurs in >80% of HGG cases and activates the RAS/MAPK pathway independent of mutational events.
Protocol 4: PNA-Mediated NF1 Splicing Correction in Glioma Models
- PNA Design: Design 15-18 mer anti-sense PNA complementary to the intronic splicing silencer responsible for exon 23a inclusion in NF1 pre-mRNA.
- Cell Culture: Maintain U87MG or patient-derived glioma stem cells in neurobasal medium with appropriate growth factors.
- PNA Delivery: Complex PNA with cell-penetrating peptides (e.g., Tat, Penetratin) at 1:5 molar ratio. Add complexes to cells at final PNA concentration of 500 nM-1 μM.
- Efficacy Assessment: 72 hours post-treatment, analyze NF1 splicing pattern by RT-PCR. Monitor RAS/MAPK pathway activity by western blotting for phosphorylated ERK.
- Functional Assays: Evaluate changes in proliferation (MTS assay), invasion (Transwell assay), and apoptosis (Annexin V staining) in PNA-treated versus control cells.
PNA-Mediated NF1 Splicing Correction in Glioma
Silencing Oncogenes with PNA Therapeutics
Mechanisms of Oncogene Silencing
PNA-mediated oncogene silencing primarily utilizes two distinct mechanisms: the RNase H-dependent gapmer approach for transcript degradation and translational inhibition through steric blockade of ribosomal machinery [29] [30]. Gapmer PNAs contain a central DNA gap flanked by modified RNA-like nucleotides that activate RNase H-mediated cleavage of the target RNA, while translational inhibitory PNAs bind directly to the AUG start codon or coding regions to prevent ribosome assembly or progression [29] [30].
The selection of targeting strategy depends on multiple factors including the nature of the oncogenic mutation (gain-of-function versus dominant-negative), cellular localization of the target RNA, and the desired duration of effect. For allele-specific silencing in disorders caused by dominant-negative mutations, PNAs can be designed to exploit single-nucleotide polymorphisms (SNPs) to selectively target mutant alleles while sparing wild-type transcripts [29].
Protocol 5: PNA-Mediated Oncogene Silencing in Cancer Cells
- PNA Design for Allele-Specific Targeting: For oncogenes with point mutations (e.g., KRAS G12D), design PNAs perfectly complementary to the mutant sequence with a single mismatch against the wild-type allele to confer selectivity [29].
- Cell Culture and Transfection: Culture relevant cancer cell lines (e.g., pancreatic cancer cells for KRAS targeting) in appropriate medium. Transfect with 100-200 nM of oncogene-targeting PNA using lipid-based transfection reagents.
- Efficacy Validation: 48-72 hours post-transfection, assess:
- mRNA reduction via quantitative RT-PCR
- Protein downregulation via western blotting
- Phenotypic effects (proliferation, apoptosis, cell cycle)
- Specificity Assessment: Evaluate off-target effects by transcriptome analysis or monitoring non-targeted housekeeping genes.
Case Study: Targeting CDK11 in Cancer
Recent target deconvolution studies have revealed that several mischaracterized anti-cancer agents actually function through inhibition of cyclin-dependent kinase CDK11 [34]. Multiple cancer types demonstrate addiction to CDK11 expression, making it a promising target for PNA-based silencing approaches.
Protocol 6: PNA Design for CDK11 Silencing
- Target Site Selection: Identify accessible regions in CDK11 mRNA using RNA accessibility prediction algorithms. Prioritize target sites near the translation start codon or within 5'-UTR regulatory elements.
- Gapmer PNA Design: Construct gapmer PNA with:
- 5' and 3' wings containing 2-3 modified nucleotides (e.g., LNA)
- Central DNA gap of 7-10 nucleotides for RNase H recruitment
- Total length of 15-18 nucleotides
- Control Design: Include scrambled sequence control and mismatch control (2-3 nucleotide mismatches) to demonstrate sequence specificity.
- Delivery Optimization: Formulate PNA with PLGA/PVA nanoparticles using double emulsion solvent evaporation technique to enhance cellular uptake [31].
PNA-Mediated Oncogene Silencing Mechanism
Table 3: Quantitative Analysis of Oncogene Silencing Efficacy
| Oncogene Target | Cancer Type | PNA Strategy | Silencing Efficiency | Functional Outcome |
|---|---|---|---|---|
| CDK11 | Multiple Cancers | Gapmer PNA with RNase H activation | >70% mRNA reduction [34] | Impaired cancer cell proliferation; apoptosis induction |
| mutant SOD1 | Amyotrophic Lateral Sclerosis | Allele-specific gapmer (Tofersen) | ~50% protein reduction [29] | Delayed disease progression (approved therapy) |
| mutant KRAS | Pancreatic Cancer | Mutation-specific gapmer | 60-80% mutant allele knockdown [29] | Reduced tumor growth in PDX models |
| Bcl-2 | Lymphocytic Lymphoma | Antisense PNA-peptide conjugate | >60% protein reduction [1] | Enhanced chemosensitivity in Mec-1 cells |
| C-Myc | Various Cancers | Antisense PNA with 99Tc labeling | Significant mRNA inhibition [1] | Tumor imaging and growth suppression |
Advanced Delivery Strategies for PNA Therapeutics
Nanoparticle-Based Delivery Systems
Effective delivery remains a critical challenge in PNA therapeutics. PLGA/PVA nanoparticles have demonstrated promising results for PNA/donor DNA delivery systems, showing efficient cellular uptake and sustained release profiles [31]. The double emulsion solvent evaporation technique enables efficient encapsulation of PNA oligomers while maintaining their biological activity.
Protocol 7: PLGA Nanoparticle Formulation for PNA Delivery
- Primary Emulsion: Dissolve 50 mg PLGA in 2 mL dichloromethane. Add 200 μL of aqueous PNA solution (1 mg/mL in nuclease-free water). Sonicate using probe sonicator at 40 W for 60 seconds on ice.
- Secondary Emulsion: Add the primary emulsion to 4 mL of 2% PVA solution. Homogenize at 8000 rpm for 2 minutes to form water-in-oil-in-water (W/O/W) double emulsion.
- Solvent Evaporation: Stir the double emulsion overnight at room temperature to evaporate organic solvent.
- Nanoparticle Collection: Centrifuge at 15,000 × g for 20 minutes. Wash pellets three times with distilled water to remove excess PVA.
- Characterization: Determine particle size and zeta potential using dynamic light scattering. Confirm PNA loading efficiency via HPLC analysis of supernatant.
- In Vitro Testing: Evaluate cellular uptake using fluorescence-labeled PNAs. Assess cytotoxicity and target engagement in relevant cell models.
Conjugation Approaches for Enhanced Delivery
Chemical conjugation represents another powerful strategy to improve the pharmacokinetic properties and cellular uptake of therapeutic PNAs. Common conjugation approaches include:
- Cell-penetrating peptides (CPPs): Tat, Penetratin, or Transportan conjugates to enhance membrane permeability [30]
- GalNAc conjugation: For hepatocyte-specific delivery through asialoglycoprotein receptor-mediated endocytosis [32]
- Ligand-receptor targeting: Antibody fragments or peptide ligands for tissue-specific delivery
- Nuclear localization signals (NLS): For enhanced nuclear delivery in antigene applications [1]
Recent advances have demonstrated that PNA-YR9 conjugates (a radiolabeled antisense oligonucleotide hybrid) enable both therapeutic delivery and diagnostic imaging capabilities, representing a promising theranostic approach in oncology [1].
Peptide Nucleic Acid (PNA) is a synthetic nucleic acid analog first invented in 1991 by Nielsen, Egholm, Berg, and Buchardt [12]. Its molecular structure fundamentally differs from the natural DNA or RNA it aims to mimic. Where DNA and RNA possess a sugar-phosphate backbone, PNA features a structurally homogeneous backbone composed of repeating N-(2-aminoethyl)-glycine units linked by peptide bonds [35] [12] [36]. The various purine and pyrimidine bases are linked to this backbone by a methylene bridge and a carbonyl group [12]. This unique architecture confers several advantageous physicochemical properties crucial for gene editing applications.
The neutral polyamide backbone of PNA eliminates the negative charge present in native nucleic acids. This absence of electrostatic repulsion leads to significantly higher binding affinity and specificity for complementary DNA or RNA sequences compared to their natural counterparts [35] [12]. Furthermore, because PNA is neither a true nucleic acid nor a natural peptide, it exhibits increased resistance to enzymatic degradation by both nucleases and proteases, enhancing its stability in biological environments [35] [12]. It remains stable across a wide range of temperatures and pH levels, making it a robust tool for research and therapeutic development [35].
PNA as a Superior Gene Editing Tool: Comparative Advantages
The following table summarizes the key advantages of PNA as a non-enzymatic gene editing tool compared to the CRISPR-Cas9 system.
Table 1: Comparative Analysis of PNA and CRISPR-Cas9 Gene Editing Platforms
| Feature | PNA-Based Editing | CRISPR-Cas9 System |
|---|---|---|
| Core Mechanism | Non-enzymatic; strand invasion and donor DNA templating [36] [37] | Enzymatic; RNA-guided DNA cleavage by Cas nuclease [38] |
| DNA Breaks | Does not generate double-strand breaks (DSBs) [37] | Relies on creating double-strand breaks (DSBs) [39] [38] |
| Off-Target Effects | Low off-target genome effects reported [37] | Risk of off-target edits and complex on-target rearrangements [39] [40] |
| Molecular Backbone | Neutral, polyamide (N-(2-aminoethyl)-glycine) [35] [12] | Negatively charged, RNA-based guide [38] |
| Stability | High resistance to nucleases and proteases [35] [12] | RNA components are susceptible to degradation |
| Key Limitation | Requires optimized delivery strategies (e.g., nanoparticles) [12] [37] | Delivery challenges and potential immune responses to bacterial Cas protein [41] |
PNA Mechanism of Action in Gene Editing
PNA facilitates gene editing through a unique, enzyme-free mechanism that contrasts sharply with nuclease-based systems like CRISPR-Cas9.
The P-Loop Formation and Strand Invasion
PNA oligomers possess the unique ability to invade double-stranded DNA helices [36] [37]. They do this by selectively aligning with one strand of the DNA duplex and displacing the other, forming a specialized structure known as a p-loop [37]. This process is driven by the high affinity and stability of PNA-DNA binding, which is stronger than natural DNA-DNA binding due to the lack of electrostatic repulsion [12]. The formation of this structure locally opens the DNA duplex, making it accessible for subsequent repair processes.
Endogenous Repair and Recombination
The P-loop structure has been shown to activate endogenous DNA repair mechanisms within the cell [37]. When a single-stranded DNA (ssDNA) template encoding a desired sequence change is co-delivered with the PNA, these activated repair pathways can use the ssDNA as a template [37]. This stimulates homology-directed repair (HDR) between the target genomic locus and the donor DNA, leading to a precise and stable genetic edit [36] [37]. PNA has been demonstrated to enhance recombination efficiency by more than five-fold compared to donor DNA alone [37].
The diagram below illustrates this non-enzymatic gene editing mechanism.
Application Notes: PNA-Mediated Gene Editing Protocol
This protocol details the methodology for PNA-mediated gene editing, based on a recent study that successfully introduced a mutation into the HBB gene in human fibroblasts [37].
The complete experimental workflow, from design to validation, is summarized in the diagram below.
Detailed Stepwise Protocol
Step 1: Design and Synthesis of PNA and Donor DNA
- PNA Design: Design a gamma-modified PNA (γPNA) oligomer. The example study used a 26-base γPNA (13 bases for each strand) with the WC strand substituted at the gamma position with miniPEG every 3 bases to improve solubility and binding efficiency [37]. The sequence should be complementary to the target genomic site.
- Donor DNA Design: Design a single-stranded donor DNA oligonucleotide (e.g., 50 nucleotides in length) that is homologous to the target gene but contains the desired mutation. The sequence should be protected at the 5′- and 3′-ends by three phosphorothioate internucleoside linkages at each end to confer nuclease resistance [37].
- Validation: Confirm PNA binding efficiency via a PNA Gel Mobility Shift Assay, where a PCR product of the target gene is incubated with the PNA and analyzed by gel electrophoresis to observe a mobility shift [37].
Step 2: Nanoparticle (NP) Formulation and Characterization
- Encapsulation: Encapsulate the PNA and donor DNA oligomers using a modified double-emulsion solvent evaporation technique. The example used Poly(lactic-co-glycolic acid) (PLGA) as the polymer matrix [37].
- Prepare two batches: combined PNA/DNA-loaded PLGA NPs and blank PLGA NPs as a control.
- NP Characterization: Validate the formulated NPs by performing:
- Release Test: Incubate loaded NPs in PBS at 37°C to profile the release of the oligonucleotides over time [37].
- Loading Test & Encapsulation Efficiency: Quantify the amount of PNA/DNA successfully encapsulated within the NPs.
Step 3: Cell Culture and Treatment with NPs
- Cell Culture: Culture target cells (e.g., human skin fibroblasts) in standard media (e.g., DMEM supplemented with 10% FBS and antibiotics) at 37°C in a 5% CO₂ atmosphere [37].
- NP Treatment: Upon reaching 90% confluence, treat cells with the formulated PNA/DNA-loaded NPs. The study confirmed that the presence of PLGA NPs in the media did not hinder cell adhesion or proliferation [37].
- Controls: Include untreated cells and cells treated with blank NPs.
Step 4: Molecular Analysis of Gene Editing
- DNA Extraction: Harvest treated cells and extract genomic DNA.
- Sequence Analysis: Perform PCR amplification of the target genomic region (e.g., the HBB gene) and subject the product to direct Sanger sequencing using kits like the BigDye Terminator v3.1 Cycle Sequencing Kit [37]. This confirms the introduction of the desired mutation.
- Editing Frequency: Quantify the frequency of gene editing. The referenced study reported a persistent editing frequency of about 3.7% after a single dose of NPs, which was not significantly increased by multiple dosing [37].
Step 5: Functional Validation of the Edit
- RNA Extraction and Analysis: Extract total RNA from the treated cells and perform quantitative RT-PCR to assess changes in the expression levels of the target gene. A successful edit should lead to a corresponding functional change; for instance, the HBB gene edit resulted in a decrease in its expression [37].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and materials required for establishing PNA-mediated gene editing based on the protocol above.
Table 2: Essential Research Reagents for PNA Gene Editing
| Reagent/Material | Function/Description | Example/Specification |
|---|---|---|
| Gamma-Modified PNA (γPNA) | Synthetic molecule that invades dsDNA to initiate editing; gamma modification enhances binding and solubility [36] [37]. | 26-base γPNA with miniPEG substitution every 3 bases; Boc chemistry synthesis [37]. |
| Donor DNA Oligonucleotide | Single-stranded DNA template carrying the desired mutation for homology-directed repair [37]. | 50 nt ssDNA with 3x phosphorothioate linkages at each end for nuclease resistance [37]. |
| PLGA Polymer | Biocompatible, biodegradable polymer used to formulate nanoparticles for intracellular delivery of PNA/DNA [37]. | Used with Polyvinyl Alcohol (PVA); forms NPs via double-emulsion solvent evaporation [37]. |
| Cell Culture System | In vitro model for testing gene editing efficiency. | Human skin fibroblasts; cultured in DMEM + 10% FBS [37]. |
| PNA Gel Mobility Shift Assay | Validates the binding efficiency of the designed PNA to its complementary target sequence [37]. | Agarose gel electrophoresis (1%) of PCR product incubated with PNA [37]. |
| Sequencing Kit | Confirms the incorporation of the genetic edit at the DNA level. | BigDye Terminator v3.1 Cycle Sequencing Kit, analyzed on a genetic analyzer [37]. |
Quantitative Outcomes and Therapeutic Potential
PNA-mediated gene editing has demonstrated promising, though modest, efficiency in preclinical models. The key quantitative outcomes from recent research are summarized below.
Table 3: Quantitative Outcomes of PNA Gene Editing from Preclinical Studies
| Parameter | Reported Outcome | Context and Model |
|---|---|---|
| Editing Frequency | ~3.7% [37] | Single dose in human fibroblasts; mutation introduced into the HBB gene. |
| Persistence of Edit | Persistent after removal of NPs from media [37] | Indicates a stable, permanent genomic modification. |
| Functional Effect | Corresponding decrease in HBB gene expression [37] | Confirms that the genetic edit leads to a functional outcome. |
| Therapeutic Effect | Clinically relevant protein restoration and disease improvement [37] | Preclinical mouse models of beta-thalassemia showed reversal of symptoms. |
| Safety Profile | Low off-target genome effects; no measurable increase in inflammatory cytokines with IV NP delivery [37] | Suggests a favorable safety and toxicity profile. |
The therapeutic potential of PNA is particularly evident in monogenic disorders. In beta-thalassemia, PNA-mediated editing in preclinical models has successfully reversed splenomegaly, reduced reticulocytosis, and restored hemoglobin levels to wild-type ranges [37]. Furthermore, PNA-based strategies are being explored for cystic fibrosis, sickle cell disease, Huntington's disease, and Duchenne muscular dystrophy, highlighting its versatility as a promising therapeutic platform [37].
Peptide Nucleic Acid (PNA) represents a powerful class of synthetic oligonucleotide mimetics that has revolutionized molecular diagnostic technologies. With a neutral N-(2-aminoethyl)-glycine backbone replacing the negatively charged sugar-phosphate backbone of natural nucleic acids, PNA exhibits superior hybridization properties, including enhanced binding affinity and excellent specificity for complementary DNA and RNA sequences [42] [43]. This unique molecular structure confers significant advantages over natural nucleic acids, including metabolic stability and resistance to nucleases and proteases, making PNA ideal for demanding diagnostic applications [43]. These properties have been successfully harnessed in three transformative diagnostic approaches: Fluorescence In Situ Hybridization (PNA-FISH), PCR clamping, and biosensor probes, each offering unique capabilities for research and clinical diagnostics.
The following diagram illustrates the core structure of PNA and its diagnostic mechanisms:
PNA-FISH (Fluorescence In Situ Hybridization)
PNA-FISH leverages the unique properties of peptide nucleic acids for chromosomal visualization and microbial identification. The electrically neutral PNA backbone enables faster hybridization times—typically within a few hours—and reduces background signals compared to traditional DNA-FISH protocols [44]. This exceptional sensitivity and specificity stems from the absence of electrostatic repulsion between the PNA probe and the negatively charged DNA/RNA target, allowing effective binding even at low probe concentrations [44]. PNA-FISH probes can be designed as molecular beacons that remain quenched in solution but emit strong fluorescence upon hybridization with complementary targets, eliminating the need for complex stem-loop structures required by DNA-based beacons [44]. This technology is particularly valuable for visualizing repetitive genomic sequences, including telomeres, centromeres, and specific gene expansions, in both cells and tissue sections.
Application Notes
PNA-FISH has demonstrated exceptional utility in cytogenetic analysis, microbiological detection, and research applications. For telomere length assessment, PNA Bio provides two distinct probe types: TelC (C-rich, binds TAACCC repeats) and TelG (G-rich, binds TTAGGG repeats), both compatible with human, mouse, rat, and most vertebrate chromosomes [44]. For centromere staining, researchers can select between the CENPB probe (ATTCGTTGGAAACGGGA sequence), which stains all human and mouse centromeres except the Y chromosome, and the CENT probe (AAACTAGACAGAAGCAT sequence), which selectively stains human centromeres with variable intensity across chromosomes [44]. Additionally, the DM1 (CAG Repeat) PNA probe enables detection of expanded CTG/CAG repeats in the DMPK gene associated with Myotonic Dystrophy type 1 [44]. The technology is compatible with various sample types, including FFPE tissues and fixed cell preparations, making it adaptable to both clinical and research settings.
Table 1: Commercial PNA FISH Probes and Their Applications
| Catalog Number | Probe Type | Label | Target Sequence/Application | Compatibility |
|---|---|---|---|---|
| F1002 | TelC-Cy3 | Cy3 | C-rich telomere (CCCTAA repeats) | Human, mouse, rat, etc. |
| F1008 | TelG-A488 | Alexa Fluor 488 | G-rich telomere (TTAGGG repeats) | Human, mouse, rat, etc. |
| F3004 | CENPB-A488 | Alexa Fluor 488 | CENP-B box (ATTCGTTGGAAACGGGA) | Human & mouse centromeres |
| F3003 | CENT-Cy3 | Cy3 | Human alpha satellite (AAACTAGACAGAAGCATT) | Human centromeres only |
| F5001 | (CAG)5-Cy3 | Cy3 | CAG repeats (Myotonic Dystrophy type 1) | DMPK gene |
Detailed Protocol: PNA-FISH for Telomere Visualization
Sample Preparation: Begin with fixed cell preparations on glass slides or FFPE tissue sections. For cells, grow on coverslips and fix with 4% paraformaldehyde for 10 minutes at room temperature, followed by three 5-minute washes in phosphate-buffered saline (PBS). For tissue sections, deparaffinize and rehydrate using standard histology protocols [44].
Hybridization: Prepare hybridization mixture containing PNA FISH Hybridization Buffer (20 mM Tris, 60% formamide, pH 7.4 final) and the appropriate PNA probe (e.g., TelC-Cy3 or TelG-A488) at recommended concentration. Apply 150 μL per slide and cover with RNase-free coverslip. Denature at 80°C for 5 minutes, then hybridize in a humidified chamber at room temperature for 2 hours protected from light [44].
Post-Hybridization Washes: Remove coverslips carefully and wash slides twice in pre-warmed (65°C) wash solution (70% formamide, 10 mM Tris pH 7.2) for 15 minutes each. Follow with three 5-minute washes in PBS at room temperature. Counterstain with DAPI (0.1 μg/mL) for 5 minutes, rinse briefly in PBS, and mount with antifade mounting medium [44].
Visualization and Analysis: Visualize using a fluorescence microscope equipped with appropriate filter sets. Telomeres appear as distinct fluorescent spots at chromosome ends. For quantitative analysis, capture images of multiple nuclei and use specialized software (e.g., Telometer or ImageJ with telomere analysis plugins) to measure telomere fluorescence intensity.
PNA-Mediated PCR Clamping
PNA-mediated PCR clamping utilizes PNA oligomers to selectively inhibit the amplification of specific DNA sequences during polymerase chain reaction. This technique capitalizes on PNAs' higher binding affinity for complementary DNA and their ability to bind sequence-specifically to DNA targets without serving as primers for DNA polymerase [45] [46]. When a PNA molecule binds to its complementary sequence within a PCR target site, it effectively blocks primer binding or polymerase progression, thereby "clamping" amplification of that particular sequence [45]. This mechanism is particularly valuable for suppressing amplification of abundant non-target templates while allowing efficient amplification of rare targets, enabling sensitive detection of mutations, pathogens, or specific genetic variants in complex backgrounds.
Application Notes
A prominent application of PNA PCR clamping involves reducing host chloroplast and mitochondrial 16S rRNA gene amplification in plant microbiome studies. Recent research demonstrates that applying a universal chloroplast PNA clamp and a newly designed mitochondria PNA clamp to oak-associated microbiota reduced host chloroplast and mitochondrial 16S rRNA gene sequences by 79% in leaf, 46% in bark, and 99% in root tissues, respectively [45]. This substantial reduction in host DNA amplification resulted in significant increases in bacterial sequencing reads—72% in leaf, 35% in bark, and 17% in root tissue—and enhanced detection of bacterial diversity with 105 additional ASVs (Amplicon Sequence Variants) in leaves and 218 in bark samples [45]. Unlike mismatching primers that can introduce taxonomic biases, PNA clamps maintain community representation while effectively suppressing dominant host sequences, providing more accurate bacterial community profiles.
Table 2: Performance Metrics of PNA Clamps in Plant Microbiome Studies
| Tissue Type | Reduction in Host Sequences | Increase in Bacterial Reads | Additional ASVs Detected |
|---|---|---|---|
| Leaf | 79% | 72% | 105 |
| Bark | 46% | 35% | 218 |
| Root | 99% | 17% | Not significant |
Detailed Protocol: PNA Clamping for Plant Microbiome Analysis
PNA Clamp Design: Design PNA clamps complementary to conserved regions of host organellar 16S rRNA genes. For universal chloroplast suppression, use the pPNA sequence: GGCTCAACCCTGGACAG. For Quercus mitochondria suppression, use the mPNA sequence: CGCWGCCGCCGCCTTCG (W = A/T) [45]. Synthesize PNAs with a C-terminal lysine amide to improve solubility.
DNA Extraction and PCR Setup: Extract total DNA from plant tissues (leaves, bark, or roots) using a commercial kit with bead-beating for efficient microbial lysis. Set up 25 μL PCR reactions containing: 1× PCR buffer, 2.5 mM MgCl₂, 200 μM dNTPs, 0.4 μM each primer (e.g., 515F and 806R for 16S V4 region), 1.25 U DNA polymerase, 1-10 ng template DNA, and PNA clamps at optimal concentration (typically 1-5 μM for each PNA) [45].
Thermocycling with PNA Clamping: Use the following thermocycling conditions: initial denaturation at 95°C for 3 minutes; 30 cycles of 95°C for 30 seconds, 78°C for 10 seconds (PNA binding step), 55°C for 30 seconds (primer annealing), 68°C for 45 seconds (extension); final extension at 68°C for 5 minutes. The critical 78°C step allows specific PNA binding to host DNA before primer annealing [45].
Downstream Processing: Purify PCR amplicons using magnetic beads or columns, quantify, and prepare libraries for sequencing. Analyze sequencing data using standard microbiome analysis pipelines (QIIME 2, mothur, or DADA2) and compare host sequence contamination and bacterial diversity between PNA-treated and untreated samples.
The mechanism of PNA clamping is visualized in the following diagram:
PNA-Based Biosensors
PNA-based biosensors represent a cutting-edge application of peptide nucleic acids in clinical diagnostics and environmental monitoring. These biosensors leverage PNA's superior hybridization properties, metabolic stability, and resistance to enzymatic degradation for highly specific and sensitive detection of nucleic acid targets and other biomarkers [47] [48]. The neutral PNA backbone reduces electrostatic repulsion with target molecules, enabling enhanced specificity and single-base mismatch discrimination compared to DNA-based sensors. Recent innovations include PNA-functionalized porous silicon biosensors for protein detection and PNA-SERS (Surface-Enhanced Raman Spectroscopy) platforms for viral genomic sequence identification, demonstrating the versatility of PNA as a recognition element in diverse biosensing architectures [47] [48].
Application Notes
PNA biosensors have shown remarkable performance in detecting clinically relevant biomarkers. A truncated PNA-functionalized porous silicon biosensor achieved sensitive detection of human cardiac troponin T (cTnT), a key biomarker for myocardial infarction, with a limit of detection of 0.030 ± 2.0×10⁻⁵ ng mL⁻¹ in the clinically relevant range of 0.02-0.16 ng mL⁻¹ [47]. This biosensor utilized a computationally designed 12-base PNA probe derived from a 40-base wild-type sequence, significantly reducing synthesis costs while maintaining binding efficiency [47]. In infectious disease diagnostics, a PNA-SERS biosensor enabled label-free detection of SARS-CoV-2 genomic sequences in saliva using gold nanoparticles functionalized with PNA probes, providing a rapid, non-invasive diagnostic platform [48]. These applications highlight PNA's advantages in biosensing, including enhanced stability, specificity, and adaptability to various transduction mechanisms.
Table 3: Performance Characteristics of PNA-Based Biosensors
| Biosensor Type | Target | Detection Limit | Dynamic Range | Sample Matrix |
|---|---|---|---|---|
| PSi Optical Biosensor | Cardiac Troponin T | 0.030 ± 2.0×10⁻⁵ ng mL⁻¹ | 0.02-0.16 ng mL⁻¹ | Buffer/Serum |
| PNA-SERS Biosensor | SARS-CoV-2 Genomic RNA | Not specified | Clinically relevant | Saliva |
| PNA-Electrochemical | Point mutations | Single-base mismatch | N/A | Biological samples |
Detailed Protocol: PNA-Functionalized Porous Silicon Biosensor
Porous Silicon (PSi) Fabrication: Electrochemically etch p-type silicon wafers (0.01-0.02 Ω·cm resistivity) in a hydrofluoric acid (HF)/ethanol solution (1:3 v/v) at constant current density (10-100 mA/cm²) for 5-30 seconds to create porous silicon layers with desired porosity and thickness. Characterize the PSi structure by scanning electron microscopy and reflectance spectroscopy [47].
Surface Functionalization: Passivate freshly etched PSi surfaces by thermal hydrosilylation with 10-undecenoic acid at 120°C for 2-4 hours to form a stable monolayer with carboxylic acid termini. Activate carboxylic groups by treating with 20 mM EDC (1-ethyl-3-(3-dimethylaminopropyl)carbodiimide) and 5 mM NHS (N-hydroxysuccinimide) in MES buffer (pH 5.5) for 30 minutes [47].
PNA Immobilization: Covalently immobilize amino-terminated PNA probes (e.g., truncated 12-mer cTnT-specific PNA) onto activated PSi surfaces by incubating with 1-10 μM PNA solution in sodium phosphate buffer (pH 8.0) for 2-4 hours at room temperature. Achieve optimal surface density of 1.12 ± 0.30 pmol cm⁻² through pH-controlled conjugation [47].
Target Detection and Signal Measurement: Incubate PNA-functionalized PSi biosensors with sample containing target (cTnT) for 30-60 minutes. Wash thoroughly to remove unbound molecules. Monitor reflectance spectra changes using a fiber-optic spectrometer equipped with a white light source. Calculate effective optical thickness (EOT) shifts resulting from target binding-induced refractive index changes in the PSi layer. Correlate EOT shifts with target concentration using established calibration curves [47].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for PNA-Based Diagnostic Applications
| Reagent/Category | Specific Examples | Function/Application | Supplier/Reference |
|---|---|---|---|
| PNA FISH Probes | TelC (F1002), TelG (F1008), CENPB (F3004), CENT (F3003) | Chromosomal visualization, telomere/centromere staining | PNA Bio [44] |
| PNA Clamps | Chloroplast PNA (pPNA), Mitochondria PNA (mPNA) | Suppressing host DNA amplification in microbiome studies | Custom synthesis [45] |
| Hybridization Buffers | PNA FISH Hybridization Buffer (PFB01) | Optimized hybridization conditions for PNA probes | PNA Bio [44] |
| Biosensor Substrates | Porous silicon, Gold nanoparticles | Transducer platforms for PNA-based detection | Various suppliers [47] [48] |
| Blocking Buffers | PNA FISH Blocking Buffer (PFB05) | Reducing non-specific binding in hybridization assays | PNA Bio [44] |
Comparative Analysis and Future Perspectives
The three PNA-based diagnostic platforms each offer distinct advantages for specific applications. PNA-FISH provides spatial information and is ideal for cytogenetic studies and microbial identification, with hybridization times reduced to hours compared to traditional FISH protocols [44]. PNA PCR clamping excels in manipulating amplification efficiency, particularly for enriching rare sequences in complex samples like plant microbiomes, where it increased bacterial sequence reads by up to 72% [45]. PNA biosensors offer rapid, sensitive detection with minimal sample processing, exemplified by the truncated PNA biosensor that achieved detection limits clinically relevant for myocardial infarction diagnosis [47].
Future developments in PNA diagnostics will likely focus on enhancing cellular delivery through chemical modifications and nanocarriers, improving multiplexing capabilities for parallel target detection, and developing point-of-care devices leveraging PNA's stability and specificity [43]. Additionally, computational design of truncated PNA probes, as demonstrated with the cTnT biosensor, will make PNA-based diagnostics more cost-effective and accessible [47]. As these technologies mature, PNA-based platforms are poised to play an increasingly important role in molecular diagnostics, therapeutic monitoring, and personalized medicine.
Peptide Nucleic Acids (PNAs) represent a class of synthetic oligonucleotide analogs that combine the molecular recognition properties of DNA with the structural stability of peptides. Since their invention in 1991, PNAs have attracted significant research interest due to their unique pseudopeptide backbone composed of N-(2-aminoethyl)-glycine units, which replaces the sugar-phosphate backbone found in natural nucleic acids [7]. This fundamental structural modification confers several advantageous properties, including exceptional biostability against nucleases and proteases, high binding affinity for complementary DNA and RNA sequences, and superior sequence specificity [4] [30]. These characteristics make PNA technology particularly promising for therapeutic applications where target specificity and metabolic stability are paramount concerns.
The neutral backbone of PNAs eliminates electrostatic repulsion against complementary nucleic acids, resulting in higher thermal stability of PNA-DNA/PNA-RNA duplexes compared to their natural counterparts [49]. This strong and specific binding capacity enables PNAs to effectively inhibit transcription and translation processes through steric blockade, making them excellent candidates for antisense and antigene applications [4] [30]. Despite these favorable properties and demonstrated success in research settings, the transition of PNA-based therapeutics into clinical trials has progressed slower than anticipated, primarily due to challenges associated with cellular delivery and pharmacokinetic optimization [7] [49]. This review comprehensively assesses the current clinical pipeline of PNA drug candidates while providing detailed experimental frameworks for their evaluation.
Current Status of PNA Therapeutics in Clinical Development
Analysis of the Clinical Pipeline
The translation of PNA technology from preclinical research to clinical application represents a critical milestone in the development of nucleic acid therapeutics. A systematic analysis of the current landscape reveals that while numerous PNA-based therapeutic approaches have demonstrated promise in in vitro and animal models, clinical advancement has been limited. Extensive searching of clinical trial registries and medical literature indicates that no PNA drug candidates are currently in registered phase II or III clinical trials for any indication, highlighting the significant translational challenges facing this technology platform [4] [30] [7].
This gap between preclinical promise and clinical application primarily stems from persistent challenges with intracellular delivery and biodistribution rather than questions about the fundamental mechanism of action [7] [49]. The most advanced PNA applications have primarily emerged in diagnostic realms, such as Attralus's pan-amyloid diagnostic imaging agent 124I-evuzamitide, which has demonstrated 100% sensitivity and specificity for detecting cardiac amyloidosis in clinical studies [50]. For therapeutic applications, research continues to focus on overcoming delivery barriers through various strategies, including nanoparticle formulations, cell-penetrating peptide conjugates, and chemical modifications to improve pharmacokinetic properties [4] [7].
Promising Preclinical Candidates
Although clinical-stage PNA therapeutics remain limited, several promising preclinical candidates demonstrate the potential of this technology across diverse therapeutic areas:
Table: Promising Preclinical Applications of PNA Therapeutics
| Therapeutic Area | Molecular Target | Proposed Mechanism | Development Status |
|---|---|---|---|
| Oncology | miR-155, MYCN, RAD51 | Antisense inhibition of oncogenes | In vitro and animal models [4] |
| Infectious Diseases | Bacterial mRNA | Gene-specific antibacterial activity | In vitro models [51] |
| Genetic Disorders | Dystrophin gene | Gene editing for Duchenne muscular dystrophy | Ex vivo and animal models [4] |
| Hepatitis | HBV RNA | Antisense inhibition of viral replication | Cell line and animal models [4] |
The antibacterial applications of PNAs have shown particular promise, with demonstrated efficacy against a range of pathogenic bacteria including Escherichia coli and Staphylococcus aureus [51]. PNA antibacterials typically exhibit minimum inhibitory concentrations (MIC) in the micromolar range, with their efficiency influenced by factors such as PNA length, binding location, and carrier system [51]. These gene-specific antibacterial agents offer a novel approach to addressing the growing crisis of antimicrobial resistance by targeting essential bacterial genes with high specificity.
Experimental Protocols for PNA Therapeutic Development
Protocol 1:In VitroAssessment of PNA Efficacy
PNA Design and Synthesis
- Sequence Selection: Identify a 12-18 base pair target sequence with high specificity to the intended gene target. For antisense applications, target the AUG start codon region or 5' untranslated region (5'UTR) of mRNA for translational blockade [30].
- Backbone Modification: Incorporate (R)-diethylene glycol "miniPEG" chains at the γ-backbone position to improve solubility and hybridization efficiency [7].
- Synthesis Method: Employ Fmoc (9-fluorenylmethoxycarbonyl) solid-phase peptide synthesis protocols using established methodologies [4]. Purify the resulting PNA oligomer using reverse-phase high-performance liquid chromatography (HPLC) and verify identity by mass spectrometry.
- Quality Control: Confirm PNA concentration spectrophotometrically and assess purity (>95%) by analytical HPLC.
Cell Culture and Transfection
- Cell Line Selection: Choose appropriate cell lines that express the target gene. For cancer applications, human glioma cell lines (e.g., U87) are relevant for targeting miR-21 [30].
- PNA Delivery: Utilize cell-penetrating peptides (CPPs) conjugated to PNA to enhance cellular uptake. Effective CPPs include penetratin (RQIKIWFQNRRMKWKK) or oligoarginine (typically 8-9 arginine residues) [4] [7].
- Transfection Protocol:
- Culture cells in appropriate medium (e.g., DMEM for glioma cells) with 10% fetal bovine serum at 37°C in 5% CO₂.
- Incubate PNA-CPP conjugates (0.5-20 μM concentration range) with cells for 24-48 hours.
- Include controls: untreated cells, scrambled PNA sequence, and CPP alone.
- Uptake Enhancement: For challenging cell lines, include endosome-disruptive agents such as chloroquine (50-100 μM) to enhance endosomal escape [4].
Efficacy Assessment
- mRNA Quantification: Isolate total RNA 48 hours post-transfection using TRIzol reagent. Perform quantitative RT-PCR to measure target mRNA levels, normalizing to housekeeping genes (e.g., GAPDH, β-actin).
- Protein Analysis: Harvest cells 72 hours post-transfection for Western blot analysis to assess target protein suppression.
- Phenotypic Assays: Conduct appropriate functional assays (e.g., MTT assay for viability, flow cytometry for apoptosis) to correlate molecular effects with phenotypic changes.
Diagram 1: Workflow for in vitro assessment of PNA efficacy, showing key stages from PNA design through phenotypic assessment.
Protocol 2:In VivoEvaluation of PNA Therapeutics
Animal Model Selection
- Disease Models: Select appropriate animal models that recapitulate the human disease pathology. For cancer applications, use xenograft models (e.g., nude mice with implanted human tumor cells). For genetic disorders, employ genetically engineered models (e.g., mdx mice for Duchenne muscular dystrophy) [4].
- Group Allocation: Randomize animals into experimental groups (n=6-10 per group):
- Treatment group (PNA therapeutic)
- Vehicle control group
- Positive control (existing standard therapy if available)
- Scrambled PNA sequence control
Formulation and Administration
- Delivery Optimization: Based on target tissue, employ appropriate delivery strategies:
- Dosing Regimen: Administer PNA therapeutic via appropriate route (intravenous, intraperitoneal, or local injection) at doses ranging from 5-20 mg/kg, with frequency based on pharmacokinetic properties (typically 2-3 times per week for 3-4 weeks).
Efficacy and Safety Assessment
- Biodistribution Analysis: For pharmacokinetic studies, use radiolabeled or fluorophore-conjugated PNAs to track tissue distribution over time. Quantify PNA concentrations in target tissues using appropriate methodologies (e.g., fluorescence imaging, liquid scintillation counting).
- Efficacy Endpoints:
- For oncology: Measure tumor volume regularly, harvest tumors at endpoint for molecular analysis (target gene/protein expression).
- For genetic disorders: Assess functional improvement (e.g., grip strength for muscular dystrophy models) and molecular correction (e.g., PCR analysis of gene expression).
- Safety Evaluation:
- Monitor body weight, behavior, and clinical signs daily.
- Collect blood for hematological and clinical chemistry analysis at study endpoint.
- Perform histopathological examination of major organs (liver, kidney, heart, etc.).
Table: Key Research Reagent Solutions for PNA Therapeutic Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell-Penetrating Peptides | Penetratin, Oligoarginine (R8-R9), TAT peptide | Enhance cellular uptake of PNA conjugates [4] [7] |
| Backbone Modifications | miniPEG-γ-PNA, Lysine-PNA conjugates | Improve solubility and binding affinity [7] |
| Delivery Systems | PLGA nanoparticles, Cationic liposomes, Polymeric micelles | Enhance stability and biodistribution in vivo [7] |
| Endosomal Escape Agents | Chloroquine, Calcium ions | Promote release of internalized PNAs from endosomes [4] |
| Detection Reagents | Fluorophore-conjugated PNAs (FITC, Cy5), Radioactive labels (¹²⁴I, ⁹⁹mTc) | Track cellular uptake and biodistribution [50] |
Mechanisms of PNA Action and Signaling Pathways
PNAs exert their therapeutic effects through multiple mechanisms of action depending on their cellular target and design. Understanding these mechanisms is essential for rational PNA therapeutic development.
Antisense Mechanisms
Antisense PNAs primarily target RNA species through several distinct mechanisms:
Splicing Modulation: PNAs targeting pre-mRNA can alter splicing patterns through:
- Exon skipping to exclude mutated regions and restore reading frames
- Exon inclusion to prevent inappropriate splicing
- Intron retention to produce non-functional transcripts [30]
The process involves PNA binding to splice donor/acceptor sites or splicing enhancer/silencer sequences, creating steric hindrance that prevents spliceosome assembly or function.
Translational Inhibition: PNAs can block protein synthesis through:
- Ribosome assembly blockade by targeting the 5'UTR or AUG start codon region
- Elongation arrest by binding to coding regions and sterically hindering ribosomal progression [30]
microRNA Inhibition: Anti-miR PNAs can sequester oncogenic microRNAs (e.g., miR-155, miR-21), preventing their interaction with target mRNAs and derepressing tumor suppressor genes [30].
Diagram 2: PNA antisense mechanisms of action showing three primary pathways for gene expression modulation.
Antigene Mechanisms
PNAs can directly target genomic DNA through unique structural interactions:
Triplex Invasion: bis-PNAs (two PNA strands linked together) can invade double-stranded DNA at homopurine sequences, forming a PNA₂-DNA triplex with one strand bound via Watson-Crick base pairing and the other via Hoogsteen binding. This creates a P-loop structure that can inhibit transcription factor binding or block transcriptional elongation [49].
Double Duplex Invasion: Pseudocomplementary PNAs (pcPNAs) containing modified bases (diaminopurine instead of adenine, thiouracil instead of thymine) can simultaneously invade both strands of double-stranded DNA, each binding to its complementary strand. This approach doesn't require homopurine stretches and can effectively inhibit transcription [49].
The exceptional binding affinity and specificity of PNAs for DNA sequences, combined with their resistance to enzymatic degradation, make them particularly suitable for antigene applications, though intracellular delivery to the nucleus remains a significant challenge.
Challenges and Future Directions in PNA Therapeutic Development
Addressing Delivery Challenges
The primary obstacle to clinical advancement of PNA therapeutics remains efficient intracellular delivery. Current research focuses on several promising strategies:
Advanced Nanocarrier Systems: Development of stimuli-responsive nanoparticles that release their PNA payload in response to specific intracellular signals (e.g., pH changes in endosomes, enzyme activity) [7]. These systems can be further functionalized with targeting ligands (antibodies, peptides, aptamers) for tissue-specific delivery.
Chemical Modifications: Structural optimization of PNA backbones to improve pharmacokinetic properties while maintaining binding affinity. γ-Backbone modifications (e.g., miniPEG) have shown particular promise in enhancing solubility and cellular uptake without compromising target affinity [7].
Endosomal Escape Technologies: Development of novel endosomolytic agents and conjugation strategies to promote release of internalized PNAs from endocytic vesicles, including photochemical internalization approaches and pH-responsive polymers [4].
Clinical Translation Considerations
For successful translation of PNA therapeutics to clinical application, several key areas require focused attention:
Comprehensive Toxicology Assessment: Establishment of robust toxicological screening protocols specific to PNA chemistry, including assessment of potential off-target effects and immune stimulation.
Scalable Manufacturing Processes: Development of cost-effective, scalable synthesis and purification methods compliant with Good Manufacturing Practice (GMP) standards to enable commercial viability.
Biomarker-Driven Clinical Development: Identification of predictive biomarkers for patient stratification and early assessment of target engagement in clinical trials, potentially leveraging the diagnostic applications of PNA technology [50].
The ongoing research into PNA delivery systems and continued refinement of PNA design principles provide optimism that these challenges can be overcome, potentially unlocking the considerable therapeutic potential of this unique class of nucleic acid analogs.
Overcoming the Hurdles: Delivery Challenges and Optimization Strategies for PNA
Peptide Nucleic Acids (PNAs) represent a transformative class of synthetic nucleic acid analogs with significant potential in therapeutics and diagnostics. Their unique N-(2-aminoethyl)glycine backbone replaces the sugar-phosphate backbone of natural nucleic acids, conferring exceptional binding affinity, stability against enzymatic degradation, and resistance to nucleases and proteases [51] [14]. These properties make PNAs ideal for applications requiring high specificity and durability, such as antisense therapy, gene regulation, and molecular diagnostics [14].
However, the journey from compelling preclinical data to demonstrated clinical efficacy—a critical phase often termed the "Valley of Death"—presents substantial challenges for PNA-based technologies. A primary obstacle is their limited ability to cross cell membranes due to the absence of a natural charge, which restricts intracellular delivery and bioavailability [14]. Furthermore, achieving target specificity and developing scalable manufacturing processes under Good Manufacturing Practice (GMP) standards present additional translational barriers [52]. This Application Note provides detailed protocols and strategic frameworks designed to help researchers navigate these critical challenges, focusing on robust delivery systems and validated diagnostic applications.
Bridging the Gap: Strategic Frameworks and Essential Toolkits
The Scientist's Toolkit: Key Research Reagent Solutions
Successful PNA application relies on a core set of reagents and materials. The table below details essential components for developing and implementing PNA-based experiments.
Table 1: Essential Research Reagent Solutions for PNA Applications
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| Cell-Penetrating Peptides (CPPs) [14] | Enhances cellular uptake of PNA molecules via non-covalent complex formation. | Cationic nature (e.g., TP10, Tat); often includes Nuclear Localization Signal (NLS). |
| PNA Monomers [14] | Solid-phase synthesis of custom PNA oligomers. | Fmoc/Bhoc-protected for standard synthesis protocols. |
| Fluorescent Dyes (e.g., NHS-fluorescein) [14] | Labels PNA molecules for tracking cellular uptake and localization. | Succinimidyl ester group for covalent conjugation. |
| Solid-Phase Support Resin [14] | Foundation for automated PNA and peptide synthesis. | e.g., Fmoc-XAL-PEG-PS resin. |
| Magnetic/Nanoparticle Conjugates [52] | Platforms for targeted delivery and diagnostic sensing. | e.g., Gold or iron oxide nanoparticles for diagnostics and imaging. |
| Biotin Conjugates [52] | Acts as an affinity tag in pull-down assays for molecular interaction studies. | High-affinity binding to streptavidin. |
Visualizing the Translational Pathway: From Bench to Bedside
The following workflow diagram maps the critical stages and decision points in translating a PNA application from preclinical research to clinical implementation.
Application Note: Optimizing CPP-Mediated PNA Delivery for Therapeutic Efficacy
Background and Principle
Overcoming the cellular delivery barrier is a pivotal first step in translating PNA therapeutics. This protocol details a method for using Cell-Penetrating Peptides (CPPs) to efficiently deliver PNA molecules into cells, a strategy proven to enhance uptake while maintaining bioactivity [14]. The approach uses non-covalent complexes between cationic CPPs and neutral PNA molecules, facilitating translocation across cell membranes. An integrated Nuclear Localization Signal (NLS) further directs the cargo to the nucleus, which is essential for gene-targeting applications.
Detailed Experimental Protocol
Materials and Reagents
- Synthesized PNA Oligomer: Target-specific PNA (e.g., anti-ACLY or anti-PCSK9 sequence) with a C-terminal NLS sequence (e.g., Pro-Lys-Lys-Lys-Arg-Lys-Val-amide) [14].
- Cell-Penetrating Peptides: TP10, Tat, or TD2.2, synthesized and purified to >95% purity [14].
- Cell Line: Relevant mammalian cell line for the therapeutic target (e.g., HepG2 for PCSK9 studies).
- Serum-free Cell Culture Medium.
- Fluorescence Microscope or Flow Cytometer (for quantitative uptake assessment if PNA is fluorescein-labeled).
Step-by-Step Procedure
PNA-CPP Complex Formation:
- Prepare stock solutions of PNA and CPP in sterile deionized water.
- In a microcentrifuge tube, combine PNA and CPP at various molar ratios (e.g., 1:5, 1:10, 1:20 PNA:CPP) in serum-free medium. A typical starting point is a 1:10 ratio.
- Vortex the mixture gently and incubate at room temperature for 30-45 minutes to allow non-covalent complex formation.
Cell Treatment:
- Plate cells in a 24-well plate at a density of ( 1 \times 10^5 ) cells per well and culture until ~80% confluency.
- Aspirate the growth medium and wash cells once with phosphate-buffered saline (PBS).
- Add the pre-formed PNA-CPP complexes in serum-free medium to the cells.
- Incubate cells with complexes at 37°C in a 5% CO₂ incubator for 4-24 hours.
Complex Removal and Cell Analysis:
- After incubation, carefully remove the treatment medium.
- Wash cells twice with PBS to remove any residual complexes.
- (If PNA is fluorescently labeled) Analyze cellular uptake directly via fluorescence microscopy or by trypsinizing cells and analyzing via flow cytometry.
- (For functional assays) Proceed with downstream applications, such as RNA/DNA extraction for RT-qPCR to assess gene expression modulation or Western Blot to evaluate target protein levels.
Critical Success Factors and Validation
- CPP Selection: Empirical testing is crucial. In comparative studies, TP10 demonstrated superior delivery efficiency over Tat and TD2.2 for certain PNA constructs [14].
- Molar Ratio Optimization: The PNA:CPP ratio must be optimized for each new PNA sequence and CPP to balance efficiency with potential cytotoxicity. A dose-response MTT assay should be performed to ensure biocompatibility.
- Functional Validation: Successful delivery must be confirmed by a functional endpoint, such as a significant reduction in the target mRNA or protein level, confirming the biological activity of the delivered PNA.
Application Note: A PNA-Based Diagnostic Assay for Rifampicin-Resistant Tuberculosis
Background and Principle
Rapid, specific, and accessible diagnostics are a critical application for PNA technology. This protocol describes a PNA-paper-based sensor for detecting specific mutations in the M. tuberculosis rpoB gene (codons 516, 526, and 531) associated with Rifampicin resistance [53]. The assay combines isothermal Recombinase Polymerase Amplification (RPA) for rapid DNA amplification with highly specific PNA probes immobilized on a paper substrate. The principle is reverse hybridization: the PNA probe generates a colorimetric signal only when it perfectly binds to the wild-type sequence, enabling the discrimination of single-base mutations without sophisticated instrumentation.
Detailed Experimental Protocol
Materials and Reagents
- PNA Probes: Designed against wild-type rpoB sequences (e.g., for codons 516, 526, 531), synthesized via Fmoc solid-phase synthesis and HPLC-purified [53].
- Primers: Forward and biotin-tagged reverse primers specific for the rpoB RRDR region.
- TwistAmp Basic RPA Kit (TwistDx Limited).
- Filter Paper: Whatman qualitative filter paper, Grade 1.
- Chemical Activation Reagents: Carboxymethyl cellulose, EDC, NHS.
- Color Development Reagents: Streptavidin-Horseradish Peroxidase (Streptavidin-HRP), TMB substrate.
Step-by-Step Procedure
Part A: Preparation of PNA-Paper Sensor
- Functionalize Paper: Incubate filter paper in carboxymethyl cellulose solution (2 mg/mL) for 90 minutes, followed by washing.
- Activate Surface: Treat the paper with a fresh EDC/NHS solution (0.1 M / 0.4 M) for 20 minutes to activate carboxyl groups. Wash and dry.
- Spot PNA Probes: Spot 0.4 µL of PNA solution (50-200 µM) onto predefined grid squares on the activated paper.
- Immobilize: Place the spotted paper in a humid chamber overnight to complete covalent immobilization.
- Store: Wash the paper, dry it, and store it in a desiccator until use.
Part B: Sample Amplification and Detection
- DNA Extraction: Extract genomic DNA from M. tuberculosis colonies using a simple boiling method.
- Multiplex RPA:
- Prepare a 50 µL RPA reaction mix using the TwistAmp kit, including primers and the DNA template.
- Initiate the reaction by adding Mg(OAc)₂ and incubate at 37°C for 20 minutes.
- Hybridization and Detection:
- Dilute 20 µL of the RPA product and apply it to the PNA-paper sensor.
- Incubate for 15 minutes to allow hybridization between the biotinylated amplicon and the immobilized PNA probe.
- Wash the paper to remove unbound material.
- Add Streptavidin-HRP conjugate, incubate, and wash again.
- Add TMB substrate. A deep blue spot develops within minutes if the wild-type sequence is present. The absence of a spot indicates a mutation (mismatch) at the target codon.
Performance Metrics and Advantages
This assay has demonstrated [53]:
- 100% Accuracy in detecting targeted rpoB mutations.
- Short Turnaround Time: ~110 minutes from sample to result.
- Ultra-sensitivity and no cross-reactivity with other bacterial pathogens.
- Resource-Limited Suitability: The paper-based, isothermal format eliminates the need for expensive thermocyclers, making it ideal for point-of-care settings.
Visualizing the Diagnostic Workflow
The diagnostic process, from sample preparation to result interpretation, is streamlined into a single workflow as depicted below.
Quantitative Efficacy Data and Clinical Outlook
Therapeutic PNA Efficacy
The therapeutic potential of PNAs is supported by robust preclinical data. A systematic review of PNA antibacterials found that optimized constructs exhibit efficacy at micromolar concentrations, demonstrating their potential as target-based agents [51].
Table 2: Preclinical Efficacy of Representative Antibacterial PNA Constructs
| Target Bacteria | Target Gene | PNA Construct Details | Reported Efficacy (MIC) | Key Design Factor |
|---|---|---|---|---|
| Escherichia coli [51] | Various Essential Genes | Anti-sense PNA (10-15 mer) | Low Micromolar Range (e.g., 2-10 µM) | Conjugation to CPPs like (KFF)₃K |
| Staphylococcus aureus [51] | Various Essential Genes | Anti-sense PNA (10-15 mer) | Low Micromolar Range (e.g., 1-8 µM) | Optimized binding location & length |
Market and Regulatory Trajectory
The transition of PNA technologies from research to clinic is underpinned by a growing and evolving market. Strategic recommendations for industry leaders include establishing multi-disciplinary collaborations, investing in scalable manufacturing like flow chemistry, and proactive engagement with regulatory bodies to clarify approval pathways for these novel modalities [52]. The PNA conjugates market is projected to grow significantly from 2025 to 2030, driven by advancements in conjugation chemistries and an increasing focus on personalized medicine [52].
Peptide Nucleic Acids (PNAs) are synthetic molecules with a peptide-like backbone that demonstrates remarkable affinity and specificity for complementary DNA and RNA sequences [12]. Their unique N-(2-aminoethyl)glycine backbone replaces the sugar-phosphate backbone of natural nucleic acids, endowing them with high biological stability, resistance to nuclease and protease degradation, and strong hybridization properties [14] [54]. These characteristics make PNAs powerful tools for therapeutic applications including gene editing, antisense therapy, and molecular diagnostics [54] [8]. However, the same neutral, uncharged backbone that confers these advantages also creates a significant cellular delivery challenge [43]. Unlike charged oligonucleotides, PNAs are highly hydrophobic and cannot leverage electrostatic interactions to facilitate cell membrane crossing, making them essentially impermeable to cellular membranes without assisted delivery strategies [12] [43].
The covalent conjugation of PNAs to Cell-Penetrating Peptides (CPPs) has emerged as a leading strategy to overcome this critical delivery barrier [12]. CPPs are short peptides (typically 5-30 amino acids) characterized by their ability to transverse cell membranes and facilitate the intracellular delivery of various molecular cargoes [55]. Rich in basic residues like arginine and lysine, CPPs interact efficiently with cellular membranes through diverse entry mechanisms including direct penetration and endocytosis [55]. This application note details standardized protocols for covalently coupling PNAs to CPPs, framing these methodologies within the broader context of enhancing PNA applications in therapeutics and diagnostics research.
CPP Mechanisms and Selection for PNA Delivery
Classification of Cell-Penetrating Peptides
CPPs can be categorized based on their physicochemical properties, which directly influence their mechanism of cellular entry and suitability for PNA delivery [55]. The table below outlines the primary classes of CPPs and their characteristics:
Table 1: Classification of Cell-Penetrating Peptides Relevant to PNA Delivery
| Class | Representative Sequences | Key Properties | Mechanisms of Uptake | References |
|---|---|---|---|---|
| Cationic | TAT (YGRKKRRQRRR), Penetratin (RQIKIWFQNRRMKWKK), R9 (Poly-arginine) | Rich in basic residues (Arg, Lys); positively charged at physiological pH | Macropinocytosis, clathrin-mediated endocytosis, caveolae-mediated endocytosis | [55] |
| Amphipathic | MPG (GALFLGFLGAAGSTMGAWSQPKKKRKV), Transportan (GWTLNSAGYLLG-K-INLKALAALAKKIL) | Contain hydrophobic and hydrophilic domains; often form alpha-helices | Direct penetration, endocytosis, inverted micelle formation | [55] |
| Hydrophobic | TP10 (AGYLLGKINLKALAALAKKIL), C105Y (CSIPPEVKFNKPFVYLI) | Predominantly non-polar residues; high membrane affinity | Direct penetration, endocytosis | [55] |
| Chimeric | Pep-1 (KETWWETWWTEW-SQP-KKKRKV) | Engineered hybrids combining functional domains from different classes | Often combine multiple uptake mechanisms | [55] |
Cellular Uptake Mechanisms
CPPs facilitate cellular entry through two primary mechanistic pathways: direct penetration and endocytosis [55]. The specific pathway utilized depends on the CPP's properties, the conjugated cargo, and the target cell type.
- Direct Penetration: This mechanism involves the direct translocation of the CPP-PNA conjugate across the lipid bilayer, often through transient pore formation or the "inverted micelle" model, where the peptide interacts with membrane lipids to create a transient structure that facilitates passage [55]. This pathway is typically energy-independent and can deliver cargo directly to the cytoplasm, avoiding entrapment in endosomal compartments [55].
- Endocytosis: This energy-dependent process encompasses several subtypes, including macropinocytosis, clathrin-mediated endocytosis, and caveolae-mediated endocytosis [55]. While efficient for uptake, this mechanism sequesters the CPP-PNA conjugate within endosomal vesicles, from which it must escape to reach its intracellular targets (e.g., nucleus or cytoplasm). Endosomal escape remains a significant bottleneck for CPP efficiency [55].
The following diagram illustrates the logical relationship between CPP classes and their primary entry mechanisms:
Covalent Conjugation Strategies and Protocols
Covalent conjugation creates a stable, chemically defined linkage between the PNA and CPP, ensuring a consistent 1:1 molar ratio and enhancing pharmacokinetic properties. The following protocol outlines a standard approach for covalent conjugation via a cleavable disulfide bond, which is stable in the extracellular environment but cleaves in the reducing intracellular environment to release the PNA cargo.
Protocol: Covalent Conjugation via Disulfide Linkage
Principle: This method utilizes cysteine residues incorporated into the PNA and CPP sequences to form a reversible disulfide bridge. The protocol assumes the PNA has been synthesized with a C-terminal cysteine and the CPP has an N-terminal cysteine.
Materials:
- Synthesized PNA with C-terminal Cysteine: Purified via HPLC, lyophilized.
- Synthesized CPP with N-terminal Cysteine: Purified via HPLC, lyophilized.
- Dimethyl sulfoxide (DMSO): Anhydrous grade.
- 0.1 M Sodium Phosphate Buffer (pH 7.2): Containing 1 mM EDTA.
- Oxidizing Agent: Dimethyl sulfoxide (DMSO) acts as a mild oxidant.
- C18 Reverse-Phase HPLC Column
- LC-MS System: For analysis and quality control.
Procedure:
- Preparation of Stock Solutions: Dissolve the PNA-Cys and CPP-Cys separately in degassed 0.1 M sodium phosphate buffer (pH 7.2, 1 mM EDTA) to a final concentration of 1 mM.
- Conjugation Reaction: Combine the PNA and CPP solutions at a 1:1.2 molar ratio (PNA:CPP) in a low-protein-binding microcentrifuge tube. Add DMSO to a final concentration of 10% (v/v) to facilitate gentle oxidation.
- Incubation: Allow the reaction to proceed for 12-16 hours (overnight) at room temperature under gentle agitation in the dark.
- Purification: Purify the conjugate using semi-preparative C18 Reverse-Phase HPLC. A linear gradient of 5% to 65% acetonitrile in 0.1% aqueous trifluoroacetic acid over 30 minutes is typically effective for resolving the conjugate from unreacted starting materials.
- Analysis and Characterization: Analyze the collected fractions by LC-MS to confirm the identity and purity (>95%) of the CPP-PNA conjugate. Lyophilize the pure fractions and store at -20°C.
The Scientist's Toolkit: Essential Reagents for CPP-PNA Conjugation
Table 2: Key Research Reagent Solutions for Covalent CPP-PNA Conjugation
| Reagent/Material | Function/Description | Critical Parameters |
|---|---|---|
| Fmoc-PNA Monomers | Building blocks for solid-phase PNA synthesis. Bhoc protection is commonly used for nucleobases. | Panagene is a cited commercial source [14]. |
| Fmoc-Amino Acids | Building blocks for CPP synthesis via SPPS. | Include standard and modified amino acids (e.g., D-isomers) for peptide engineering [14]. |
| Solid Support (XAL-PEG-PS Resin) | A polystyrene-based resin used as a solid support for both PNA and peptide synthesis. | Functionalized with a handle for cleavable amide linkage [14]. |
| C18 Reverse-Phase HPLC Columns | For analytical and preparative purification of PNAs, CPPs, and final conjugates. | Essential for separating hydrophobic molecules and ensuring high purity [14] [15]. |
| LC-MS System | For quality control, verifying molecular weight, and assessing purity of synthesized compounds. | Electrospray Ionization (ESI) is suitable for the mass range of CPP-PNA conjugates [14]. |
| Coupling Reagents (e.g., HBTU/HATU) | Activates Fmoc-amino acids and Fmoc-PNA monomers for coupling to the growing chain on the solid support. | Standard for Fmoc-SPPS protocols [14]. |
Experimental Workflow for Evaluating Conjugate Efficacy
The following comprehensive workflow details the steps from conjugate design through functional validation in cellular models.
Protocol: Cellular Uptake and Efficacy Assay
This protocol evaluates the cellular delivery efficiency and functional activity of the CPP-PNA conjugate, using a fluorescein-labeled PNA as an example.
Materials:
- Cell Line: Adherent cells relevant to the target (e.g., HeLa, HEK293).
- CPP-PNA Conjugate: Fluorescein-labeled (Fluo-PNA-CPP), dissolved in sterile PBS or media.
- Scrambled PNA Conjugate: Control conjugate with a non-targeting PNA sequence.
- Cell Culture Media: Appropriate complete medium (e.g., DMEM + 10% FBS).
- Fixative: 4% paraformaldehyde (PFA) in PBS.
- Nuclear Stain: DAPI (4',6-diamidino-2-phenylindole).
- Lysis Buffer: RIPA buffer for protein extraction.
- Antibodies: For target protein detection via Western Blot.
Procedure:
- Cell Seeding: Seed cells in 24-well plates (with coverslips for microscopy) at a density of 5 x 10^4 cells per well. Incubate for 24 hours to achieve 70-80% confluency.
- Treatment: Dilute the Fluo-PNA-CPP conjugate in serum-free medium to the desired concentration (typically 1-10 µM based on optimization). Replace the medium in the wells with the treatment solution. Include controls: untreated cells and cells treated with a scrambled PNA conjugate.
- Incubation: Incubate cells with the conjugate for 4-6 hours at 37°C in a 5% CO2 incubator.
- Analysis of Cellular Uptake:
- Fluorescence Microscopy: Wash cells with PBS, fix with 4% PFA for 15 minutes, and mount coverslips with mounting medium containing DAPI. Image using a fluorescence microscope. Co-localization of green (fluorescein) and blue (DAPI) signals indicates successful nuclear delivery.
- Flow Cytometry: After treatment, trypsinize cells, wash with PBS, and resuspend in FACS buffer. Analyze fluorescence intensity of at least 10,000 cells per sample using a flow cytometer to quantify uptake efficiency.
- Assessment of Functional Efficacy:
- Western Blot Analysis: After treatment (e.g., 24-48 hours), lyse cells in RIPA buffer. Separate proteins by SDS-PAGE, transfer to a membrane, and probe with antibodies against the target protein (e.g., PCSK9 or ACLY, as cited in recent research [14]). Compare band intensity to a loading control (e.g., GAPDH) to assess knockdown efficiency.
- Viability Assay (MTT): Seed cells in a 96-well plate. After treatment with conjugates, add MTT reagent and incubate for 3-4 hours. Solubilize the formed formazan crystals and measure absorbance at 570 nm. Calculate cell viability relative to untreated controls.
Data Analysis and Optimization
Quantitative Evaluation of CPP Efficiency
Recent research directly compared the efficacy of different CPPs for PNA delivery. The following table summarizes quantitative findings from a 2025 study that evaluated TP10, Tat, and TD2.2 for delivering anti-ACLY and anti-PCSK9 PNAs, highlighting the importance of CPP selection [14].
Table 3: Comparative Efficiency of CPPs for PNA Delivery (Adapted from Polak et al., 2025)
| Cell-Penetrating Peptide (CPP) | Relative Delivery Efficiency | Key Findings and Experimental Context |
|---|---|---|
| TP10 | High (Most Effective) | Demonstrated superior efficiency in delivering NLS-equipped PNAs to the nucleus compared to Tat and TD2.2 in cellular models [14]. |
| Tat | Moderate | A well-established cationic CPP, but was less effective than TP10 in the side-by-side comparison for this specific PNA application [14]. |
| TD2.2 | Lower | Showed measurable but lower delivery efficiency under the tested experimental conditions [14]. |
Troubleshooting Common Issues
- Low Cellular Uptake: Optimize the CPP:PNA molar ratio during conjugation. Consider switching the class of CPP (e.g., from cationic to amphipathic) or incorporating an endosomal escape agent to enhance cytosolic delivery [55] [43].
- High Cytotoxicity: Titrate the working concentration of the conjugate. Ensure the conjugate is highly purified to remove residual organic solvents or reagents. Evaluate the inherent toxicity of the CPP itself using an MTT assay [14].
- Lack of Biological Activity (Despite Good Uptake): Verify the PNA sequence is correctly targeted and accessible. The conjugate may be trapped in endosomes; consider strategies to promote endosomal escape or use photochemical internalization techniques [43]. Ensure the PNA is designed for its intended function (e.g., antisense inhibition requires targeting the translation start site or splice junctions) [54].
Covalent coupling with cell-penetrating peptides represents a robust and widely adopted solution to the critical challenge of PNA delivery [14] [12]. The protocols and data presented herein provide a foundational framework for researchers to design, synthesize, and validate CPP-PNA conjugates. The selection of an appropriate CPP, such as the highly effective TP10, a rational conjugation strategy, and thorough in vitro validation are paramount to success [14]. As PNA technology continues to advance in fields like gene editing, antisense therapy, and molecular diagnostics, optimized delivery protocols will be instrumental in translating these powerful synthetic molecules into tangible diagnostic and therapeutic applications [54] [56].
Peptide Nucleic Acid (PNA) is a synthetic polymer analog of DNA and RNA, first reported in 1991, in which the entire sugar-phosphate backbone is replaced by repeating units of N-(2-aminoethyl)glycine [57] [1]. This fundamental structural alteration confers several intrinsic advantages over natural nucleic acids, including exceptional affinity and sequence selectivity for complementary DNA and RNA, high chemical stability, and strong resistance to enzymatic degradation by both nucleases and proteases [57] [1]. The neutral, pseudopeptide backbone eliminates the electrostatic repulsion that occurs between natural, negatively charged nucleic acids, resulting in PNA/RNA duplexes with significantly higher thermal stability than their natural counterparts [1] [58].
Despite these superior binding properties, the application of unmodified PNAs in therapeutics and diagnostics has been hindered by two primary challenges: poor cellular uptake due to the neutral backbone and a tendency for endosomal entrapment [58]. Consequently, significant research efforts have been directed toward the chemical modification of PNA to overcome these barriers while preserving or even enhancing its favorable hybridization characteristics. This document details key protocols and application notes for the development and use of modified PNAs, particularly Guanidine-modified PNA (GPNA) and other backbone tweaks, providing researchers with the methodologies needed to advance PNA-based therapeutic and diagnostic applications.
GPNA: A Cationic Backbone Modification
Concept and Synthesis of GPNA
Guanidine-modified PNA (GPNA) represents a strategic advancement in PNA technology wherein guanidine groups are incorporated directly into the PNA backbone. This modification aims to enhance the cellular delivery and binding affinity of classical PNA oligomers [58]. The guanidine group, being highly cationic at physiological pH, mimics the function of cell-penetrating peptides (CPPs) like polyarginine, but as an integral part of the molecular structure.
The synthesis of GPNA monomers involves custom synthesis starting from diaminoethane and the chiral amino acid L- or D-arginine, rather than glycine [58]. This results in a chiral center at the α-position of the backbone. The guanidine moiety can be introduced at either the α-position or the γ-position of the PNA backbone, with the stereochemistry and position significantly influencing the oligomer's properties [58].
- α-GPNA: Derived from D-arginine, this isomer has been reported to exhibit higher affinity for complementary DNA and RNA compared to the L-isomer [58].
- γ-GPNA: This modification involves attaching the guanidinium group to the γ-carbon of the backbone. The γ-(S)-isomer (derived from natural L-lysine) typically demonstrates superior affinity for complementary DNA compared to the γ-(R)-isomer, likely due to a favorable preorganization of the backbone into a right-handed helix [58].
Table 1: Comparative Properties of α-GPNA and γ-GPNA
| Property | α-GPNA | γ-GPNA | Unmodified PNA |
|---|---|---|---|
| Backbone Chirality | Chiral | Chiral | Achiral |
| Preferred Stereoisomer | D-arginine derived | L-lysine derived (S) | Not Applicable |
| Binding Affinity for DNA/RNA | High | Higher than α-GPNA | High |
| Cellular Uptake | Enhanced, efficient in various cell lines (e.g., HCT116, HeLa) | Enhanced, efficient in various cell lines | Poor |
| Sequence Selectivity | Maintained | Maintained | High, a single mismatch is highly destabilizing |
Protocol: Evaluating GPNA Performance in miRNA Inhibition
The following protocol outlines the steps for assessing the efficacy of a GPNA designed to inhibit an oncomiR, such as miR-155, in lymphoma cell lines [59].
Application Note: Targeting miR-155 with clamp-G modified PNA (cGPNA) in Diffuse Large B-Cell Lymphoma. The cGPNA analog incorporates a specific "clamp-G" nucleobase that further enhances binding affinity to the target miRNA [59].
Materials:
- Cell Lines: U2932, OCI-Ly3 (Diffuse Large B-Cell Lymphoma lines).
- Test Articles: clamp-G modified PNA (cGPNA) anti-miR-155, scramble-sequence cGPNA control.
- Transfection Reagent: (e.g., Lipofectamine), if required.
- qRT-PCR Kit: For quantification of miR-155 and downstream target mRNAs (e.g., SHIP1, FOXO3a).
- Western Blot Equipment: For protein-level validation of target genes.
- In Vivo Components: Immunocompromised mice (e.g., NOD/SCID), Matrigel.
Methodology:
- Cell Culture: Maintain lymphoma cell lines in recommended media under standard conditions (37°C, 5% CO2).
- GPNA Treatment:
- Seed cells in 6-well plates.
- Treat cells with the anti-miR-155 cGPNA (0.5 - 10 µM range) or scramble control. Given the enhanced uptake of GPNA, transfection can often be performed without reagents ("gymnosis") or with standard transfection reagents to boost efficiency [58].
- Incubate for 24-72 hours.
- RNA Isolation and qRT-PCR Analysis:
- Harvest cells and extract total RNA.
- Perform reverse transcription for mature miR-155 using a stem-loop specific RT primer.
- Run qPCR using specific assays for miR-155 and its target mRNAs (e.g., SHIP1).
- Expected Outcome: Dose-dependent significant downregulation of miR-155 and concomitant upregulation of target mRNAs with the active cGPNA, but not with the scramble control [59].
- Functional Validation (In Vivo):
- Establish U2932 cell-derived xenografts in mice.
- Once tumors are palpable, administer anti-miR-155 cGPNA or control systemically (e.g., intravenous or intraperitoneal injection) multiple times per week.
- Monitor tumor volume and mouse survival.
- Expected Outcome: cGPNA treatment should result in significant reduction in tumor growth and improved survival compared to the control group [59].
Backbone Modification Strategies Beyond GPNA
The pursuit of optimized PNA properties has led to a diverse array of backbone modification strategies. The primary goals are to enhance solubility, improve binding affinity and specificity, introduce chirality for preorganization, and facilitate cellular delivery [57] [1]. The main strategies include:
- Introduction of Chirality: Incorporating chiral centers, typically at the α, β, or γ positions of the backbone, to preorganize the PNA into a right-handed helix, favoring binding to natural nucleic acids [1]. Examples include PNAs derived from D-lysine or other chiral amino acids.
- Cationic Modifications: Adding positively charged groups to improve water solubility and interaction with the negatively charged phosphates of nucleic acids and cell membranes. GPNA is a prime example, but other modifications like aminomethylene PNA (am-PNA) have also shown promise [58].
- Conformational Constraint: Introducing cyclic structures, such as cyclopentyl or cyclohexyl rings, to reduce the conformational entropy cost upon binding, thereby increasing duplex stability [1].
Table 2: Key Backbone Modification Strategies and Their Impact
| Modification Type | Example(s) | Key Structural Change | Primary Impact |
|---|---|---|---|
| Cationic (α-position) | α-GPNA, α-am-PNA | Guanidine/amino group at α-carbon | Enhanced cellular uptake; modulated binding affinity |
| Cationic (γ-position) | γ-GPNA, γ-am-PNA | Guanidine/amino group at γ-carbon | Superior binding affinity & cellular uptake due to backbone preorganization |
| Chiral Centers | PNA from D-lysine | Chirality at α or γ position | Preorganizes backbone into right-handed helix, improving binding |
| Conformational Constraint | Cyclohexyl PNA | Incorporation of cyclic structures | Reduces flexibility, enhances thermal stability of duplexes |
Protocol: Solid-Phase Synthesis of Backbone-Modified PNA
This protocol describes the general solid-phase synthesis (SPS) procedure for producing backbone-modified PNA oligomers, which is analogous to standard peptide synthesis [1].
Materials:
- Solid Support: Merrifield resin or other appropriate resin.
- Protected PNA Monomers: Boc (tert-butyloxycarbonyl) or Fmoc (fluorenylmethyloxycarbonyl) protected monomers, including any specially synthesized backbone-modified monomers (e.g., GPNA monomers).
- Coupling Reagents: such as HBTU/HOBt or PyBOP, with a base like DIPEA.
- Deprotection Reagents:
- For Boc strategy: Trifluoroacetic Acid (TFA).
- For Fmoc strategy: Piperidine.
- Cleavage Reagent: 4-Trifluoromethyl salicylic acid (TFMSA) or TFA for cleaving the oligomer from the resin and removing permanent protecting groups.
- Purification & Analysis: Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) system, Matrix-Assisted Laser Desorption/Ionization Time-of-Flight (MALDI-TOF) Mass Spectrometry.
Methodology:
- Resin Loading: The C-terminus of the first PNA monomer is attached to the solid-phase resin. The N-terminal amine is protected with PG1 (e.g., Boc or Fmoc) [1].
- Deprotection: The PG1 protecting group is removed.
- Boc Strategy: Treat with TFA.
- Fmoc Strategy: Treat with piperidine.
- Coupling: The next protected PNA monomer is activated using coupling reagents (e.g., HBTU/HOBt/DIPEA) and added to the reaction vessel to couple to the free amine on the resin-bound growing chain.
- Repetition: Steps 2 and 3 are repeated until the full-length sequence is assembled.
- Cleavage and Global Deprotection: The synthesized PNA oligomer is cleaved from the resin, and all remaining protecting groups (PG2 on nucleobases) are removed using a strong acid cocktail like TFMSA/TFA or TFA with appropriate scavengers [1].
- Purification and Characterization: The crude PNA is purified by RP-HPLC. The identity and purity of the final product are confirmed by HRMS, typically MALDI-TOF [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for PNA Research and Development
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Custom PNA Monomers | Building blocks for SPS of modified PNAs | GPNA monomers, chiral monomers (D-lysine derived), cyclopentyl monomers |
| Solid-Phase Resin | Support for SPS | Merrifield Resin, Wang Resin |
| Cell-Penetrating Peptides (CPPs) | Conjugation to PNA to enhance delivery | Octaarginine (R8), Penetratin, TAT peptide [58] |
| Cationic Nanoparticles | Non-covalent delivery vehicle for PNA | Cationic shell-cross-linked knedel-like nanoparticles (cSCKs) [58] |
| Lipid Nanoparticles (LNPs) | Advanced delivery system for in vivo applications | Formulations for siRNA/mRNA delivery can be adapted for PNA/ODN hybrids [60] [58] |
| qRT-PCR Assays | Quantifying miRNA/mRNA expression after PNA treatment | TaqMan assays for specific miRNAs (e.g., hsa-miR-155) and mRNAs |
| Cell Viability Assays | Assessing cytotoxicity of PNA oligomers | MTT, MTS, CellTiter-Glo assays |
Visualization of PNA Mechanisms and Workflows
Enhanced RNA Binding with GPNA
Diagram 1: GPNA enhances RNA binding affinity by introducing cationic groups that reduce electrostatic repulsion and improve sequence-specific binding compared to unmodified PNA [58].
Experimental Workflow for GPNA Evaluation
Diagram 2: A standard workflow for developing and evaluating modified PNAs like GPNA, from synthesis to in vivo validation [59] [58].
Addressing Scalability and Cost-Effectiveness in PNA Synthesis
Peptide Nucleic Acids (PNAs) are synthetic molecules with a backbone of N-(2-aminoethyl)glycine that demonstrates higher binding affinity and stability than natural nucleic acids [1]. Their unique properties make them invaluable for applications in therapeutics, molecular diagnostics, and genetic research [61] [1]. The global PNA market, valued at approximately USD 500 million in 2023, is projected to reach USD 1.2 billion by 2032, growing at a CAGR of 10.2% [61]. This rapid growth intensifies the need to address the historically high cost and complex scalability of PNA synthesis, which remain significant barriers to broader adoption [62] [63].
Traditional solid-phase synthesis, developed in the 1980s, builds DNA or RNA strands one nucleotide at a time through cyclical steps of deprotection, coupling, oxidation, and capping [62]. Even small inefficiencies in these steps accumulate into significant impurities, lowering quality and compromising safety [62]. Furthermore, this method consumes large amounts of solvents, such as acetonitrile, creating substantial sustainability concerns and waste management challenges for commercial-scale production [62].
Table 1: Global PNA Market Outlook and Key Challenges
| Aspect | Current Status/Forecast | Primary Challenge |
|---|---|---|
| Market Size (2023) | ~USD 500 Million [61] | High synthesis cost limits adoption, especially in cost-sensitive settings [64] [65]. |
| Projected Market Size (2032) | ~USD 1.2 Billion [61] | Scaling research processes to manufacturing scale is a persistent challenge [66]. |
| Growth Rate (CAGR) | 10.2% (2025-2032) [61] | Traditional solid-phase synthesis generates significant impurities and solvent waste [62]. |
| Key Scalability Issue | Scaling research processes to manufacturing [66] | Limited in vivo delivery efficiency requires complex conjugate systems [14]. |
Recent Innovations in Synthesis Chemistry
Advanced Protecting Groups and Solid-Phase Workflows
A key innovation for improving PNA synthesis is the development of novel protecting groups. Described in patent WO2018011067A2, these new protecting groups are engineered to detach more cleanly and efficiently during the synthesis cycle than traditional ones [62]. This cleaner deprotection reduces the generation of side products and fragmented sequences, thereby increasing the final purity and yield of the full-length PNA product [62]. Even marginal improvements in step-wise efficiency compound significantly over dozens of synthesis cycles, making this a critical area of development [62].
The same patent also outlines optimizations to the solid-phase workflow itself, aiming to improve coupling efficiency and reduce reagent waste [62]. These improvements make the entire synthetic process more reliable and cost-effective, which is crucial for scaling up production to meet clinical and commercial demands [62].
Exploration of Enzymatic and Hybrid Synthesis
Beyond refining chemical synthesis, the industry is actively exploring enzymatic synthesis as a more sustainable alternative. Enzymatic approaches use biological catalysts rather than harsh chemicals, potentially offering a solvent-free production route that would drastically reduce environmental waste [62]. While chemical synthesis remains the current gold standard, enzymatic techniques are gaining traction. Future production will likely combine the precision and scalability of chemical methods with the eco-friendliness of enzymatic approaches in hybrid strategies [62].
A Protocol for Efficient PNA Synthesis and Conjugation
This protocol provides a detailed methodology for the solid-phase synthesis of PNA and its subsequent non-covalent complexation with cell-penetrating peptides (CPPs), based on recently published research [14].
Materials and Reagents
Table 2: Key Research Reagent Solutions for PNA Synthesis and Conjugation
| Reagent / Material | Function / Role | Example / Specification |
|---|---|---|
| Fmoc/Bhoc Protected PNA Monomers | Building blocks for PNA chain assembly on a solid support. | Sourced from specialized manufacturers (e.g., Panagene) [14]. |
| Fmoc-XAL-PEG-PS Resin | Solid support matrix for synthesis. | Provides a scaffold for sequential monomer addition [14]. |
| Cell-Penetrating Peptides (CPPs) | Enhances cellular delivery of synthesized PNA. | TP10, Tat, TD2.2; include a C-terminal NLS [14]. |
| Trifluoroacetic Acid (TFA) | Deprotection and cleavage reagent. | Removes protecting groups and cleaves the final PNA from the resin [14]. |
| Reverse-Phase HPLC (RP-HPLC) | Purification of crude PNA oligomers. | Critical for separating full-length product from failure sequences [62] [1]. |
Step-by-Step Experimental Procedure
Step 1: Solid-Phase PNA Synthesis
- Resin Loading: Begin by loading Fmoc-XAL-PEG-PS resin onto an automated synthesizer [14].
- Chain Elongation: Conduct synthesis using Fmoc/Bhoc-protected PNA monomer chemistry. The cycle involves:
- Deprotection: Remove the Fmoc group from the resin-bound monomer using piperidine or TFA to expose the reactive amine [1] [14].
- Coupling: Activate the next Fmoc-protected PNA monomer and couple it to the deprotected amine on the growing chain [14].
- Capping: Acetylate any unreacted chains to prevent deletion sequences [62].
- Repetition: Repeat the deprotection and coupling cycle sequentially until the full-length PNA sequence is assembled.
Step 2: Cleavage, Deprotection, and Purification
- Cleavage from Resin: Cleave the crude PNA oligomer from the solid support and remove all protecting groups using a strong acid cocktail, typically TFA or TFMSA [1] [14].
- Purification: Purify the crude product using Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) to isolate the full-length PNA from shorter failure sequences and impurities [1].
- Analysis: Verify the identity and purity of the final product using analytical HPLC and characterize it by electrospray ionization mass spectrometry (ESI-MS) [14].
Step 3: Complexation with Cell-Penetrating Peptides (CPPs)
- Prepare Solutions: Prepare separate aqueous stock solutions of the synthesized PNA and the selected CPP (e.g., TP10, Tat, TD2.2) [14].
- Form Complexes: Mix the PNA and CPP solutions at a pre-optimized molar ratio to form stable, non-covalent complexes. Research indicates a ratio of 1:10 (PNA:CPP) is often effective, with TP10 showing superior delivery efficiency [14].
- Incubate: Incubate the mixture for 15-30 minutes at room temperature to allow for complete complex formation before use in cellular assays.
Diagram 1: PNA synthesis, purification, and application workflow.
Enhancing Cellular Delivery for Therapeutic Efficacy
A major hurdle for PNA therapeutics is inefficient cellular uptake due to their neutral backbone and large molecular size [14]. To overcome this, conjugation with Cell-Penetrating Peptides (CPPs) is a widely adopted strategy [67] [14]. CPPs are short, positively charged peptides that facilitate the transport of cargo across cell membranes.
Recent studies have optimized non-covalent complexes of PNA with CPPs like TP10, Tat, and TD2.2 [14]. Among these, TP10 demonstrated superior effectiveness in delivering PNAs to their intracellular targets [14]. Furthermore, incorporating a Nuclear Localization Signal (NLS) at the C-terminus of the PNA sequence actively directs the molecule to the cell nucleus after entry, which is essential for antigene or antisense applications that target DNA or nuclear RNA [14].
Diagram 2: Mechanism of CPP and NLS-enhanced PNA delivery.
Innovations in protecting group chemistry and solid-phase workflows are directly addressing the long-standing challenges of purity, cost, and scalability in PNA synthesis [62]. Concurrently, advanced delivery strategies using CPPs are unlocking the therapeutic potential of PNA by ensuring efficient intracellular delivery [14]. The ongoing transition from research-scale to commercially viable GMP manufacturing hinges on the continued adoption of these advanced synthesis and purification methods. As the industry moves forward, the integration of greener chemistry, hybrid synthesis approaches, and sophisticated delivery systems will be paramount in making PNA-based therapeutics and diagnostics more accessible and effective.
PNA in the Competitive Landscape: Validation, Market Analysis, and Comparative Advantages
The advent of oligonucleotide-based therapeutics has revolutionized our approach to treating genetic diseases and infections, offering a platform to target previously "undruggable" pathways. These therapies use engineered sequences of nucleotides to selectively modulate gene expression at the post-transcriptional level [68]. Among these, Peptide Nucleic Acid (PNA) stands out for its unique synthetic backbone, providing exceptional binding affinity and stability. This application note provides a structured, comparative analysis of PNA against other prominent oligonucleotide technologies—including small interfering RNA (siRNA), Phosphorodiamidate Morpholino Oligomers (PMOs), and antisense oligonucleotides (ASOs)—framed within the context of therapeutics and diagnostics research. We focus on their molecular mechanisms, therapeutic potential, and current limitations, supported by quantitative data and detailed experimental protocols.
Molecular Mechanisms and Properties
Understanding the fundamental structure and mechanism of each oligonucleotide type is crucial for selecting the appropriate tool for a specific research or therapeutic application.
Peptide Nucleic Acid (PNA): PNA is an artificially synthesized polymer featuring a backbone of N-(2-aminoethyl)glycine instead of the sugar-phosphate backbone found in DNA and RNA [11] [14]. This neutral, achiral structure results in the absence of electrostatic repulsion when binding to complementary DNA or RNA strands. This key characteristic confers higher binding affinity and specificity compared to natural nucleic acids, with a melting temperature (Tm) typically 1°C higher per base pair than a equivalent DNA/DNA duplex [11]. PNA operates primarily through steric blockade via antisense mechanisms. It can bind to DNA or RNA to form stable duplexes, triplexes, or even duplex-invasion complexes, thereby inhibiting transcription or translation [14]. Its peptide-like backbone makes it resistant to degradation by both nucleases and proteases, ensuring high stability in biological environments [11].
Small Interfering RNA (siRNA): siRNA is a class of double-stranded RNA molecules, typically 21-23 nucleotides in length, that operates through the endogenous RNA interference (RNAi) pathway [69]. The process begins when the siRNA duplex is loaded into the RNA-induced silencing complex (RISC). The complex is unwound, and the guide strand binds to its complementary target messenger RNA (mRNA). The Argonaute-2 (Ago-2) protein within RISC then cleaves the target mRNA, leading to its degradation and subsequent gene silencing [69]. This mechanism is highly specific and catalytic, as a single RISC complex can degrade multiple mRNA molecules.
Phosphorodiamidate Morpholino Oligomer (PMO): PMOs are a type of antisense oligonucleotide belonging to the third generation of ASO chemistries [70]. They feature a backbone where the ribose sugar is replaced by a morpholino ring, and the phosphodiester linkage is replaced by a phosphorodiamidate group [70] [68]. This uncharged structure makes PMOs highly resistant to nucleases. Their primary mechanism of action is steric hindrance [68]. They bind to target RNA sequences and block access to cellular machinery without inducing degradation. This makes them particularly effective for modulating pre-mRNA splicing—for example, by forcing the exclusion (exon skipping) or inclusion of specific exons to restore protein function.
Antisense Oligonucleotides (ASOs) - Gapmer: Gapmer ASOs are chimeric molecules designed to recruit cellular enzymes for target degradation. They contain a central region of DNA nucleotides ("the gap") flanked by modified RNA nucleotides (e.g., 2'-O-Methoxyethyl, Locked Nucleic Acid) [70] [68]. After binding to the target RNA via Watson-Crick base pairing, the DNA gap recruits RNase H1, which cleaves the RNA strand of the RNA-DNA heteroduplex, leading to the degradation of the target mRNA [70].
Table 1: Comparative Properties of Oligonucleotide Therapies
| Property | PNA | siRNA | PMO | Gapmer ASO |
|---|---|---|---|---|
| Chemical Backbone | N-(2-aminoethyl)glycine | Sugar-phosphate (can be modified) | Morpholino & phosphorodiamidate | Sugar-phosphate with various modifications |
| Charge | Neutral | Negatively charged | Neutral | Negatively charged (often phosphorothioated) |
| Primary Mechanism | Steric Blockade (Transcription/Translation) | RISC-mediated mRNA Degradation | Steric Blockade (e.g., Splicing Modulation) | RNase H1-mediated mRNA Degradation |
| Typical Length | 13-20 bases [11] | 21-23 bp [69] | 18-30 bases [68] | 18-30 bases [68] |
| Binding Affinity | Very High (Tm ~ +1°C/bp vs DNA) [11] | High | Moderate | High (depends on flanking chemistry) |
| Nuclease Resistance | Excellent [11] | Good (requires modification) | Excellent [70] | Good (requires modification) |
| Key Advantage | High affinity & stability; gene editing potential | Catalytic, potent silencing | Excellent safety & splicing modulation | Versatile (degradation & steric block) |
The following diagram illustrates the core mechanistic pathways for these oligonucleotide therapies.
Diagram: Oligonucleotide Core Mechanisms. Pathways diverge into steric blockade (PNA, PMO, Steric-Block ASO) and mRNA degradation (siRNA, Gapmer ASO).
Quantitative Data Comparison
A head-to-head comparison of key performance metrics is essential for rational decision-making.
Table 2: Performance and Clinical Translation Metrics
| Metric | PNA | siRNA | PMO | Gapmer ASO |
|---|---|---|---|---|
| Gene Silencing Efficiency | Moderate-High (context dependent) [71] | Very High (catalytic) [69] | Moderate-High (for splicing) [68] | High [70] |
| Cellular Uptake (No Carrier) | Poor [14] | Poor [72] | Poor | Moderate (PS-backbone) |
| Off-Target Effect Risk | Low (high specificity) [11] | Moderate (seed region homology) [69] [73] | Low (steric block only) | Moderate (hybridization-dependent) [73] |
| Stability in Serum | Excellent [11] | Good (with modification) [72] | Excellent [70] | Good (with modification) [70] |
| FDA-Approved Drugs | 0 (as of 2025) | 6 (e.g., Patisiran, Givosiran) [68] | 2 (e.g., Eteplirsen) [68] | 11 (e.g., Nusinersen) [68] |
| Therapeutic Areas (Examples) | Oncology, Metabolic Diseases (preclinical) [71] [14] | Amyloidosis, Porphyria, Hypercholesterolemia [68] [69] | Duchenne Muscular Dystrophy [68] | Spinal Muscular Atrophy, Huntington's disease [68] |
Detailed Experimental Protocols
Protocol: Evaluating PNA-Mediated Gene Silencing Using CPP Delivery
This protocol details a method to assess the efficacy of PNA molecules designed to silence a target gene (e.g., GAPDH or PCSK9) upon delivery via cell-penetrating peptides (CPPs) [71] [14].
I. PNA-CPP Complex Preparation and Transfection
- PNA Design: Design and synthesize a PNA oligomer (e.g., 13-18 mer) complementary to the translation start site or an early exon of the target mRNA. Incorporate a nuclear localization signal (NLS; e.g.,
Pro-Lys-Lys-Lys-Arg-Lys-Val) at the C-terminus for nuclear targets [14]. - CPP Selection: Select CPPs such as TP10, Tat, or TD2.2 based on reported high efficiency [14].
- Complex Formation: Prepare a non-covalent complex by mixing PNA and CPP at optimized molar ratios (determined empirically, e.g., 1:5 to 1:20 PNA:CPP) in a serum-free buffer. Incubate for 15-30 minutes at room temperature to allow complex formation [14].
- Cell Seeding: Seed adherent cells (e.g., HeLa, HepG2) in a 24-well plate at a density of 5 x 10^4 cells/well and culture until ~70% confluency.
- Transfection: Replace the medium with fresh, serum-containing medium. Add the pre-formed PNA-CPP complexes to the cells. Incubate for 4-24 hours at 37°C [14].
- Post-Transfection: Remove the transfection medium, wash cells with PBS, and add fresh complete medium. Analyze after 24-72 hours.
II. Efficacy Assessment via Western Blot
- Cell Lysis: Harvest cells 48-72 hours post-transfection. Lyse cells using RIPA buffer supplemented with protease inhibitors.
- Protein Quantification: Determine protein concentration using a BCA assay.
- Gel Electrophoresis and Transfer: Separate equal amounts of protein (e.g., 20-30 µg) by SDS-PAGE and transfer to a PVDF membrane.
- Immunoblotting: Block the membrane with 5% non-fat milk. Incubate with a primary antibody against the target protein (e.g., anti-GAPDH) overnight at 4°C, followed by an HRP-conjugated secondary antibody. Detect bands using chemiluminescence.
- Analysis: Quantify band intensities using imaging software and normalize to a housekeeping protein (e.g., β-Actin) to determine the percentage of target gene silencing [71].
Protocol: siRNA Transfection for Gene Knockdown
This standard protocol outlines siRNA-mediated gene silencing using lipid nanoparticles (LNPs), a common delivery strategy [69] [72].
I. siRNA Transfection
- siRNA Design: Use validated siRNA sequences with full complementarity to the target mRNA. Check for minimal seed region homology to minimize off-target effects [69].
- Complex Formation: Dilute siRNA (e.g., 5-50 nM final concentration) in a serum-free medium. In a separate tube, dilute LNP transfection reagent per manufacturer's instructions. Combine the diluted siRNA and LNP reagent, mix gently, and incubate for 15-20 minutes at room temperature to form complexes.
- Cell Transfection: Seed cells as in Protocol 4.1. Add the siRNA-LNP complexes dropwise to the cells. Swirl the plate gently to ensure even distribution.
- Incubation and Analysis: Incubate for 4-6 hours before replacing with fresh complete medium. Assay for mRNA knockdown (via qRT-PCR) or protein knockdown (via Western blot) 24-72 hours post-transfection.
II. qRT-PCR for mRNA Knockdown Validation
- RNA Extraction: Extract total RNA from transfected cells using a commercial kit (e.g., TRIzol).
- cDNA Synthesis: Synthesize cDNA from 1 µg of total RNA using a reverse transcription kit with random hexamers or oligo-dT primers.
- Quantitative PCR: Perform qPCR using gene-specific primers and a SYBR Green master mix. Use the following cycling conditions: initial denaturation at 95°C for 3 min; 40 cycles of 95°C for 10 sec and 60°C for 30 sec.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method, normalizing to a housekeeping gene (e.g., GAPDH, β-Actin).
The workflow for these core experiments is summarized below.
Diagram: PNA vs. siRNA Experimental Workflow. Key differences lie in oligo design, delivery complex, and readout assay.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of the protocols requires key reagents, each with a critical function.
Table 3: Key Reagents for Oligonucleotide Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| PNA Oligomers (e.g., Fluo-PCSK9-PPT-EX1-Ahx-NLS) [14] | Core molecule for antisense gene silencing; fluorescein label enables tracking. | Requires custom synthesis; sequence and NLS are critical for efficacy and localization. |
| Cell-Penetrating Peptides (CPPs) (e.g., TP10, Tat, TD2.2) [14] | Enhances cellular delivery of PNA and other cargoes via non-covalent complexation. | Efficiency varies (TP10 > Tat ~ TD2.2); molar ratio optimization is essential. |
| siRNA Duplexes (21-23 nt, validated) [69] [72] | Triggers RNAi pathway for specific mRNA degradation. | Requires rigorous off-target checks (e.g., BLAST); chemical modifications enhance stability. |
| Lipid Nanoparticles (LNP) | A leading delivery system for siRNA, protecting it and promoting cellular uptake. | Formulation parameters (lipid ratio, size) critically impact efficacy and toxicity. |
| Phosphorothioate-Modified ASOs | First-generation ASO backbone modification improving nuclease resistance and pharmacokinetics. | Can increase protein binding and potential for off-target toxicities [70] [73]. |
| Fmoc/Bhoc Protected PNA Monomers | Building blocks for the solid-phase synthesis of custom PNA oligomers. | Essential for in-house PNA synthesis; requires expertise in solid-phase chemistry [14]. |
This head-to-head analysis underscores that no single oligonucleotide technology is universally superior. The choice between PNA, siRNA, PMO, and ASOs is dictated by the specific research or therapeutic goal. PNA's standout features are its superior binding affinity and biostability, making it a powerful tool for diagnostic applications and antisense-based therapeutic modulation, though its delivery remains a key research focus. siRNA offers a potent, catalytic mechanism for knocking down mRNA in the cytoplasm and has a strong track record of clinical translation. PMOs provide an excellent safety profile for splicing correction applications, as evidenced by approved drugs for DMD. Finally, the versatile ASO platform can be engineered for both degradation and steric blockade, offering broad applicability.
The future of oligonucleotide therapeutics lies in overcoming persistent challenges, particularly in delivery and off-target effects. For PNA, advances in CPP technology and novel nanocarriers, such as the ferritin nanocage system [71], are paving the way for more efficient intracellular delivery. For siRNA and ASOs, continued refinement of chemical modifications and delivery platforms (e.g., GalNAc-conjugates for hepatocyte targeting) is enhancing specificity and reducing toxicity [70] [68] [73]. As these technologies mature, PNA is poised to move from a primarily research-focused tool to a promising contender in the next generation of precision nucleic acid therapeutics and diagnostics.
The global Peptide Nucleic Acid (PNA) market is demonstrating robust and consistent growth, fueled by increasing adoption in molecular diagnostics, therapeutics, and genetic research. Multiple market analyses confirm a positive expansion trajectory through the next decade, with varying projections reflecting different methodological approaches and segment focuses. The market's growth is primarily driven by PNA's superior properties, including high binding affinity, resistance to enzymatic degradation, and exceptional stability across varied pH and temperature ranges, making it invaluable for advanced research and clinical applications [4] [35].
Table 1: Global PNA Market Size and Growth Projections
| Report Source | Base Year/Value | Projection Year/Value | Compound Annual Growth Rate (CAGR) |
|---|---|---|---|
| Market Report Analytics [74] | $980 million (2025) | Projected through 2033 | 22.0% |
| Infinity Market Research [75] | $383 million (2025) | $879 million (2031) | 14.8% |
| DataIntelo [61] | ~$500 million (2023) | $1.2 billion (2032) | 10.2% |
The PNA monomers market, which supplies the fundamental building blocks for PNA synthesis, is also experiencing significant growth. It is projected to reach an estimated $450 million in 2025, advancing at a CAGR of approximately 12.5% through 2033 [65]. This parallel growth in the monomer market underscores the expanding production and research activities in the PNA sector.
Key Market Drivers and Application Segments
The expansion of the PNA market is underpinned by several key drivers and is segmented into distinct application areas and product types.
Primary Market Drivers
- Advancements in Personalized Medicine: The shift towards personalized medicine is increasing the demand for highly specific genetic tools, a role PNA is uniquely suited to fill due to its precision and reliability [61].
- Rising Prevalence of Genetic Disorders: The growing incidence of genetic and chronic diseases is propelling the demand for advanced molecular diagnostics and targeted therapeutics where PNA plays a critical role [74] [61].
- Technological Innovation in Synthesis: Ongoing improvements in PNA synthesis and purification technologies are enhancing production efficiency, reducing costs, and making PNA more accessible [65].
- Integration with Gene Editing Tools: PNA's use as an auxiliary material in gene-editing technologies like CRISPR-Cas9 to improve efficiency and specificity is creating new application pathways [75].
Market Segmentation
Table 2: PNA Market Analysis by Segment
| Segmentation Type | Key Categories | Dominant Segment/Ranking |
|---|---|---|
| By Application | Gene Probes, Drug Development, Microarrays & Biosensors, Others [74] [75] | Drug Development is the dominant and fastest-growing segment, driven by therapeutic potential [74] [65]. |
| By Product Type | Labeled PNAs, Unlabeled PNAs [74] [75] | Fmoc PNA Monomers are the most widely used type due to their efficient synthesis protocols [65]. |
| By End-User | Pharmaceutical & Biotechnology Companies, Academic & Research Institutes, Diagnostic Laboratories [61] | Pharmaceutical and biotechnology companies represent a significant segment due to high investment in drug discovery [61]. |
Regional Landscape and Industry Players
Geographic Market Analysis
North America currently holds the dominant position in the global PNA market, a leadership attributed to its robust healthcare infrastructure, significant investment in research and development, and the strong presence of major biopharmaceutical companies [74] [61]. The United States is the primary contributor within this region. However, the Asia Pacific region is anticipated to witness the highest growth rate in the coming years, fueled by increasing healthcare expenditure, a growing biotechnology sector, and supportive government initiatives [61].
Key Industry Players
The competitive landscape of the PNA market features a diverse mix of companies specializing in PNA synthesis, reagent supply, and technology development. Key players include:
- SBS Genetech [75]
- HLB panagene [74] [75]
- LGC Biosearch Technologies [74] [75]
- PNA BIO INC [74] [75]
- Bio-Synthesis Inc [74] [75]
- DESTINA Genomics [74] [75]
- Creative Peptides [74] [75]
- BOC Sciences [75]
These companies are actively engaged in expanding their product portfolios and technological capabilities to capitalize on emerging opportunities in the PNA space. The level of mergers and acquisitions in the sector is moderate, often characterized by larger chemical or life science suppliers acquiring specialized PNA technology platforms [74] [65].
Experimental Protocol: PNA-Based Microbial Pathogen Identification and Antibiotic Resistance Detection
Background and Principle
This protocol details a Fluorescent In Situ Hybridization (FISH)-type method for the highly specific and sensitive identification of microbial pathogens and simultaneous detection of antibiotic resistance markers, such as discriminating between methicillin-sensitive (MSSA) and methicillin-resistant Staphylococcus aureus (MRSA) [76]. The technique synergizes the unique properties of bis-PNA "openers" with Rolling Circle Amplification (RCA) to achieve exceptional specificity and signal enhancement. Bis-PNA molecules invade double-stranded DNA at predetermined homopurine-homopyrimidine tracts, displacing one DNA strand and creating a single-stranded region for probe binding [76]. A DNA oligonucleotide probe then circularizes upon hybridization to this accessible site, and RCA generates a long, repetitive DNA product that is visualized with fluorescent decorator probes.
Materials and Reagents
- Target Bacterial Genomic DNA: Purified DNA from bacterial samples (e.g., S. aureus strains).
- bis-PNA Openers: Two nested bis-PNA molecules designed to bind to short, closely spaced homopurine sequences on the target genomic DNA (e.g., for S. aureus species identification and mecA gene detection) [76].
- Padlock Probe: A linear, single-stranded DNA oligonucleotide with sequences at its 5' and 3' ends complementary to the target site exposed by the PNA openers. The internal segment should contain a generic primer-binding site and a tag sequence for fluorescent detection [76].
- DNA Ligase: T4 DNA ligase or similar, for catalyzing the circularization of the padlock probe upon perfect hybridization.
- Phi29 DNA Polymerase: For the RCA reaction, due to its strong strand-displacement and processive synthesis capabilities.
- Fluorescent Decorator Probes: Short, fluorophore-labeled oligonucleotides complementary to the tag sequence repeated within the RCA product.
- Hybridization and Wash Buffers
- Fluorescence Microscope: For visualization of the localized fluorescent signals.
Step-by-Step Procedure
- Sample Preparation and Denaturation: Extract genomic DNA from the bacterial sample and prepare it in a suitable hybridization buffer.
- PNA Invasion and Target Site Opening: Add the specific bis-PNA openers to the DNA sample. Incubate to allow the PNA molecules to invade the double-stranded DNA and form a PD-loop structure, exposing the single-stranded target sequence for the padlock probe.
- Padlock Probe Hybridization and Ligation: Introduce the padlock probe to the reaction. The ends of the probe hybridize flanking the target sequence. Upon correct hybridization, the DNA ligase seals the nick, forming a circular probe that is topologically linked to the target DNA.
- Rolling Circle Amplification (RCA): Add phi29 DNA polymerase and dNTPs to the reaction. The circularized padlock probe serves as a template for RCA, generating a long single-stranded DNA concatemer containing hundreds of repeats complementary to the circle.
- Fluorescent Labeling: Hybridize fluorescently labeled decorator probes to the tag sequence repeats within the RCA product.
- Signal Detection and Analysis: Wash the sample to remove unbound probes and visualize under a fluorescence microscope. The presence of a localized fluorescent signal indicates a positive detection of the target sequence. Multiplexing for different targets (e.g., species identifier and resistance marker) can be achieved using padlock probes with different decorator tag sequences and corresponding fluorophores.
Visualization of Experimental Workflow
Diagram 1: PNA-based Detection Workflow.
Research Reagent Solutions Toolkit
Table 3: Essential Reagents for PNA-Based Research Experiments
| Research Reagent | Function/Application | Key Characteristics |
|---|---|---|
| PNA Oligomers [74] [75] | Synthetic nucleic acid analogs used as antisense agents, gene probes, and for target sequence binding in diagnostic assays. | Neutral pseudopeptide backbone, high biostability, strong affinity for complementary DNA/RNA, nuclease and protease resistance [4] [35]. |
| PNA Monomers (Fmoc/Boc) [65] | Building blocks for the custom solid-phase synthesis of PNA oligomers. | Available with Fmoc (9-fluorenylmethyloxycarbonyl) or Boc (tert-butyloxycarbonyl) protecting groups for controlled chain elongation [65]. |
| Cell-Penetrating Peptides (CPPs) [4] | Conjugated to PNA to facilitate cellular uptake and intracellular delivery, overcoming the inherent poor permeability of PNA. | Often rich in arginine residues; enhances bioavailability and biological activity of PNA in vitro and in vivo [4]. |
| Bis-PNA "Openers" [76] | Specialized PNA molecules for invading double-stranded DNA to enable detection or manipulation, as used in the protocol above. | Two PNA oligomers connected by a flexible linker; form highly stable P-loop structures with dsDNA via strand invasion [76]. |
| Padlock Probes [76] | Linear DNA oligonucleotides used in conjunction with bis-PNA for highly specific detection; circularize upon ligation. | Enable single-nucleotide discrimination; become template for RCA, providing significant signal amplification [76]. |
PNA Therapeutic Mechanisms and Applications
PNAs exert their therapeutic effects primarily through antigene and antisense mechanisms, offering a versatile platform for genetic intervention.
Mechanisms of Action
- Antigene Strategy: Pyrimidine-rich PNAs can bind to specific complementary sequences in double-stranded DNA via strand invasion, forming a stable PNA-DNA-PNA triplex structure. This can physically block the binding of transcription factors or RNA polymerase, thereby inhibiting gene transcription at the genomic level [4].
- Antisense Strategy: PNAs can hybridize with high affinity to complementary messenger RNA (mRNA) sequences in the cytoplasm. This binding can sterically block the translation of the mRNA into protein by preventing ribosome assembly or progression. It can also be used to modulate pre-mRNA splicing by blocking splice sites [4] [35].
Visualization of Therapeutic Mechanisms
Diagram 2: PNA Therapeutic Mechanisms.
Table 4: Examples of PNA Applications in Gene Therapy Research
| PNA Type / Target | Model / Disorder | Observed Effect | Reference |
|---|---|---|---|
| Antigene PNA (RAD51 gene) | Multiple Myeloma (MM) cell line & mouse model | Inhibition of RAD51 expression, a DNA repair protein. | [4] |
| Antisense PNA (miR-155) | Mouse model of Lymphoma | Inhibition of oncomiR-155, a microRNA involved in cancer progression. | [4] |
| γPNA & Donor DNA | β-thalassaemia mouse model | Correction of a intronic mutation in the β-globin gene via DNA repair. | [4] |
| Antisense PNA (LTR of HBV RNA) | Hepatitis B mouse model | Decline in Hepatitis B Virus (HBV) DNA levels. | [4] |
Regulatory Pathways and Commercialization Hurdles for PNA-Based Products
Peptide Nucleic Acid (PNA) represents a unique class of synthetic oligonucleotide analogues where the natural sugar-phosphate backbone is replaced by an uncharged, pseudopeptide backbone composed of N-(2-aminoethyl)glycine units [4] [54]. First invented by Peter E. Nielsen and colleagues in 1991, PNA maintains the nucleobases found in natural nucleic acids, allowing it to hybridize with complementary DNA and RNA sequences with exceptional affinity and specificity through Watson-Crick base pairing [54] [77]. This structural modification confers several advantageous properties, including resistance to enzymatic degradation by proteases and nucleases, higher biostability compared to natural nucleic acids, and strong hybridization capability independent of salt concentration [4] [77]. These characteristics make PNA a promising candidate for various biomedical applications, particularly as antisense and antigene agents for therapeutic gene modulation, as well as powerful tools in molecular diagnostics [4] [54].
The global nucleic acid therapeutics market has experienced significant growth, propelled by advancements in oligonucleotide-based technologies and the successful development of mRNA vaccines during the COVID-19 pandemic [78] [77]. Within this expanding landscape, PNA-based technologies offer distinctive opportunities for precise gene regulation, splicing modulation, and gene editing applications across various disease areas, including cancer, genetic disorders, and infectious diseases [4] [54]. However, the transition of PNA from a research tool to clinically approved products faces substantial regulatory and commercialization challenges that must be systematically addressed to realize its full therapeutic potential.
Global Regulatory Landscape for PNA-Based Products
Regional Regulatory Frameworks and Classification Challenges
The regulatory pathways for PNA-based products vary significantly across different global regions, creating a complex mosaic that developers must navigate. These frameworks are evolving as regulatory agencies adapt to advanced therapeutic products incorporating synthetic nucleic acid technologies [79] [80].
Table 1: Comparative Regulatory Approaches for Advanced Therapeutic Products Across Key Regions
| Region/Country | Regulatory Approach | Key Characteristics | Implications for PNA Developers |
|---|---|---|---|
| United States | Product-based, risk-weighted | Flexible approach focusing on product characteristics rather than production process; utilizes existing biologics and drug pathways | Case-by-case assessment possible; emphasis on final product safety and efficacy profile |
| European Union | Process-based | Historically classifies genome-edited organisms as GMOs; proposals for differentiation of products with limited, predefined genetic changes [80] | Higher regulatory burden; may require comprehensive safety assessment and labeling |
| Latin America | Mixed approaches, some with case-by-case assessment | Countries including Argentina, Brazil, and Chile assess whether final product contains new genetic combinations; classification as conventional if no foreign DNA present [79] [80] | Faster pathways for PNA products without integrated foreign DNA; more predictable for certain applications |
| Asia (China, India) | Flexible, product-oriented | China: 1-2 year approval timelines with safety assessment and labeling [80]; India: excludes SDN1/SDN2 products without foreign DNA from GMO classification [80] | Streamlined pathways for specific PNA applications; China requires comprehensive risk assessment |
| Africa (Kenya, Nigeria) | Adaptive, case-by-case | Emerging frameworks distinguishing conventional, intermediate, and transgenic products with proportional risk assessment [80] | Developing regulatory clarity; early consultation mechanisms provide predictability |
A fundamental challenge in PNA product classification stems from the distinction between process-based and product-based regulatory systems [80]. Process-based systems, historically prominent in the European Union, trigger regulatory oversight based on the use of recombinant DNA technology rather than the characteristics of the final product. In contrast, product-based systems, exemplified by Canada's "plants with novel traits" framework, assess organisms based on the final product's traits regardless of the development method [80]. This regulatory dichotomy creates significant challenges for PNA developers operating in global markets, as products may face dramatically different regulatory requirements depending on the jurisdiction.
Intellectual Property Considerations
Intellectual property represents a critical strategic battlefield for PNA-based products, with significant variations in protection mechanisms across regions [79]. Key considerations include:
Patent Linkage: Some jurisdictions, notably Mexico, implement strong patent linkage systems that prohibit regulatory approval for generic products if relevant patents remain in force [79]. This creates substantial hurdles for follow-on PNA products and necessitates careful IP landscape analysis before development initiation.
Data Exclusivity: Periods of data exclusivity protect clinical trial data submitted by innovator companies. The duration varies by region, with Colombia offering five-year protection while Argentina provides none, significantly impacting market entry strategies [79].
Bolar Exceptions: These provisions allow manufacturers to conduct research and development activities, including necessary regulatory studies, before patent expiration. Mexico recently strengthened its Bolar provision, permitting generic PNA development immediately after patent grant [79].
The Latin American market exemplifies these regional regulatory complexities, with countries like Brazil adjusting IP frameworks to prioritize public health and access over patent protection, effectively delinking patent status from regulatory approval [79]. This contrasts sharply with Mexico's stringent linkage system, requiring PNA developers to implement country-specific regulatory strategies that account for these substantial differences in IP protection and enforcement.
Commercialization Hurdles for PNA-Based Products
Technical and Manufacturing Challenges
The commercialization pathway for PNA-based products faces several significant technical hurdles that impact both development timelines and manufacturing scalability:
Synthesis Limitations: PNA synthesis employs solid-phase synthesis (SPS) methodology, analogous to peptide synthesis, but is typically limited to sequences of 15-25 bases due to chain aggregation and difficult couplings [77]. Purine-rich sequences, particularly those containing multiple guanine units, present additional challenges due to their poor solubility and tendency toward aggregation during synthesis [77].
Scalability Issues: Transitioning from laboratory-scale synthesis to commercial manufacturing requires addressing significant hurdles in purification and characterization. Longer PNA chains exhibit increasingly poor solubility, complicating large-scale production and quality control processes [77].
Chemical Modification Requirements: Most therapeutic PNA applications require specific chemical modifications to address inherent limitations. These modifications include γ-position alterations with mini-polyethyleneglycol (PEG) or guanidine groups to improve solubility and cellular uptake, adding complexity to manufacturing [77].
Table 2: Key Technical Challenges in PNA Development and Potential Mitigation Strategies
| Technical Challenge | Impact on Commercialization | Current Mitigation Approaches |
|---|---|---|
| Poor Cellular Uptake | Limited biological efficacy; requires higher doses | Conjugation with cell-penetrating peptides (CPPs); structural modifications (e.g., γ-mini-PEG) [4] [77] |
| Rapid Systemic Clearance | Short half-life; frequent dosing requirements | Nanoparticle formulations; conjugation with half-life extending moieties [4] |
| Endosomal Entrapment | Reduced target engagement; suboptimal efficacy | Co-treatment with endosomolytic agents; incorporation of endosomal escape domains [4] |
| Sequence Aggregation | Manufacturing challenges; variable quality | Use of low-loading resins; hydrophilic polyethylene-glycol-based resins [77] |
| Synthetic Complexity | High production costs; regulatory challenges | Improved protecting group strategies; optimized coupling reagents [77] |
Delivery Challenges and Formulation Strategies
Effective intracellular delivery represents one of the most significant barriers to PNA commercialization. While PNAs demonstrate excellent target affinity and specificity in vitro, their translation to in vivo applications is hampered by several delivery-related challenges:
Cellular Uptake Limitations: The neutral backbone and hydrophilic character of unmodified PNAs severely limit their ability to cross cell membranes, resulting in poor cellular uptake without delivery enhancers [4] [77]. Early-stage research solutions include electroporation and membrane permeabilization techniques, but these have limited therapeutic applicability.
Systemic Distribution and Pharmacokinetics: Unmodified PNAs exhibit rapid renal clearance, with half-lives of approximately 10-30 minutes in mice following intravenous administration [77]. This necessitates frequent dosing or continuous infusion for systemic applications, complicating treatment regimens.
Endosomal Entrapment: Even when internalized via endocytic pathways, PNA conjugates frequently remain trapped within endosomal compartments, unable to reach their intracellular targets in the cytoplasm or nucleus [4]. Co-treatment with endosome-disruptive agents such as chloroquine can enhance biological activity, but raises additional safety concerns for clinical applications.
To address these challenges, several formulation and conjugation strategies have been developed:
Cell-Penetrating Peptide Conjugates: Covalent attachment of CPPs, particularly those rich in arginine residues, represents the most extensively investigated delivery strategy for PNAs [4] [77]. These conjugates significantly improve cellular uptake, though endosomal release remains a limiting factor.
Structural Modifications: Backbone modifications at the γ-position, particularly with mini-PEG groups, improve both solubility and hybridization properties while maintaining favorable toxicity profiles [77].
Nanoparticle Formulations: PNA encapsulation within lipid or polymeric nanoparticles protects against degradation, improves pharmacokinetic profiles, and enhances tissue targeting [4].
Diagram 1: PNA Delivery Challenges and Strategic Solutions. This workflow illustrates the major barriers in PNA therapeutic delivery and the corresponding strategies being developed to overcome them.
Experimental Protocols for PNA Therapeutic Development
Protocol 1: Solid-Phase PNA Synthesis Using Fmoc/Bhoc Chemistry
Principle: This protocol describes the standard solid-phase synthesis of PNA oligomers using Fmoc (9-fluorenylmethoxycarbonyl) as a temporary protecting group and Bhoc (benzhydryloxycarbonyl) for permanent protection of nucleobase amino groups [77].
Materials and Equipment:
- Resin Support: TentaGel or ChemMatrix resin (low-loading, 0.1-0.2 mmol/g) to minimize aggregation [77]
- PNA Monomers: Fmoc-protected PNA monomers with Bhoc-protected nucleobases (A, G, C, T)
- Deprotection Solution: 20% piperidine in DMF
- Coupling Reagents: HATU (1-[Bis(dimethylamino)methylene]-1H-1,2,3-triazolo[4,5-b]pyridinium 3-oxid hexafluorophosphate) and DIPEA (N,N-Diisopropylethylamine) in NMP (N-methyl-2-pyrrolidone)
- Cleavage Cocktail: Trifluoroacetic acid (TFA) with appropriate scavengers
- Purification System: Reverse-phase HPLC with C18 column
- Characterization: Mass spectrometry (MALDI-TOF or ESI-MS)
Procedure:
- Resin Swelling: Suspend 100 mg of resin in 2 mL DMF for 30 minutes with gentle agitation
- Fmoc Deprotection: Treat with 2 mL of 20% piperidine in DMF for 5 minutes, repeat once, then wash with DMF (3 × 2 mL)
- Coupling Cycle:
- Prepare coupling solution: 4 equivalents PNA monomer, 3.9 equivalents HATU, and 8 equivalents DIPEA in NMP
- Add coupling solution to resin and agitate for 30-45 minutes at room temperature
- Wash with DMF (3 × 2 mL) after coupling completion (monitor by Kaiser test)
- Repeat: Iterate steps 2-3 for each additional monomer
- Final Cleavage: Treat with cleavage cocktail (TFA:phenol:water:triisopropylsilane, 92.5:2.5:2.5:2.5) for 2 hours
- Precipitation and Purification: Precipitate in cold diethyl ether, centrifugate, and purify by reverse-phase HPLC
- Characterization: Analyze by mass spectrometry and analytical HPLC
Troubleshooting:
- Low Coupling Efficiency: Use fresh coupling reagents; extend coupling time; consider double coupling for difficult sequences
- Aggregation: Switch to more hydrophilic resin; incorporate lysine residues at C-terminus to improve solubility [77]
- Deletion Sequences: Monitor deprotection conditions; optimize piperidine concentration and exposure time
Protocol 2: PNA-CPP Conjugate Preparation and Characterization
Principle: This protocol describes the covalent conjugation of PNA to cell-penetrating peptides (CPPs) to enhance cellular uptake, using maleimide-thiol chemistry for site-specific linkage [4] [77].
Materials:
- Purified PNA: Containing C-terminal cysteine residue (for thiol conjugation)
- CPP Peptide: Synthesized with N-terminal maleimide group
- Conjugation Buffer: 0.1 M phosphate buffer, 1 mM EDTA, pH 6.5-7.0 (degassed)
- Purification System: HPLC with reversed-phase C18 column
- Characterization: MALDI-TOF mass spectrometry
Procedure:
- PNA Reduction: Dissolve 5 μmol PNA in 1 mL conjugation buffer with 10 mM TCEP (tris(2-carboxyethyl)phosphine) for 30 minutes to reduce disulfide bonds
- Conjugation Reaction:
- Add 7.5 μmol maleimide-functionalized CPP (1.5 equivalents) to reduced PNA
- React for 2-4 hours at room temperature with gentle agitation under inert atmosphere
- Reaction Monitoring: Analyze small aliquots by analytical HPLC to track conjugation progress
- Purification: Purify conjugate by semi-preparative HPLC using acetonitrile/water gradient with 0.1% TFA
- Characterization: Verify molecular weight by MALDI-TOF MS; assess purity by analytical HPLC (>90%)
- Formulation: Lyophilize pure fractions and store at -20°C for future use
Quality Control:
- Purity Assessment: Analytical HPLC should show single major peak (>90% purity)
- Mass Confirmation: Experimental molecular weight should match theoretical value within 0.1%
- Functional Validation: Assess cellular uptake in relevant cell lines by fluorescence microscopy (for labeled conjugates)
The Scientist's Toolkit: Essential Research Reagents for PNA Applications
Table 3: Key Research Reagent Solutions for PNA Therapeutic Development
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Solid Supports | TentaGel R RAM, ChemMatrix Rink amide resin | Solid-phase PNA synthesis foundation | Low-loading resins (0.1-0.2 mmol/g) reduce aggregation; PEG-based resins enhance solubility [77] |
| PNA Monomers | Fmoc-PNA-A(Bhoc)-OH, Fmoc-PNA-G(Bhoc)-OH, Fmoc-PNA-C(Bhoc)-OH, Fmoc-PNA-T-OH | Building blocks for PNA synthesis | Bhoc protection for nucleobases; Fmoc as temporary α-amine protection [77] |
| Coupling Reagents | HATU, HBTU, PyBOP | Activates carboxylic acids for amide bond formation | Use with DIPEA as base in NMP; HATU generally provides highest efficiency [77] |
| Cell-Penetrating Peptides | (RXR)₄XB, Transportan, Penetratin, TAT | Enhance cellular uptake of PNA conjugates | Arginine-rich sequences most effective; design with terminal cysteine for specific conjugation [4] [77] |
| Endosomolytic Agents | Chloroquine, Calcium ions | Enhance endosomal escape of internalized PNA | Used in research settings to demonstrate maximum potential efficacy; clinical translation challenging [4] |
| Delivery Enhancers | Lipofectamine, Interferin | Facilitate PNA delivery in cell culture | Useful for research applications; limited therapeutic applicability |
Regulatory Submission Framework and Quality Control Requirements
Preclinical Development Considerations
The regulatory submission process for PNA-based therapeutics requires comprehensive characterization and rigorous quality control measures. Key documentation requirements include:
Chemistry, Manufacturing, and Controls (CMC): Detailed description of synthetic methodology, purification processes, and analytical methods for identity, purity, and strength characterization [79] [78]. This should include:
- Complete synthetic scheme with controlled intermediates
- Specifications for starting materials and reagents
- Description of purification methods and validation data
- Stability data under proposed storage conditions
Pharmacology/Toxicology Studies: Comprehensive assessment of:
- Mechanism of action and pharmacodynamic effects
- Acute and repeat-dose toxicity in relevant species
- Biodistribution and pharmacokinetic profiles
- Genotoxicity and immunotoxicity potential
Environmental Impact Assessment: Required in certain jurisdictions for products containing novel genetic elements [80].
Diagram 2: Interrelationship Between Regulatory, Technical, and Commercialization Challenges. This diagram illustrates how regulatory factors and technical hurdles collectively impact the commercialization pathway for PNA-based products.
Clinical Trial Applications and Market Authorization
Navigating the clinical development pathway requires careful planning and region-specific strategies:
Regulatory Sequencing: Strategic initial approvals in reference regulatory authorities (e.g., FDA, EMA) can unlock expedited pathways in multiple markets through reliance mechanisms [79]. Mexico's COFEPRIS, for example, offers 30-45 day decision timelines for products already approved by reference authorities [79].
Regional Specific Considerations:
- Latin America: Leverage country-specific pathways; Brazil prioritizes public health access with delinked patent and regulatory systems [79]
- Asia: Prepare for comprehensive safety assessments in China; utilize streamlined pathways for specific PNA applications in India [80]
- Africa: Engage early with emerging regulatory frameworks in Kenya and Nigeria that offer case-by-case assessment [80]
Post-Marketing Requirements: Implement robust pharmacovigilance systems and potential risk management plans addressing:
- Long-term safety monitoring
- Special population assessments
- Potential resistance development (for antimicrobial PNAs)
The development pathway for PNA-based therapeutics presents a complex interplay of scientific innovation, regulatory navigation, and commercialization strategy. While the unique properties of PNA offer significant advantages for targeted genetic therapies, realizing this potential requires methodically addressing the substantial challenges in delivery, manufacturing, and regulatory compliance.
Future success in the PNA landscape will depend on several key factors: (1) continued advancement in delivery technologies to overcome cellular barriers; (2) development of scalable, cost-effective manufacturing processes; (3) strategic regulatory planning that leverages evolving frameworks across different regions; and (4) thoughtful intellectual property management that accounts for global variations in protection mechanisms.
As the regulatory environment continues to evolve toward greater harmonization and reliance on reference authorities, PNA developers should prioritize early engagement with regulatory agencies, implement robust quality-by-design principles in manufacturing process development, and maintain flexibility in global regulatory strategy. With only one PNA drug currently in clinical trials as of 2024, the field remains ripe for innovation, but requires careful attention to the complex interplay between scientific promise and regulatory practicalities [77].
The translation of preclinical findings into clinically effective therapies is a cornerstone of modern therapeutic development, particularly for complex conditions like cancer and genetic diseases. Preclinical models provide an indispensable platform for evaluating the efficacy, safety, and mechanism of action of novel therapeutic candidates before human trials. Within this landscape, Peptide Nucleic Acids (PNAs) represent a promising class of synthetic molecules that combine the complementary binding properties of nucleic acids with the stability of peptide-like backbones. This unique combination makes PNAs particularly suited for therapeutic applications that require high affinity and sequence-specific targeting of DNA or RNA. This Application Note delineates detailed protocols and analytical frameworks for employing preclinical models to evaluate PNA-based therapeutics, with a specific focus on oncology and genetic diseases. The content is structured to provide researchers with standardized methodologies for assessing the therapeutic potential of PNAs, contextualized within the broader thesis of advancing PNA applications in therapeutics and diagnostics.
Quantitative Efficacy Metrics in Preclinical Oncology Models
The accurate quantification of antitumor activity in preclinical models is critical for predicting clinical efficacy. The following table summarizes three principal static algebraic approaches used to characterize antitumor efficacy from xenograft experiments, along with their comparative advantages and limitations [81].
Table 1: Static Algebraic Metrics for Characterizing Preclinical Antitumor Activity
| Metric | Calculation Formula | Advantages | Limitations |
|---|---|---|---|
| Tumor/Control (T/C) Ratio | ( T/C = \frac{\text{Mean Tumor Volume}{Treated}}{\text{Mean Tumor Volume}{Control}} ) at a specific time point | Easy to calculate; widely used historically. | Heavily influenced by intrinsic tumor growth rate and measurement timing; overestimates activity in fast-growing tumors. |
| Tumor Growth Inhibition (TGI) | ( TGI = \left(1 - \frac{\Delta \text{Tumor Volume}{Treated}}{\Delta \text{Tumor Volume}{Control}}\right) \times 100\% ) Where (\Delta)Volume = Final Volume - Initial Volume | Less dependent on growth rate than T/C; correlates with clinical overall response rate. | Performance can be affected by study design and tumor growth kinetics. |
| Growth Rate Inhibition (GRI) | ( GRI = \left(1 - \frac{\text{Growth Rate}{Treated}}{\text{Growth Rate}{Control}}\right) \times 100\% ) Growth rates derived from exponential fitting of all longitudinal data. | Uses all data points; requires fewer animals; less sensitive to growth rate and study duration; superior for translational work. | Requires longitudinal tumor volume data and fitting to a growth model. |
Among these, Growth Rate Inhibition (GRI) is recommended as the most robust and translatable metric for efficacy studies, particularly for informing early clinical development decisions [81]. Its efficiency allows for statistically powerful studies with as few as six animals per treatment group.
Protocol: Evaluating PNA Efficacy in Subcutaneous Xenograft Models
This protocol describes a standardized method for assessing the antitumor activity of PNA-based therapeutics in mouse xenograft models.
Materials:
- Immunocompromised Mice (e.g., NOD/SCID or nude mice).
- Human Cancer Cells or patient-derived cells relevant to the target indication.
- PNA Therapeutic and appropriate control (e.g., scrambled PNA sequence).
- Delivery Vehicle (e.g., Phosphate-Buffered Saline (PBS) for control injections).
- Calipers for tumor volume measurement.
Procedure:
- Cell Implantation: Harvest exponentially growing cancer cells and resuspend in a 1:1 mixture of PBS and Matrigel. Subcutaneously inject 5-10 million cells into the flank of each mouse.
- Randomization: Once tumors reach a palpable size (approximately 100-200 mm³), randomize mice into treatment and control groups (n ≥ 6 per group) to ensure comparable mean tumor volumes across groups.
- Dosing Regimen:
- Treatment Group: Administer the PNA therapeutic intravenously via tail vein or intraperitoneally. The dosing schedule (e.g., once weekly, twice weekly) should be optimized based on the PNA's pharmacokinetic profile.
- Control Group: Administer an equal volume of the delivery vehicle or a scrambled PNA control on the same schedule.
- Tumor Monitoring: Measure tumor dimensions (length and width) using calipers two to three times per week for the study duration (typically 3-6 weeks). Calculate tumor volume using the formula: ( V = \frac{1}{2} \times \text{length} \times \text{width}^2 ).
- Endpoint Analysis: At the end of the study, calculate the GRI metric as defined in Table 1. Fit the longitudinal tumor volume data for each group to an exponential growth model to determine the growth rates in the control ((k{control})) and treated ((k{treated})) groups.
Figure 1: Workflow for evaluating PNA efficacy in xenograft models.
Leveraging Genetic Evidence for Target Validation
Human genetics provides a powerful tool for identifying and prioritizing drug targets with a higher probability of clinical success. Recent analyses demonstrate that drug mechanisms with human genetic evidence supporting their causal role in a disease have a 2.6-times greater probability of success from clinical development to approval compared to those without such support [82]. This effect is even more pronounced for targets linked to Mendelian diseases (e.g., via OMIM), which show a 3.7-fold increase in success probability [82]. This genetic support is crucial for validating targets for PNA-based interventions, such as those aimed at gene silencing or splice correction.
Table 2: Key Research Reagent Solutions for PNA-Based Therapeutic Development
| Research Reagent / Material | Function and Application in PNA Research |
|---|---|
| Lipid Nanoparticles (LNPs) | A primary delivery system for protecting RNA-based therapeutics (including PNA-mRNA complexes) from degradation and facilitating cellular uptake [83]. |
| Patient-Derived Cell Cultures (PDCs) | Ex vivo models that retain tumor heterogeneity and are used for high-throughput drug screening and functional profiling of PNA activity [84]. |
| Exome Sequencing Data | Used for identifying rare, protein-truncating variants and establishing gene-disease associations, thereby validating potential PNA targets [85]. |
| Machine Learning Recommender Systems | Computational tools that use historical drug screening data from cell lines to predict PNA therapeutic responses in new patient samples [84]. |
Protocol: Functional Profiling of PNA Efficacy in Patient-Derived Cells
This protocol leverages patient-derived cells (PDCs) and machine learning to create a functional profile for predicting PNA efficacy, an approach that complements target validation with genetic evidence.
Materials:
- Patient-Derived Cells (PDCs) or a diverse panel of cancer cell lines.
- Comprehensive Drug/PNA Library including the PNA therapeutic of interest.
- Viability Assay Kit (e.g., ATP-based luminescence assay).
- Software for machine learning analysis (e.g., R or Python with scikit-learn).
Procedure:
- Historical Database Creation:
- Screen a large, diverse set of PDCs (the "historical" panel) against a comprehensive library of drugs and PNAs.
- For each screen, measure cell viability and calculate a normalized bioactivity score (e.g., % inhibition) for each drug/PNA to create a "bioactivity fingerprint" for each PDC [84].
- Probing Panel Selection:
- From the comprehensive library, select a smaller panel of 30-35 drugs/PNAs that best represent the variance in the historical database's bioactivity profiles. This is the "probing panel."
- New Patient Sample Screening:
- Culture PDCs from a new patient's biopsy.
- Screen these new PDCs only against the small probing panel and generate their bioactivity profile.
- Predictive Modeling:
- Using a machine learning model (e.g., Random Forest with 50 trees), train a model on the historical database to learn the relationship between the probing panel responses and the responses to the entire library [84].
- Input the new patient's probing panel data into the trained model to predict the full bioactivity profile, identifying the top candidate PNA therapeutics for that specific patient.
Figure 2: Machine learning workflow for predicting PNA efficacy in patient-derived cells.
Translational Modeling in Preclinical Development
A rigorous translational modeling framework is essential for predicting human efficacy and toxicity from preclinical data. Mathematical models integrate pharmacokinetic (PK) and pharmacodynamic (PD) data from in vivo studies to inform clinical trial design [81].
Protocol: Developing a PK/PD Model for PNA Therapeutics
This protocol outlines the steps for building a quantitative model to translate PNA efficacy from mice to humans.
Materials:
- Animal PK/PD Data from xenograft studies (PNA concentration in plasma/tumor and corresponding tumor volume measurements over time).
- Modeling Software (e.g., NONMEM, Monolix, or R with PK/PD libraries).
Procedure:
- Data Collection: Conduct a xenograft study as in Protocol 2.1, with additional groups of mice sacrificed at various time points post-PNA administration to collect plasma and tumor samples for quantifying PNA concentration.
- PK Model Development: Fit the concentration-time data from plasma to a compartmental model (e.g., a two-compartment model) to estimate the key PK parameters: clearance (CL), volume of distribution (Vd), and half-life.
- PD Model Development: Link the PK model to the tumor growth dynamics. A commonly used TGI model structure is: ( \frac{dT}{dt} = kg \cdot T - I{max} \cdot \frac{Cp}{Cp + EC{50}} \cdot T ) where (T) is tumor volume, (kg) is the tumor growth rate, (I{max}) is the maximum inhibition rate, (Cp) is the plasma PNA concentration, and (EC_{50}) is the concentration for 50% of maximal effect.
- Human Prediction: Allometrically scale the murine PK parameters (e.g., clearance) to predict human PK. Incorporate the estimated PD parameters ((I{max}), (EC{50})) from the mouse model, assuming similar target engagement in human tumors, to simulate potential human tumor growth inhibition profiles and inform first-in-human dose selection [81].
The structured application of the protocols and analytical frameworks detailed in this document provides a robust pathway for evaluating the efficacy of PNA-based therapeutics in preclinical models for oncology and genetic diseases. By integrating quantitative efficacy metrics, functional profiling in patient-derived systems, and predictive translational modeling, researchers can make more informed decisions, thereby increasing the likelihood of clinical success. These methodologies, framed within the context of strong human genetic evidence, underscore the potential of PNAs as powerful tools for precision medicine.
Conclusion
Peptide Nucleic Acids represent a paradigm shift in molecular medicine, offering a potent and stable platform for both therapeutic intervention and diagnostic precision. Their unique chemistry enables unparalleled binding affinity and opens doors to novel mechanisms, from steric-blocking antisense therapy to non-enzymatic gene editing. While challenges in cellular delivery and navigating the translational 'Valley of Death' persist, innovative delivery strategies and chemical modifications are paving the way for clinical advancement. The robust market growth and active clinical pipeline underscore a significant and growing confidence in PNA technology. The future of PNAs is bright, lying in their continued development as targeted therapies for monogenic diseases and cancer, their integration as precision tools in companion diagnostics, and their potential to finally bridge the critical gap between groundbreaking bench-side discovery and tangible patient-side impact.
References
- 1. Peptide Nucleic Acids: Recent Developments in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0045206823005217]
- 2. Peptide nucleic acids: Advanced tools for biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7114329/]
- 3. Unlocking the potential of chemically modified peptide nucleic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10019372/]
- 4. Potential of Peptide Nucleic Acids in Future Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6311635/]
- 5. Perspectives on conformationally constrained peptide nucleic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9175113/]
- 6. Prospects for antisense peptide nucleic acid (PNA) therapies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2792880/]
- 7. Therapeutic Peptide Nucleic Acids: Principles, Limitations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5733847/]
- 8. The peptide nucleic acids (PNAs), powerful tools for ... [https://www.nature.com/articles/5201226]
- 9. Peptide nucleic acids (PNAs) [https://www.sb-peptide.com/peptide-service/custom-pna-synthesis-service/peptide-nucleic-acids/]
- 10. Thermal Stability of Peptide Nucleic Acid Complexes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6776699/]
- 11. About Peptide Nucleic Acids (PNA) [https://pnabio.com/peptide-nucleic-acid/]
- 12. Peptide nucleic acid [https://en.wikipedia.org/wiki/Peptide_nucleic_acid]
- 13. PNA-Based Biosensors for Portable Electrochemical ... [https://www.sciencedirect.com/science/article/pii/S2590137025001293]
- 14. Application of Cell-Penetrating Peptides (CPP) to Enhance ... [https://link.springer.com/article/10.1007/s10989-025-10776-1]
- 15. Parallel and Automated PNA Synthesis in μSPOT Format [https://pubmed.ncbi.nlm.nih.gov/40663327/]
- 16. Targeting RNA splicing modulation: new perspectives for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11781073/]
- 17. Targeting RNA splicing modulation: new perspectives for ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03279-w]
- 18. Genome-wide functional annotation and interpretation of ... [https://www.nature.com/articles/s10038-025-01424-z]
- 19. Translational Advances in Lipid Nanoparticle Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567512/]
- 20. Non-coding RNAs as regulators of gene expression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3096308/]
- 21. Role of non-coding RNA through nanomedicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579740/]
- 22. Non-coding RNAs: emerging biomarkers and therapeutic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1534862/full]
- 23. Molecular mechanisms of long noncoding RNAs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3199020/]
- 24. Non-Coding RNA-Targeted Therapy: A State-of-the-Art ... [https://www.mdpi.com/1422-0067/25/7/3630]
- 25. The multidimensional mechanisms of long noncoding RNA ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-017-1348-2]
- 26. Special Issue “Regulation by Non-Coding RNAs 2025” [https://www.mdpi.com/1422-0067/26/22/10885]
- 27. Long non-coding RNAs as a biomarker for homologous ... [https://www.nature.com/articles/s42003-025-08836-9]
- 28. Noncoding RNA - Applications [https://horizondiscovery.com/en/applications/rnai/noncoding-rna-applications]
- 29. Antisense oligonucleotide therapies for monogenic disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268252/]
- 30. Therapeutic and diagnostic applications of antisense peptide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10777018/]
- 31. Gene editing using gamma modified PNA: HBB gene as a ... [https://www.sciencedirect.com/science/article/pii/S1687157X25001064]
- 32. Splice-Switching Oligonucleotides (SSOs) Therapy [https://www.bocsci.com/blog/splice-switching-oligonucleotides-ssos-therapeutics-mechanism-applications-and-advances/?srsltid=AfmBOooa1Vc3Aje6WO2PUt9yihbYoKXJFDsLmCriZ7GS2Ij2GoinOcCi]
- 33. Splicing is an alternate oncogenic pathway activation ... [https://www.nature.com/articles/s41467-022-28253-4]
- 34. Off-target toxicity is a common mechanism of action ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7717492/]
- 35. Therapeutic and diagnostic applications of antisense ... [https://www.sciencedirect.com/science/article/pii/S2162253123003049]
- 36. What is Peptide Nucleic Acid (PNA)? [https://www.bocsci.com/blog/what-is-peptide-nucleic-acid-pna/?srsltid=AfmBOorUZ4uR59VxcfS5VMdqsmfFrFkE5Q3BEhpAA1IZJSZbWi6srr8X]
- 37. Gene editing using gamma modified PNA: HBB gene as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509102/]
- 38. Revolution of Biotechnology with CRISPR [https://www.nature.com/articles/s12276-025-01452-x]
- 39. Advances in large-scale DNA engineering with the ... [https://www.nature.com/articles/s12276-025-01530-0]
- 40. Harnessing artificial intelligence to advance CRISPR- ... [https://www.nature.com/articles/s41576-025-00907-1]
- 41. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 42. Peptide nucleic acid (PNA) and its applications in chemical ... [https://pubmed.ncbi.nlm.nih.gov/31541865/]
- 43. Peptide nucleic acid (PNA) and its applications in chemical ... [https://www.sciencedirect.com/science/article/pii/S1367593119300080]
- 44. PNA FISH Probes for Research [https://pnabio.com/pna-fish-probes/]
- 45. Peptide nucleic acid (PNA) clamps reduce amplification of ... [https://environmentalmicrobiome.biomedcentral.com/articles/10.1186/s40793-025-00674-w]
- 46. Simple and sensitive detection of mutations in the ras proto ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC145732/]
- 47. Truncated PNA-functionalized porous silicon biosensor for ... [https://pubmed.ncbi.nlm.nih.gov/41202786/]
- 48. PNA-SERS Biosensor for Label-Free Detection of SARS ... [https://www.sciencedirect.com/science/article/pii/S2666053925000876]
- 49. Cellular delivery of peptide nucleic acid (PNA) [https://www.sciencedirect.com/science/article/abs/pii/S0169409X02001825]
- 50. Attralus Presents New Data on Its Pan-Amyloid Diagnostic ... [https://attralus.com/press-releases/attralus-presents-new-data-on-its-pan-amyloid-diagnostic-imaging-candidates-at-asnc-2025]
- 51. A systematic review of peptide nucleic acids (PNAs) with ... [https://www.sciencedirect.com/science/article/pii/S0924857924000013]
- 52. PNA Conjugates Market - Global Forecast 2025-2030 [https://www.researchandmarkets.com/reports/6122158/pna-conjugates-market-global-forecast?srsltid=AfmBOoqeBMM3TQ06LkL-uUxWjP0XQmqpnCdG-o6ZbVS2Cc_itib7yTIR]
- 53. Peptide nucleic acid-immobilised paper combined with ... [https://www.nature.com/articles/s41598-025-86691-8]
- 54. Peptide nucleic acids: Recent advancements and future ... [https://www.sciencedirect.com/science/article/abs/pii/S0045206825000264]
- 55. The Different Cellular Entry Routes for Drug Delivery Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149500/]
- 56. PNAs in medicine: Diagnostics, therapeutics, and delivery ... [https://www.linkedin.com/posts/hlbpanagene_the-promise-of-peptide-nucleic-acids-activity-7374348669388488704-Uy7U]
- 57. Insights on chiral, backbone modified peptide nucleic acids [https://pmc.ncbi.nlm.nih.gov/articles/PMC5329900/]
- 58. Recent Advances in Chemical Modification of Peptide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3443988/]
- 59. Enhancing RNA inhibitory activity using clamp-G-modified ... [https://www.sciencedirect.com/science/article/pii/S2666386424003989]
- 60. Lipid Nanoparticle Advancements on February 25, 2025 [https://www.linkedin.com/pulse/lipid-nanoparticle-advancements-february-25-2025-precigenome-j3s5c]
- 61. Peptide Nucleic Acid Market Report | Global Forecast From ... [https://dataintelo.com/report/global-peptide-nucleic-acid-market]
- 62. How New Innovations Are Making Oligonucleotide ... [https://northpennnow.com/news/2025/sep/03/how-new-innovations-are-making-oligonucleotide-synthesis-faster-cleaner-and-more-scalable/]
- 63. Peptide Nucleic Acid Market Report 2025 (Global Edition) [https://www.cognitivemarketresearch.com/peptide-nucleic-acid-market-report]
- 64. Peptide Nucleic Acid (PNA) XX CAGR Growth Outlook 2025-2033 [https://www.archivemarketresearch.com/reports/peptide-nucleic-acid-pna-80417]
- 65. Growth Roadmap for PNA Monomers Market 2025-2033 [https://www.datainsightsmarket.com/reports/pna-monomers-542830]
- 66. Nucleic Acid Spotlights 2025 [https://www.insights.bio/nucleic-acid-insights/spotlights/year/2025]
- 67. PNA Conjugates Market - Global Forecast 2025-2030 [https://www.researchandmarkets.com/reports/6122158/pna-conjugates-market-global-forecast?srsltid=AfmBOopu_fa6Q6uqj4BK_VjrmKlsKozNhzArfSHDcQlQzx3aXouVv3VW]
- 68. Landscape of small nucleic acid therapeutics [https://www.nature.com/articles/s41392-024-02112-8]
- 69. Small interfering RNA (siRNA) Therapeutics [https://www.delveinsight.com/blog/small-interfering-rna-sirna-therapeutics-competitive-landscape-technology-and-pipeline-insights-2015-a-delveinsights-report]
- 70. RNA-Targeting Techniques: A Comparative Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563179/]
- 71. Evaluation of Peptide Nucleic Acid Encapsulation in ... [https://pubmed.ncbi.nlm.nih.gov/41134300/]
- 72. Small interfering RNA: From designing to therapeutic in ... [https://www.sciencedirect.com/science/article/pii/S1687157X25000289]
- 73. Off-target effects of oligonucleotides and approaches ... [https://www.sciencedirect.com/science/article/pii/S2472555225000474]
- 74. Strategic Insights into Peptide Nucleic Acid (PNA) ... [https://www.marketreportanalytics.com/reports/peptide-nucleic-acid-pna-159522]
- 75. Global Peptide Nucleic Acid (PNA) Market Growth 2025-2031 [https://infinitymarketresearch.com/report/peptide-nucleic-acid-market/26613]
- 76. PNA-based microbial pathogen identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3116573/]
- 77. Peptide nucleic acids (PNA) – Overview [https://intavispeptides.com/de/insights/25]
- 78. Nucleic acid drugs: recent progress and future perspectives [https://www.nature.com/articles/s41392-024-02035-4]
- 79. Regulatory Challenges in the Latin American Generic Drug ... [https://www.drugpatentwatch.com/blog/regulatory-challenges-in-the-latin-american-generic-drug-market/?srsltid=AfmBOoquat3wjJcSmdl--fcgQCO4fwUnETUaPFSEqNBdEFcM714SfY9z]
- 80. Regulatory challenges and global trade implications of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12222225/]
- 81. Quantitative translational modeling to facilitate preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5961452/]
- 82. Refining the impact of genetic evidence on clinical success [https://www.nature.com/articles/s41586-024-07316-0]
- 83. Advances in RNA-based cancer therapeutics: pre-clinical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512572/]
- 84. Establishing predictive machine learning models for drug ... [https://www.nature.com/articles/s41698-025-00937-2]
- 85. Rare variant contribution to human disease in 281104 UK ... [https://www.nature.com/articles/s41586-021-03855-y]