Antisense Oligonucleotides (ASOs): A Comprehensive Guide to Gene Silencing Mechanisms and Therapeutic Development
This article provides a comprehensive analysis of antisense oligonucleotides (ASOs), a transformative class of gene-silencing therapeutics.
Antisense Oligonucleotides (ASOs): A Comprehensive Guide to Gene Silencing Mechanisms and Therapeutic Development
Abstract
This article provides a comprehensive analysis of antisense oligonucleotides (ASOs), a transformative class of gene-silencing therapeutics. Tailored for researchers, scientists, and drug development professionals, it explores the foundational mechanisms of ASO action, from RNase H-mediated degradation to steric hindrance and splice modulation. It details the latest methodological advances in chemical modifications, delivery strategies, and computational design, alongside real-world applications in treating rare genetic and common diseases. The content further addresses critical challenges in stability, delivery, and toxicity, offering optimization strategies and validation frameworks through preclinical models and clinical trial insights. By synthesizing current research, market trends, and future directions, this resource serves as an essential reference for advancing ASO-based therapeutic programs.
The Science of Silence: Unraveling the Core Mechanisms of Antisense Oligonucleotides
Antisense oligonucleotides (ASOs) are short, synthetic, single-stranded DNA or RNA molecules, typically 13 to 25 nucleotides in length, designed to be perfectly complementary to a specific target messenger RNA (mRNA) sequence through Watson-Crick base pairing [1] [2] [3]. Since the pioneering work of Stephenson and Zamecnik in 1978, who first demonstrated that a short oligonucleotide could inhibit Rous sarcoma virus replication, ASO technology has evolved into a sophisticated therapeutic platform for modulating gene expression at the RNA level [4] [3]. This approach enables precise intervention in the central dogma of biology, targeting the intermediate step between DNA and protein to address the underlying causes of genetic disorders.
ASOs represent a powerful tool in the gene silencing research arsenal, offering a unique combination of high specificity, programmable design, and mechanistic versatility. Their ability to target previously "undruggable" pathways and their applicability to both rare and common diseases have positioned ASOs as a transformative modality in precision medicine, with multiple FDA-approved therapies and a robust pipeline of clinical candidates [4] [5] [2].
Basic Structure and Chemical Modifications
The fundamental structure of an ASO consists of a short chain of nucleosides linked by phosphodiester bonds. Each nucleoside comprises a nitrogenous base (adenine, cytosine, guanine, thymine, or uracil), a pentose sugar (deoxyribose or ribose), and a phosphate group [1]. However, natural oligonucleotides are highly susceptible to degradation by intracellular nucleases, necessitating chemical modifications to enhance their stability, specificity, and cellular uptake.
Table 1: Common Chemical Modifications in ASO Design
| Modification Type | Description | Primary Function | Examples |
|---|---|---|---|
| Backbone Modification | Replacement of non-bridging oxygen with sulfur in phosphate group | Increases nuclease resistance and enhances protein binding | Phosphorothioate (PS) |
| Sugar Modification | Modification at the 2' position of the ribose sugar | Enhances binding affinity to target RNA and improves stability | 2'-O-methyl (2'-OMe), 2'-O-methoxyethyl (2'-MOE), Locked Nucleic Acid (LNA) |
| Conjugate Groups | Attachment of specific molecules to the oligonucleotide | Improves targeted delivery to specific tissues or cells | GalNAc (for hepatocyte targeting), lipids, peptides, antibodies |
These chemical modifications are crucial for overcoming the inherent challenges of oligonucleotide therapeutics. Phosphorothioate modifications, for instance, not only increase resistance to nucleases but also promote protein binding, which facilitates cellular uptake and influences tissue distribution [1] [6]. The evolution of ASO chemistry has progressed through generations of improvements, with third-generation modifications like phosphorodiamidate morpholino oligomers (PMOs) offering enhanced binding affinity and reduced toxicity profiles [1] [3].
Mechanisms of Action
ASOs modulate gene expression through diverse mechanisms, broadly categorized into those that degrade target RNA and those that act through steric blockade without degradation. The specific mechanism employed depends on ASO chemistry, design, and binding location within the target transcript.
RNase H1-Dependent Degradation
This mechanism utilizes gapmer designs, where the ASO contains a central DNA "gap" region flanked by chemically modified RNA-like nucleotides on both ends. Upon hybridization to the target mRNA, the DNA-RNA heteroduplex recruits the ubiquitous cellular enzyme RNase H1, which cleaves the RNA strand, leading to mRNA degradation and subsequent suppression of gene expression [4] [2]. This approach is particularly useful for reducing the expression of pathogenic transcripts in gain-of-function disorders.
Steric Blockade
Steric-blocking ASOs physically obstruct access to specific sequences on the target RNA without inducing degradation. This mechanism enables several sophisticated applications:
- Splicing Modulation: Splice-switching ASOs (SSOs) bind to pre-mRNA and modulate alternative splicing by blocking the binding of splicing factors to regulatory sequences. This can promote exon inclusion (e.g., nusinersen for spinal muscular atrophy) or exon exclusion (e.g., eteplirsen for Duchenne muscular dystrophy) [4] [5].
- Translation Inhibition: ASOs can bind to the translation start site or other regulatory regions, physically blocking the ribosomal machinery and preventing protein synthesis [3].
- miRNA Inhibition: ASOs can function as "antagomirs" by binding to and sequestering microRNAs, thereby preventing them from repressing their natural mRNA targets [3].
Targeted Augmentation of Nuclear Gene Output (TANGO)
TANGO strategies represent a novel approach to increase protein production from specific genes through ASO-mediated mechanisms:
- Targeting Poison Exons: ASOs can block the splicing of naturally occurring "poison exons" that would otherwise lead to non-productive mRNA, thereby increasing functional mRNA and protein levels [4].
- Blocking Translational Repressive Elements: ASOs can bind to upstream open reading frames (uORFs) or other translation-suppressive motifs within mRNA untranslated regions (UTRs), relieving repression and enhancing translation of the main coding sequence [4] [3].
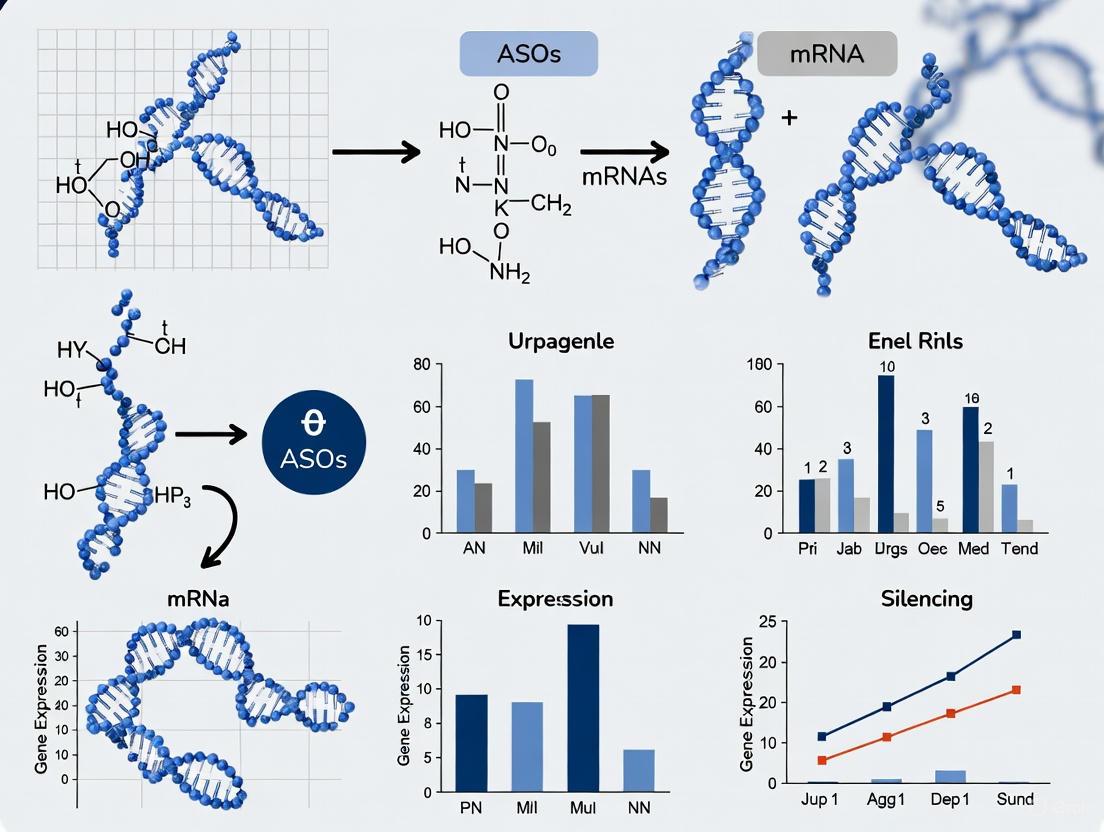
Diagram 1: Diverse Mechanisms of ASO Action. ASOs can modulate gene expression through degradation, steric blockade, or upregulation pathways depending on their design and cellular context.
ASO Synthesis and Design Considerations
Synthesis Protocol
ASO synthesis primarily utilizes solid-phase phosphoramidite chemistry, which enables efficient, stepwise oligonucleotide assembly [1]. The detailed protocol involves the following steps:
Deprotection: The 5'-end protecting group (typically dimethoxytriphenyl, DMT) is removed using trichloroacetic acid (TCA) or dichloroacetic acid (DCA), preparing the growing chain for nucleotide addition.
Coupling: The 3'-OH of the incoming phosphoramidite monomer is activated by tetrazole, forming a reactive intermediate that links to the 5'-end of the support-bound oligonucleotide chain.
Capping: Any unreacted 5'-OH groups (failed couplings) are blocked ("capped") with acetic anhydride and N-methylimidazole to prevent the formation of deletion sequences in subsequent cycles.
Oxidation: The newly formed phosphite triester linkage is oxidized to a more stable phosphate (or phosphorothioate) using iodine/water or a sulfurization reagent.
Cleavage and Deprotection: After complete sequence assembly, the oligonucleotide is cleaved from the solid support (typically controlled pore glass, CPG) and all protecting groups are removed under specific conditions.
This synthetic approach enables the production of high-quality ASOs with various modifications, though careful purification is required to remove truncated sequences, longer sequences, and other impurities that may form during synthesis [1].
Critical Design Considerations
Successful ASO design requires attention to multiple factors beyond simple sequence complementarity:
Target Accessibility: mRNA folds into secondary and tertiary structures that can impede ASO binding. Target sites should be selected in unpaired regions, which can be predicted computationally or identified experimentally through methods like RNase H mapping [1] [7].
Sequence Specificity: ASOs should be designed to uniquely target the intended RNA sequence. BLAST analysis is recommended to ensure minimal off-target hybridization to unrelated transcripts [1].
Avoidance of Immunostimulatory Motifs: Unmethylated CpG dinucleotides can stimulate immune responses and should be avoided in ASO design [1].
Thermodynamic Properties: GC content and secondary structure formation of the ASO itself should be optimized to balance binding affinity and specificity.
Advanced design approaches are emerging, including structure-based methods that consider the three-dimensional architecture of target RNAs. These "3D-ASO" designs employ tertiary interaction templates derived from natural RNA structures like pseudoknots, enabling enhanced affinity and specificity for structured target sites [7].
Therapeutic Applications and Clinical Protocols
ASOs have demonstrated significant therapeutic potential across diverse disease areas, particularly for monogenic disorders. Their application spans neurogenetic, metabolic, and oncologic disorders, with emerging n-of-1 approaches for ultra-rare conditions [4].
Table 2: Selected Approved ASO Therapies and Their Applications
| Drug Name | Target Condition | Mechanism | Administration Route | Key Clinical Outcome |
|---|---|---|---|---|
| Nusinersen (Spinraza) | Spinal Muscular Atrophy | Splicing modulation of SMN2 gene | Intrathecal | Improved motor function in infants and children |
| Eteplirsen (Exondys 51) | Duchenne Muscular Dystrophy | Exon skipping in dystrophin gene | Intravenous | Increased dystrophin production |
| Tofersen (Qalsody) | SOD1-ALS | RNase H-mediated degradation of mutant SOD1 mRNA | Intrathecal | Reduced SOD1 protein levels in CSF |
| Inotersen (Tegsedi) | hATTR Amyloidosis | RNase H-mediated knockdown of TTR mRNA | Subcutaneous | Improved neuropathy and quality of life |
Administration and Delivery Protocols
Effective ASO delivery remains a critical consideration in therapeutic development:
Central Nervous System Delivery: Intrathecal administration bypasses the blood-brain barrier, allowing ASOs to directly reach neurons and glial cells in the brain and spinal cord. The slow clearance from cerebrospinal fluid enables sustained effects with intermittent dosing [4]. Clinical protocols for nusinersen, for example, involve loading doses followed by maintenance dosing every four months.
Hepatic Delivery: The liver efficiently takes up ASOs via receptor-mediated endocytosis. Systemic administration (intravenous or subcutaneous) is effective for hepatocyte targets, with conjugation to GalNAc ligands significantly enhancing delivery specificity and potency through engagement with the asialoglycoprotein receptor [4] [8].
Emerging Delivery Strategies: Chemically inducible ASOs (iASOs) represent an innovative approach for cell-selective activation. For example, phenylboronic acid-caged iASOs remain inactive until triggered by hydrogen peroxide, enabling tumor-cell-selective gene silencing [9]. Additionally, antibody-oligonucleotide conjugates and nanoparticle formulations are being developed for tissue-specific targeting [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for ASO Experiments
| Reagent/Category | Function in Research | Specific Examples & Applications |
|---|---|---|
| Phosphoramidite Reagents | Building blocks for ASO synthesis | DNA/RNA phosphoramidites with protective groups (DMT, β-cyanoethyl) for solid-phase synthesis |
| Chemical Modification Reagents | Introduce nuclease resistance and enhance binding | Phosphorothioate reagents, 2'-O-methyl, 2'-MOE, LNA phosphoramidites for ASO optimization |
| Delivery/Targeting Reagents | Facilitate cellular uptake and tissue-specific delivery | GalNAc conjugation reagents, lipid nanoparticles (LNPs), cell-penetrating peptides |
| Solid Support Materials | Platform for automated oligonucleotide synthesis | Controlled pore glass (CPG) beads with appropriate linkers for various synthesis scales |
| Analytical Standards | Quality control and quantification | HPLC standards, reference materials for purity assessment and bioanalytical method development |
| Enzymatic Tools | Mechanism of action studies | Recombinant RNase H1, Argonaute 2 (Ago2) for in vitro characterization of ASO activity |
Comparison with Other Gene Silencing Modalities
ASOs are often compared with small interfering RNAs (siRNAs), another prominent oligonucleotide therapeutic platform. While both modalities achieve gene silencing through sequence-specific RNA targeting, they differ in several key aspects:
Diagram 2: Comparative Analysis of ASO and siRNA Platforms. While both are oligonucleotide therapeutics, ASOs and siRNAs differ in fundamental properties and therapeutic applications.
ASOs offer distinct advantages for certain applications, particularly their ability to target nuclear RNAs, achieve allele-selective silencing for dominant disorders, and employ multiple mechanisms beyond simple degradation [6]. However, both platforms continue to evolve with improvements in chemistry and delivery systems.
Antisense oligonucleotides have matured from a theoretical concept to a validated therapeutic platform with multiple approved drugs and a robust clinical pipeline. Their precise mechanism of action, programmability, and ability to target previously undruggable pathways position ASOs as powerful tools in the gene silencing research arsenal and precision medicine.
Future developments in ASO technology will likely focus on overcoming remaining challenges, particularly delivery to tissues beyond the liver and central nervous system. Innovations in conjugate chemistry, cell-specific activation strategies (such as iASOs), and advanced formulations will expand the therapeutic reach of ASOs [9] [8]. Furthermore, structure-based design approaches that account for RNA three-dimensional architecture promise to enhance the efficiency and specificity of future ASO therapeutics [7].
As the field advances, ASOs are poised to make increasingly significant contributions to the treatment of genetic disorders, cancer, and other diseases with well-defined molecular targets, ultimately fulfilling their potential as a versatile and precise modality for genetic medicine.
Antisense oligonucleotides (ASOs) are short, synthetic, single-stranded nucleic acids, typically 13-30 nucleotides in length, designed to modulate gene expression by binding to target RNA molecules via Watson-Crick base pairing [10] [11] [3]. They represent a powerful therapeutic platform for treating genetic disorders, with multiple drugs receiving FDA approval. ASOs primarily function through two distinct mechanistic categories: those that enzymatically degrade their target RNA (e.g., RNase H-mediated degradation) and those that sterically hinder cellular processes without degrading the RNA [10] [12]. The choice between these mechanisms depends on the therapeutic goal, target RNA sequence, and cellular context, and is fundamentally determined by the ASO's chemical design [10] [11].
The following diagram illustrates the fundamental mechanistic divergence between these two primary ASO action pathways.
RNase H-Mediated Degradation Pathway
Mechanism and Molecular Machinery
RNase H-mediated degradation is an enzymatic mechanism that results in the cleavage and destruction of the target RNA [10] [13]. This pathway is initiated when a DNA-like ASO base-pairs with its complementary target mRNA to form an RNA-DNA heteroduplex [10]. This heteroduplex is then recognized by the cellular enzyme RNase H1, an endonuclease present in both the nucleus and cytoplasm [10] [13]. RNase H1 cleaves the RNA strand within the heteroduplex region, leading to subsequent degradation of the mRNA by cellular exonucleases [10]. The resulting mRNA fragments, lacking protective 5'-cap and poly-A tail structures, are rapidly degraded, preventing translation of the encoded protein [13].
The efficiency of RNase H cleavage depends on several factors, including the length and stability of the RNA-DNA hybrid, with more stable, perfectly complementary hybrids promoting stronger RNase H binding and cleavage activity [13]. This mechanism is particularly exploited by gapmer ASOs, which contain a central DNA "gap" region (typically 8-10 deoxynucleotides) flanked by modified RNA nucleotides that confer nuclease resistance and enhance binding affinity but do not support RNase H activity [11] [12].
Experimental Protocol for RNase H-Dependent ASOs
Objective: To evaluate the efficacy of RNase H-dependent ASOs in reducing target mRNA levels in mammalian cell culture.
Materials:
- Gapmer ASOs: Design with 16-20 nucleotide length, including 8-10 DNA nucleotides in the central gap, flanked by 2'-O-methoxyethyl (2'-MOE) or LNA-modified wings [11] [13].
- Cell Line: Appropriate mammalian cell line expressing the target mRNA.
- Transfection Reagent: Cytofectin or Lipofectamine RNAiMAX [14].
- Lysis Buffer: RIPA buffer for protein isolation, RLT buffer for RNA isolation [14].
- Analysis Reagents: Primers for qRT-PCR, antibodies for Western blot.
Procedure:
- ASO Design and Preparation: Design gapmer ASOs complementary to the target mRNA region. Include appropriate negative control ASOs with scrambled sequences.
- Cell Seeding: Plate cells in appropriate culture media 24 hours before transfection to achieve 60-80% confluency.
- Transfection: Transfect cells with 50 nM ASO using 3 μg/mL Cytofectin transfection reagent for 24 hours [14].
- RNA Isolation: Harvest total cellular RNA using RNeasy kit 24-48 hours post-transfection.
- qRT-PCR Analysis: Perform quantitative RT-PCR using approximately 10 ng RNA with TaqMan primer and probe sets specific to the target mRNA. Normalize to Ribogreen or housekeeping genes [14].
- Protein Analysis: Isolate protein using RIPA buffer with protease inhibitors. Perform Western blot with 10-40 μg protein lysate to confirm reduction of target protein [14].
- Data Analysis: Calculate mRNA reduction using the relative standard curve method compared to negative control ASOs.
Steric Hindrance Mechanism
Mechanism and Functional Outcomes
In contrast to RNase H-mediated degradation, steric hindrance ASOs function without degrading the target RNA by physically blocking access to specific sequence elements or protein-binding sites [10] [11]. These ASOs are fully modified with chemical groups such as 2'-O-methyl (2'-OMe), 2'-O-methoxyethyl (2'-MOE), or phosphorodiamidate morpholino (PMO) throughout their sequence, making them resistant to RNase H recognition while increasing target affinity and nuclease stability [14] [15]. The therapeutic effects are achieved through several mechanisms:
- Splice Modulation: ASOs bind to splice regulatory elements (donor/acceptor sites, branch points, enhancers, or silencers) in pre-mRNA, redirecting splicing machinery to promote exon inclusion or exclusion [10] [12]. This approach can restore reading frames or skip exons containing disease-causing mutations.
- Translational Blockade: ASOs binding to the 5' untranslated region (UTR) or start codon can sterically hinder ribosome assembly or scanning, preventing translation initiation [10] [3].
- Modulation of RNA Function: ASOs can block regulatory elements such as upstream open reading frames (uORFs) or microRNA binding sites, thereby increasing translation of the main ORF [11] [3].
- Indirect Degradation Pathways: Some steric-blocking ASOs can be designed to promote aberrant splicing that introduces premature termination codons (PTCs), leading to transcript degradation via the nonsense-mediated decay (NMD) pathway [14].
Experimental Protocol for Steric-Blocking ASOs
Objective: To assess the splice-modulating activity of steric-blocking ASOs in cell culture.
Materials:
- Steric-Blocking ASOs: Fully modified 18-25 nucleotide ASOs with 2'-OMe, 2'-MOE, or PMO modifications [14] [15].
- Cell Line: HeLa or other relevant cell lines expressing the target pre-mRNA.
- Transfection Reagent: Lipofectamine RNAiMAX or Cytofectin.
- RNA Isolation Kit: RNeasy kit or equivalent.
- RT-PCR Reagents: Reverse transcriptase, PCR polymerase, gel electrophoresis equipment.
Procedure:
- ASO Design: Design ASOs complementary to splice acceptor/donor sites, exonic splicing enhancers, or silencers of the target pre-mRNA.
- Cell Transfection: Plate cells and transfect with 50 nM ASO using appropriate transfection reagent for 24 hours [14].
- RNA Isolation: Harvest total RNA 24-48 hours post-transfection.
- RT-PCR Analysis: Reverse transcribe 400 ng RNA using random hexamers. Perform PCR with primers flanking the target exon.
- Gel Electrophoresis: Resolve PCR products on 5% non-denaturing polyacrylamide gels and stain with ethidium bromide [14].
- Quantification: Image gels and calculate the percentage of exon skipping/inclusion using band intensity: [exon exclusion band / (inclusion band + exclusion band)] × 100, with correction for DNA content per band [14].
- Validation: Sequence PCR products to confirm accurate splicing patterns.
Comparative Analysis: Key Distinctions
The table below summarizes the fundamental differences between RNase H-mediated degradation and steric hindrance mechanisms, highlighting their distinct applications, design requirements, and experimental considerations.
| Parameter | RNase H-Mediated Degradation | Steric Hindrance |
|---|---|---|
| Primary Mechanism | Enzymatic cleavage of target RNA [10] [13] | Physical blockade of RNA function [10] [11] |
| Effect on Target RNA | Degradation [10] | Modification of function/splicing; no degradation [10] |
| ASO Chemical Structure | Gapmer (DNA core with modified flanking regions) [11] [12] | Fully modified (uniform 2'-MOE, 2'-OMe, PMO, etc.) [14] |
| Therapeutic Applications | Reducing expression of toxic proteins [12] | Exon skipping, splice correction, translation modulation [10] [12] |
| Cellular Localization | Nucleus and cytoplasm [10] | Primarily nucleus for splicing modulation [10] |
| Key Enzymes/Pathways | RNase H1 [10] [13] | Spliceosome, NMD pathway (indirectly) [14] |
| Experimental Readout | mRNA reduction (qRT-PCR), protein reduction (Western) [14] | Splicing changes (RT-PCR), protein isoform detection [14] |
The following workflow diagram outlines the key decision points for researchers when selecting between these two fundamental ASO mechanisms for their experimental or therapeutic goals.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of ASO experiments requires specific reagent solutions designed for nucleic acid therapeutics research. The table below outlines key materials and their functions.
| Research Reagent | Function/Application |
|---|---|
| Gapmer ASOs (DNA core with 2'-MOE/LNA wings) | Enable RNase H-mediated target RNA degradation [11] [12] |
| Steric-Blocking ASOs (fully modified 2'-OMe, PMO) | Modulate splicing or translation without degradation [14] [15] |
| Cytofectin Transfection Reagent | Efficient delivery of ASOs into mammalian cells [14] |
| RNeasy Kit | High-quality total RNA isolation for downstream qRT-PCR and splicing analysis [14] |
| TaqMan Primer/Probe Sets | Specific detection and quantification of target mRNA levels via qRT-PCR [14] |
| RNase H1 Enzyme | In vitro validation of gapmer ASO mechanism and activity [13] |
RNase H-mediated degradation and steric hindrance represent two fundamental, mechanistically distinct approaches for ASO-based gene regulation. The RNase H pathway is ideal for applications requiring reduction of specific RNA transcripts, particularly for gain-of-function mutations where decreasing protein levels is therapeutic [12]. In contrast, steric hindrance ASOs offer precise control over RNA processing through splice modulation and translational regulation, making them suitable for restoring functional protein expression in loss-of-function disorders [10] [12]. The choice between these mechanisms directly influences ASO design, chemical modification strategy, experimental protocols, and expected outcomes. Understanding these distinctions enables researchers to strategically select the optimal approach for their specific research objectives in gene function studies or therapeutic development.
Application Notes: Clinical Translation and Therapeutic Landscape
Splicing modulation therapies, particularly those utilizing antisense oligonucleotides (ASOs), have emerged as a powerful precision medicine platform for treating genetic disorders caused by loss-of-function mutations. These therapies function by manipulating the natural process of pre-mRNA splicing to correct disease-causing genetic errors, either by excluding problematic exons or including critical ones to restore functional protein expression [16] [17].
FDA-Approved Exon-Skipping Therapies for Duchenne Muscular Dystrophy
The most advanced clinical application of exon skipping is for Duchenne muscular dystrophy (DMD), an inherited progressive muscle disease caused by variants in the DMD gene that disrupt the reading frame of dystrophin mRNA [18] [19]. ASO-mediated exon skipping converts out-of-frame deletions to in-frame deletions, enabling the production of partially functional dystrophin proteins [18].
Table 1: FDA-Approved Exon-Skipping Therapies for DMD
| Therapeutic Agent | Target Exon | Year Approved | Mechanism | Patient Population |
|---|---|---|---|---|
| Eteplirsen [16] [18] | Exon 51 | 2016 (Accelerated Approval) | Phosphorodiamidate morpholino oligomer (PMO) that binds exon 51 splicing enhancer | ~13% of DMD patients amenable to exon 51 skipping |
| Golodirsen [16] [20] | Exon 53 | 2019 (Accelerated Approval) | PMO that induces exclusion of exon 53 from mature mRNA | ~8% of DMD patients amenable to exon 53 skipping |
| Viltolarsen [16] [17] | Exon 53 | 2020 (Accelerated Approval) | PMO that binds regulatory elements to promote exon 53 skipping | ~8% of DMD patients amenable to exon 53 skipping |
| Casimersen [16] [20] | Exon 45 | 2021 (Accelerated Approval) | PMO designed to skip exon 45 during pre-mRNA processing | ~8% of DMD patients amenable to exon 45 skipping |
The confirmatory Phase 3 ESSENCE trial (96 weeks) for golodirsen and casimersen recently completed, reporting numerical trends favoring treatment over placebo despite not achieving statistical significance on the primary endpoint (4-step ascend velocity). Importantly, when excluding participants impacted by COVID-19-related dosing interruptions (43% of cohort), the data demonstrated clinically meaningful slowing of disease progression [20].
Exon Inclusion Therapy for Spinal Muscular Atrophy
Splice-switching ASOs can also promote beneficial exon inclusion, as exemplified by nusinersen (Spinraza) for spinal muscular atrophy (SMA) [17]. SMA is caused by mutations in the SMN1 gene. Nusinersen targets the SMN2 pre-mRNA to promote inclusion of exon 7, resulting in increased production of full-length, functional SMN protein and dramatically improved patient outcomes [17] [21].
Emerging Applications in Oncology
Aberrant RNA splicing is a molecular hallmark present in almost all cancer types, with tumors exhibiting up to 30% more alternative splicing events than normal tissues [22]. This creates new therapeutic opportunities for splice-modulating ASOs to:
- Correct cancer-specific aberrant splicing that drives tumorigenesis [22]
- Generate neoantigens that enhance immunotherapeutic responses [22]
- Reverse splicing events that confer resistance to conventional therapies [22]
Table 2: Key Splicing Aberrations and Therapeutic Opportunities in Cancer
| Splicing Factor/Alteration | Cancer Type | Functional Consequence | Therapeutic Strategy |
|---|---|---|---|
| SRSF1 Upregulation [22] | Lung, Pancreatic, Brain, Breast | Promotes oncogenic isoform switching | ASO-mediated silencing or splice correction |
| SRSF3 Overexpression [22] | Breast, Cervical, Nasopharyngeal | Enhances cancer cell proliferation | Targeted exon skipping or inclusion |
| hnRNPA1 Dysregulation [22] | Multiple Solid Tumors | Promotes PKM2 isoform, enhancing glycolysis | Splice-switching to favor PKM1 isoform |
| Mutations in SF3B1, U2AF1, SRSF2 [22] | Hematological malignancies, Solid tumors | Disrupted splice site recognition | Corrective ASOs or small molecule inhibitors |
Protocols: Experimental Framework for Splice-Modulating ASO Development
Protocol 1: In Silico Prediction and Design of Splice-Switching ASOs
Purpose: To computationally identify and prioritize splice-disruptive variants and design candidate ASOs for experimental validation.
Background: An estimated 15-30% of all disease-causing mutations affect splicing through disruption of canonical splice sites, activation of cryptic sites, or alteration of regulatory elements [17]. Genome-first approaches using whole-genome sequencing enable systematic detection of these variants.
Materials:
- Genomic DNA or whole-genome sequencing data
- Splicing prediction software (e.g., SpliceAI, ESEfinder, NNSPLICE)
- ASO design platform
Procedure:
Variant Identification: Annotate whole-genome sequencing data using pipelines that incorporate deep learning-based splicing prediction models (e.g., SpliceAI) to score potential splice-disruptive effects of variants, including deep-intronic and synonymous changes [17].
Variant Prioritization: Filter and prioritize variants based on:
- Predicted impact on splicing regulatory elements (ESEs, ESSs, ISEs, ISSs)
- Evolutionary conservation of affected nucleotides
- Population allele frequency
- Proximity to exon-intron boundaries [17]
ASO Target Selection: Identify optimal ASO binding sites within pre-mRNA that:
ASO Sequence Design: Design 15-25 nucleotide ASOs with:
- Perfect complementarity to the target pre-mRNA region
- Appropriate chemical modifications (e.g., 2'-O-methyl, 2'-MOE, PMO) for enhanced stability and binding affinity [21]
Figure 1: Computational workflow for predicting splice-disruptive variants and designing targeted ASOs.
Protocol 2: Experimental Validation of Splicing Correction
Purpose: To empirically test the efficacy of candidate ASOs in modulating splicing patterns in cellular models.
Background: ASOs act through steric blockade to prevent spliceosomal components or regulatory factors from accessing pre-mRNA targets. For DMD, ASOs bind to splicing enhancer sequences within exons, leading to exon exclusion and restoration of the dystrophin reading frame [18] [19].
Materials:
- Patient-derived fibroblasts or myoblasts
- Control cell lines (wild-type)
- Candidate ASOs and scrambled control ASOs
- Transfection reagent
- RNA extraction kit
- RT-PCR reagents
- Gel electrophoresis system
- Western blot apparatus
- Dystrophin-specific antibodies (for DMD models)
Procedure:
Cell Culture and Transfection:
- Culture patient-derived cells (e.g., fibroblasts or myoblasts) harboring the target mutation in appropriate growth media.
- Transfect cells with candidate ASOs (0.1-100 nM range) using lipid-based transfection reagents. Include untransfected and scrambled ASO controls.
- Incubate cells for 24-72 hours to allow splicing modulation.
RNA Analysis:
- Extract total RNA using silica-membrane columns.
- Perform reverse transcription to generate cDNA.
- Amplify target region by PCR using primers flanking the exon of interest.
- Analyze PCR products by agarose gel electrophoresis to visualize splicing patterns:
- Successful exon skipping will yield a shorter PCR product.
- Successful exon inclusion will yield a longer PCR product.
- Quantify band intensity to determine splicing correction efficiency.
Protein Analysis (for DMD models):
- Lyse cells for protein extraction 48-96 hours post-transfection.
- Separate proteins by SDS-PAGE and transfer to membranes.
- Probe membranes with dystrophin-specific antibodies to detect restored protein expression.
- Compare expression levels to wild-type controls and untreated cells.
Figure 2: Experimental workflow for validating ASO-mediated splicing correction in cellular models.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Splice-Modulation Research
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| ASO Chemistries [21] | Phosphorodiamidate morpholino oligomers (PMOs), 2'-O-methyl (2'-OMe), 2'-O-methoxyethyl (2'-MOE) | Backbone modifications that enhance nuclease resistance, improve binding affinity, and reduce toxicity |
| Delivery Systems [2] | Lipid nanoparticles (LNPs), GalNAc conjugates, Dynamic polyconjugates | Enhance cellular uptake and targeted delivery of ASOs to specific tissues (e.g., liver, muscle) |
| Cell Models [17] | Patient-derived fibroblasts, Myoblasts, Induced pluripotent stem cells (iPSCs) | Provide physiologically relevant systems for testing ASO efficacy and mechanism of action |
| Splicing Prediction Tools [17] | SpliceAI, ESEfinder, NNSPLICE | Computational platforms to predict splice-disruptive variants and optimize ASO target sequences |
| Validation Reagents | Splice-junction specific primers, Isoform-specific antibodies | Enable detection and quantification of successful splicing correction at RNA and protein levels |
Molecular Mechanism of Splice-Switching ASOs
Figure 3: Molecular mechanism of splice-switching ASOs. ASOs bind pre-mRNA to sterically block splicing regulatory elements, leading to either exon skipping or inclusion.
Antisense oligonucleotide (ASO) technology represents a transformative approach for modulating gene expression through sequence-specific targeting of RNA. This application note details the historical evolution, molecular mechanisms, and standardized protocols for implementing ASO therapies in research and clinical settings. We provide a comprehensive timeline of key developments from conceptual origins to approved therapies, along with experimental workflows and reagent specifications to support drug development professionals in leveraging this powerful technology. The content is structured to facilitate practical implementation while contextualizing advances within the broader framework of genetic medicine.
Antisense oligonucleotides (ASOs) are short, synthetic, single-stranded DNA or RNA molecules designed to bind complementary target RNA sequences through Watson-Crick base pairing, enabling precise control of gene expression at multiple regulatory levels [3]. Since their conceptualization, ASOs have evolved from laboratory tools to sophisticated therapeutics capable of addressing previously undruggable genetic targets.
The fundamental principle of ASO technology involves designing oligonucleotides complementary to specific RNA targets, which upon binding can modulate RNA function through various mechanisms including RNase H-mediated degradation, steric blockade, and splice modulation [23] [12]. This versatility has established ASOs as invaluable tools for functional genomics and as promising therapeutic modalities for monogenic disorders, with 15 oligonucleotide drugs having received market authorization as of 2024 [12].
This document provides researchers with both historical context and practical methodologies for implementing ASO technologies, emphasizing the progression from basic research to clinical application.
Historical Timeline of ASO Development
The development of ASO technology spans nearly five decades, marked by key conceptual, technical, and clinical breakthroughs. The table below summarizes major milestones in ASO evolution.
Table 1: Historical Timeline of Key ASO Developments
| Year | Development | Significance | Key Researchers/Organizations |
|---|---|---|---|
| 1978 | First demonstration of antisense principle | Synthetic oligonucleotide inhibited Rous sarcoma virus replication [23] [24] | Zamecnik and Stephenson |
| 1979 | RNase H mechanism described | Established enzyme-mediated degradation of RNA in DNA-RNA hybrids [24] | Donis-Keller |
| 1980s | Phosphorothioate backbone modification | Greatly improved nuclease resistance and pharmacokinetics [23] [25] | Multiple groups |
| 1998 | First ASO drug approved (Fomivirsen) | Approved for CMV retinitis; validated ASOs as therapeutics [24] [26] [25] | FDA/EMEA |
| 2000s | Advanced chemical modifications (2'-MOE, LNA) | Enhanced binding affinity and specificity [23] | Multiple groups |
| 2011-2016 | Splice-switching ASOs approved | Eteplirsen (2016) for DMD; Nusinersen (2016) for SMA [26] [25] | FDA/EMEA |
| 2018-2023 | Expansion to neurodegenerative diseases | Inotersen (2018) for amyloidosis; Tofersen (2023) for ALS [25] | FDA/EMEA |
The initial concept of "complementary-addressed modification" was formulated in 1967 by Grineva, who proposed that attaching active chemical groups to oligonucleotides could direct them to specific nucleic acid fragments [24]. However, the field languished until the late 1970s due to challenges with oligonucleotide synthesis, cellular delivery, and limited genomic sequence information [24].
The modern era of ASO technology began with Zamecnik and Stephenson's 1978 demonstration that a synthetic 13-mer oligodeoxynucleotide could inhibit Rous sarcoma virus replication [23] [24]. This established the core antisense principle and suggested therapeutic potential. The subsequent discovery that RNase H cleaves the RNA strand of DNA-RNA hybrids provided a crucial mechanistic foundation for ASO activity [24].
The first-generation ASO chemical modification—phosphorothioate (PS) linkages—significantly improved stability against nuclease degradation and enhanced protein binding for better tissue distribution [23] [25]. The first ASO drug, fomivirsen (Vitravene), approved in 1998, targeted cytomegalovirus retinitis in AIDS patients and validated the entire therapeutic approach [26] [25].
Second-generation modifications (2'-O-alkyl RNAs like 2'-O-methyl and 2'-O-methoxyethyl) further improved binding affinity and nuclease resistance [23]. The most significant advance came with locked nucleic acid (LNA) and other bridged nucleic acids (BNAs), which dramatically increased affinity for complementary sequences [23].
The clinical landscape expanded with splice-switching ASOs, particularly for Duchenne muscular dystrophy (eteplirsen, 2016) and spinal muscular atrophy (nusinersen, 2016) [26] [25]. Most recently, ASOs have addressed neurodegenerative diseases including amyotrophic lateral sclerosis (tofersen, 2023) [25].
Molecular Mechanisms of ASO Action
ASOs employ diverse mechanisms to modulate gene expression, determined by their chemical properties and target sites. The diagram below illustrates the primary mechanistic pathways.
Diagram 1: Primary Mechanisms of ASO Action. ASOs function through multiple pathways depending on their design and cellular localization, leading to either mRNA degradation or modulation of protein function. Abbreviations: ssASOs: splice-switching ASOs; RISC: RNA-induced silencing complex.
Key Mechanistic Pathways
RNase H-Mediated Degradation
Gapmer ASOs contain a central DNA region flanked by modified nucleotides (e.g., 2'-MOE or LNA). The DNA segment forms heteroduplexes with target mRNA, recruiting RNase H1 which cleaves the RNA strand [23] [12]. This pathway primarily operates in the nucleus and results in sustained reduction of target RNA levels.
Splice Modulation
Splice-switching ASOs (ssASOs) bind to pre-mRNA sequences and modulate splicing by blocking splice regulatory elements (splice sites, branch points, enhancers, or silencers) [12]. This can cause exon inclusion or exclusion, potentially restoring reading frames or altering protein isoforms. Successful applications include nusinersen for spinal muscular atrophy, which promotes inclusion of exon 7 in SMN2 transcripts [26].
Steric Blockade
ASOs can physically block ribosome assembly, translation initiation, or protein binding without degrading the target RNA [23]. This mechanism is employed by chemically modified ASOs (e.g., 2'-O-alkyl, PMO, PNA) that do not activate RNase H.
RNA Interference Pathway
Small interfering RNAs (siRNAs), while distinct from single-stranded ASOs, represent a related oligonucleotide therapeutic approach. siRNAs are double-stranded and operate through the RNA-induced silencing complex (RISC) in the cytoplasm, leading to sequence-specific mRNA cleavage [23] [12].
Research Reagent Solutions
Successful ASO experimentation requires carefully selected reagents and controls. The table below outlines essential materials and their functions.
Table 2: Essential Research Reagents for ASO Experiments
| Reagent Category | Specific Examples | Function & Application | Considerations |
|---|---|---|---|
| ASO Chemistries | Phosphorothioate (PS), 2'-O-Methoxyethyl (2'-MOE), Locked Nucleic Acid (LNA), Phosphorodiamidate Morpholino Oligomer (PMO) | Determine nuclease resistance, binding affinity, cellular uptake, and mechanism of action | PS improves stability; LNA increases affinity; PMO enables steric blockade [23] |
| Delivery Reagents | Lipid nanoparticles (LNPs), Cell-penetrating peptides (CPPs), GalNAc conjugates | Enhance cellular uptake and target tissue delivery | GalNAc conjugates enable hepatocyte-specific targeting [25] |
| Control ASOs | Scrambled sequence, Mismatch control, Sense strand control | Verify sequence-specific effects and rule out off-target impacts | Should have same length and chemistry as active ASO [23] |
| Enzymatic Assays | RNase H activity assays, Quantitative RT-PCR | Measure target reduction and mechanistic validation | Essential for gapmer ASO characterization [23] |
| Cell Culture Models | Primary cells, Immortalized lines, Patient-derived cells | Provide biologically relevant testing systems | Patient-derived cells crucial for rare disease modeling [12] |
Experimental Protocols
Protocol: In Vitro Screening of ASO Efficacy
This protocol outlines standardized methodology for initial ASO screening in cell culture systems.
Materials Required
- Synthetic ASOs (≥95% purity, desalted)
- Appropriate cell line expressing target RNA
- Transfection reagent (e.g., lipofectamine)
- Serum-free medium
- Lysis buffer for RNA extraction
- qRT-PCR reagents for target quantification
Procedure
- Cell Seeding: Plate cells in 24-well plates at 50-70% confluence 24 hours before transfection.
- ASO Preparation: Dilute ASOs to 1-10µM stock solutions in nuclease-free water.
- Complex Formation:
- Dilute ASO in serum-free medium (50µL total)
- Dilute transfection reagent separately in serum-free medium (50µL total)
- Combine diluted ASO and transfection reagent, incubate 15-20 minutes at room temperature
- Transfection:
- Add complexes dropwise to cells
- Incubate 4-6 hours at 37°C, 5% CO₂
- Replace with complete medium
- Harvesting: Collect cells 24-48 hours post-transfection for RNA analysis.
- Analysis: Extract total RNA and quantify target reduction via qRT-PCR normalized to housekeeping genes.
Key Parameters
- Include appropriate controls (scrambled ASO, untreated cells, transfection control)
- Test multiple ASOs targeting different regions of the same transcript
- Optimize ASO concentration (typically 10-100nM) and transfection conditions
- Perform dose-response and time-course experiments for lead ASOs
Protocol: Assessing Splice-Modulating ASOs
This protocol specifically addresses validation of splice-switching ASOs.
Additional Materials
- Primers flanking alternative exon
- Gel electrophoresis or capillary electrophoresis system
- RNA extraction kit with DNase treatment
- RT-PCR reagents
Procedure
- Transfection: Follow steps 1-5 from Protocol 5.1.
- RNA Extraction: Isolve total RNA using silica-membrane columns with on-column DNase digestion.
- RT-PCR:
- Perform reverse transcription with oligo(dT) or random hexamers
- Conduct PCR with primers spanning the targeted splice region
- Use limited cycle number (25-30) to maintain quantitative range
- Product Analysis:
- Separate PCR products by agarose gel or capillary electrophoresis
- Quantify band intensities to calculate exon inclusion/skipping ratios
- Validation: Confirm altered splice variants by Sanger sequencing.
Protocol: In Vivo Administration in Rodent Models
For therapeutic development, in vivo evaluation is essential. The workflow below outlines the key steps in this process.
Diagram 2: In Vivo ASO Evaluation Workflow. The process involves careful design, formulation, and administration followed by comprehensive analysis to determine therapeutic efficacy.
Materials
- Purified, sterile ASO in saline or PBS
- Animal model (e.g., transgenic mice, xenograft models)
- Appropriate injection apparatus (syringes, pumps, catheters)
- Tissue collection supplies (fixatives, frozen storage tubes)
Procedure
- Dose Preparation: Calculate ASO dose based on animal weight (typically 1-100mg/kg). Prepare fresh solutions in sterile PBS.
- Administration:
- Systemic delivery: Inject via tail vein (mice) or peripheral vein (larger animals)
- CNS delivery: Intracerebroventricular or intrathecal injection
- Local delivery: Subretinal, intramuscular, or topical application
- Dosing Regimen: Single or multiple doses depending on ASO pharmacokinetics and study objectives.
- Monitoring: Observe animals for adverse effects; monitor weight and activity.
- Tissue Collection: Harvest target tissues at predetermined timepoints; snap-freeze for molecular analysis or fix for histology.
- Analysis:
- Quantify target reduction (qRT-PCR, Western blot)
- Assess pharmacokinetics (ASO concentration in tissues)
- Evaluate phenotypic improvements (behavior, histopathology, biomarkers)
Clinical Applications and Approved Therapies
ASO therapeutics have received regulatory approval for multiple genetic disorders, demonstrating the clinical translation of this technology.
Table 3: Selected Approved ASO Therapies and Applications
| Drug Name | Target Condition | Mechanism of Action | Target Gene | Year Approved |
|---|---|---|---|---|
| Fomivirsen | CMV retinitis | RNase H-mediated degradation of viral mRNA | CMV immediate-early gene | 1998 [26] [25] |
| Mipomersen | Homozygous familial hypercholesterolemia | RNase H-mediated reduction of apoB-100 mRNA | APOB | 2013 [26] [25] |
| Eteplirsen | Duchenne muscular dystrophy | Exon skipping to restore reading frame | Dystrophin exon 51 | 2016 [26] [25] |
| Nusinersen | Spinal muscular atrophy | Exon inclusion to produce functional SMN protein | SMN2 exon 7 | 2016 [26] [25] |
| Inotersen | Hereditary transthyretin amyloidosis | RNase H-mediated reduction of mutant TTR | TTR | 2018 [26] [25] |
| Tofersen | SOD1-ALS | RNase H-mediated reduction of mutant SOD1 | SOD1 | 2023 [25] |
The clinical success of ASOs has been particularly notable for monogenic disorders with well-characterized genetic causes [12]. The approval of nusinersen for spinal muscular atrophy represented a breakthrough, demonstrating that ASOs could effectively target the central nervous system when administered intrathecally [26]. Similarly, the development of eteplirsen and subsequent exon-skipping ASOs for Duchenne muscular dystrophy established splice modulation as a viable therapeutic strategy [26].
More recently, the accelerated approval of tofersen for SOD1-associated ALS highlighted the potential of ASOs to address neurodegenerative diseases, with ongoing clinical trials investigating applications for Huntington's disease, Alzheimer's disease, and Parkinson's disease [25].
ASO technology has evolved from a conceptual framework to a robust therapeutic platform with demonstrated clinical efficacy. The continued refinement of chemical modifications, delivery strategies, and target selection promises to expand applications to additional genetic disorders. This application note provides researchers with historical context, mechanistic insights, and standardized protocols to facilitate further advancement in this rapidly evolving field. As ASO technologies continue to mature, they offer unprecedented opportunities for precise modulation of gene expression and personalized therapeutic interventions for previously untreatable genetic diseases.
Key Molecular Targets and Associated Disease Pathways
Antisense oligonucleotides (ASOs) represent a transformative class of therapeutic agents that modulate gene expression through precise Watson-Crick base pairing with target RNA sequences [23]. These synthetic single-stranded DNA or RNA molecules, typically 15-22 nucleotides in length, offer researchers and drug developers a powerful tool for investigating disease pathways and developing targeted treatments for conditions with high unmet medical need [27]. The fundamental mechanism involves ASOs binding to complementary RNA sequences, leading to gene silencing through RNase H-mediated degradation of the target RNA or through steric blockade of translation or splicing mechanisms [23]. This application note details key molecular targets, their associated disease pathways, and provides structured experimental protocols for ASO-based research.
Key Molecular Targets and Clinical Applications
ASO technology has enabled targeting of previously "undruggable" genetic pathways, particularly for rare genetic, neuromuscular, and neurodegenerative disorders [28]. The table below summarizes prominent molecular targets in ASO research and development:
Table 1: Key Molecular Targets for ASO Therapeutics
| Molecular Target | Associated Disease(s) | ASO Mechanism | Development Stage |
|---|---|---|---|
| Dystrophin gene | Duchenne Muscular Dystrophy (DMD) | Exon skipping (e.g., exon 53 skipping) to restore reading frame [28] | Clinical (WVE-N531 in development) [28] |
| Apolipoprotein(a) | Hyperlipoproteinaemia | Reduce apolipoprotein(a) production [28] | Phase III (Pelacarsen) [28] |
| SMN2 gene | Spinal Muscular Atrophy (SMA) | Splicing modulation to increase functional SMN protein [23] | Approved therapies |
| SCN2A gene | Developmental epileptic encephalopathy, channelopathies | Variant-specific suppression for seizure control [29] | Clinical trials |
| miR-122 | Hepatitis C, cancer | Inhibition of miRNA function [23] | Research/Preclinical |
| UCA1 | Various cancers | Targeting long non-coding RNA [30] | Research |
| Huntington's disease gene | Huntington's disease | Reduce mutant protein production [31] | Pipeline |
| Hereditary transthyretin (TTR) | hATTR Amyloidosis | Reduce mutant TTR production [31] | Approved therapies |
The global ASO market, valued at approximately $2.5 billion in 2025, reflects substantial investment in these targets, with anticipated growth of 15% CAGR through 2035 [31]. Current pipelines include over 170 therapeutic candidates being developed by more than 30 companies, highlighting the robust interest in this modality [31].
ASO Mechanisms of Action
ASOs employ distinct mechanisms to modulate gene expression, with the primary pathways being RNase H-mediated degradation and steric blockade:
Diagram 1: ASO Mechanisms of Action
The RNase H pathway requires a central DNA "gap" region within the ASO to form DNA-RNA heteroduplexes that recruit endogenous RNase H enzymes, leading to catalytic cleavage of the target RNA [23]. Steric-blocking ASOs, typically fully modified with high-affinity nucleotides, physically prevent cellular machinery from accessing specific RNA regions without degradation, enabling precise modulation of splicing patterns or translation initiation [23].
Chemical Modifications and Design Strategies
Optimizing ASO efficacy requires strategic chemical modifications to enhance stability, binding affinity, and cellular delivery:
Table 2: Key Chemical Modifications for ASOs
| Modification Type | Common Examples | Key Properties | Impact on RNase H Activity |
|---|---|---|---|
| Backbone | Phosphorothioate (PS) | Improved nuclease resistance, protein binding, bioavailability [23] [27] | Maintains activity |
| Sugar (2'-position) | 2'-O-methyl (2'-OMe), 2'-O-methoxyethyl (2'-MOE), 2'-Fluoro (2'-F) | Increased binding affinity, nuclease resistance [23] | Eliminates activity |
| Conformationally restricted | Locked Nucleic Acid (LNA/BNA) | Significantly increased binding affinity, nuclease resistance [23] | Eliminates activity |
| Base | 5-Methylcytosine | Increased Tm, reduced immune activation in CpG motifs [27] | Maintains activity |
Modern ASO design typically employs gapmer architectures: chimeric oligonucleotides with 2-5 modified nucleotides (e.g., LNA or 2'-MOE) on each terminus flanking a central 8-10 base DNA "gap" [23]. The modified wings enhance nuclease resistance and target affinity, while the DNA gap permits RNase H recruitment. Comparative studies demonstrate that LNA-containing gapmers show superior potency compared to 2'-MOE and 2'-OMe modifications [27].
Experimental Protocol: ASO-Mediated Gene Silencing
Protocol 1: In Vitro Screening of ASO Efficacy
Objective: Evaluate ASO-mediated knockdown of target gene expression in cell culture.
Materials:
- Synthetic ASOs (desalted or HPLC-purified)
- Appropriate cell line expressing target gene
- Transfection reagent compatible with oligonucleotides
- RT-qPCR reagents for mRNA quantification
- Western blot reagents for protein quantification
Procedure:
- ASO Design: Design 3-5 ASOs targeting different regions of the target mRNA. Include appropriate control ASOs (mismatch and scrambled sequences) [30].
- Cell Seeding: Seed cells in 24-well plates at 50-70% confluence 24 hours before transfection.
- Transfection Complex Formation:
- Dilute ASOs in serum-free medium to 2x final concentration
- Dilute transfection reagent separately in serum-free medium
- Combine diluted ASO and transfection reagent, incubate 15-20 minutes
- Treatment: Add complexes to cells at multiple concentrations (e.g., 10-100 nM) in triplicate.
- Incubation: Culture cells for 24-48 hours at 37°C, 5% CO₂.
- Analysis:
- Harvest cells for RNA isolation and RT-qPCR analysis of target mRNA levels
- Perform western blotting to assess protein level reduction
- Include appropriate housekeeping genes for normalization [30]
Validation:
- Employ at least two independent ASOs targeting different regions of the same gene
- Include mismatch controls (≥4 base mismatches) and scrambled sequence controls
- Establish dose-response curves to calculate IC₅₀ values [30]
Protocol 2: Animal Studies for ASO Efficacy
Objective: Evaluate ASO-mediated gene silencing in vivo.
Materials:
- PS-modified ASOs (HPLC-purified with Na⁺ salt exchange)
- Sterile saline for formulation
- Appropriate animal model
- Syringes/administration equipment
Procedure:
- ASO Preparation: Dissolve ASOs in sterile saline. For in vivo use, higher purity oligos are required [27].
- Dosing Regimen:
- Determine appropriate route of administration (subcutaneous, intravenous, intrathecal)
- Establish multiple dosage levels based on preliminary studies
- Include appropriate vehicle control groups
- Administration: Administer ASOs according to established schedule.
- Monitoring: Observe animals for signs of toxicity or adverse effects.
- Tissue Collection: Harvest relevant tissues at predetermined timepoints.
- Analysis:
- Quantify target mRNA reduction in tissues using RT-qPCR
- Assess protein level modulation by western blot or immunohistochemistry
- Evaluate phenotypic improvements using disease-relevant endpoints
Considerations:
- Parenteral administration (particularly subcutaneous and intravenous) predominates in clinical settings [31]
- Tissue distribution varies with ASO chemistry and administration route
- Long-term studies require careful monitoring of potential toxicities
Research Reagent Solutions
Table 3: Essential Research Reagents for ASO Experiments
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| ASO Chemistry Types | Phosphorothioate backbone, 2'-MOE, LNA, 2'-OMe | Enhance stability, binding affinity, and cellular uptake [23] [27] |
| Control Oligos | Mismatch control (≥4 base mismatches), scrambled sequence | Distinguish sequence-specific from non-specific effects [30] |
| Delivery Reagents | Cationic lipids, polymer-based transfection reagents | Facilitate cellular uptake of ASOs in vitro |
| Purification Methods | HPLC purification, standard desalt | Ensure oligo quality and reduce toxicity (essential for in vivo studies) [27] |
| Detection Assays | RT-qPCR reagents, northern blot, western blot | Quantify mRNA and protein level changes post-treatment [30] |
Experimental Workflow
A comprehensive ASO experimental program incorporates sequential validation steps:
Diagram 2: ASO Experimental Workflow
Emerging Applications and Future Directions
ASO technology continues to expand into novel therapeutic areas. Splice-switching ASOs represent a promising application, with demonstrated success in modulating splicing of the dystrophin gene in Duchenne Muscular Dystrophy to produce partially functional protein isoforms [23]. Additionally, ASOs targeting non-coding RNAs—particularly microRNAs and long non-coding RNAs—offer opportunities to modulate complex regulatory networks in oncology and other disease areas [23] [30].
The emergence of individualized ASO therapies for ultra-rare diseases (affecting single patients or small families) represents a frontier in precision medicine. Organizations like the 1 Mutation 1 Medicine (1M1M) consortium are establishing frameworks for developing patient-specific ASOs for neurological diseases, demonstrating meaningful clinical benefits even in severe, progressive disorders [29] [32].
Antisense oligonucleotides provide researchers and drug developers with a versatile platform for targeted gene modulation across diverse disease pathways. The continued refinement of ASO chemistry, design principles, and delivery strategies is accelerating the translation of this technology from basic research to clinical applications. By adhering to rigorous experimental standards—including appropriate controls, dose-response assessments, and orthogonal validation methods—scientists can reliably exploit ASO technology to investigate disease mechanisms and develop novel therapeutic interventions for conditions with significant unmet medical needs.
From Bench to Bedside: Designing, Developing, and Deploying ASO Therapeutics
Antisense oligonucleotides (ASOs) are short, synthetic nucleic acid strands designed to modulate gene expression by binding to specific RNA targets through Watson-Crick base pairing [21] [3]. Their therapeutic success fundamentally relies on chemical modifications that enhance native oligonucleotide properties, conferring resistance to nucleases, improving target affinity, and optimizing pharmacokinetic profiles [33] [34]. First-generation ASOs primarily utilized phosphorothioate (PS) backbone modifications, while subsequent generations introduced sophisticated sugar modifications including 2'-O-methyl (2'-OMe), 2'-O-methoxyethyl (2'-MOE), and phosphorodiamidate morpholino oligomers (PMO), alongside conformationally constrained nucleotides like Locked Nucleic Acid (LNA) [33] [35]. This application note provides a structured comparison of these key chemical modifications and detailed protocols for their application in gene silencing research, supporting a broader thesis on ASO therapeutic development.
Key Chemical Modifications and Properties
Table 1: Comparative properties of major ASO chemical modifications.
| Modification Type | Key Structural Feature | Mechanism Compatibility | Thermal Stability (ΔTm/mod) | Nuclease Resistance | Reported Toxicity Concerns |
|---|---|---|---|---|---|
| PS Backbone | Sulfur substitutes non-bridging oxygen | RNase H, Steric Block | Slight decrease | High | Dose-dependent; reduced vs. early generations [33] |
| 2'-OMe | 2'-O-methyl group on ribose | Steric Block only | +0.9 to +1.6°C | High | Favorable safety profile [35] |
| 2'-MOE | 2'-O-methoxyethyl group on ribose | Steric Block only | +0.9 to +1.6°C | Very High | Reduced pro-inflammatory effects [35] |
| PMO | Morpholino ring & phosphorodiamidate | Steric Block only | Similar to DNA | Very High | Unmodified PMO: Low; ivPMO-conjugates: Higher toxicity reported [36] |
| LNA | 2'-O, 4'-C methylene bridge | RNase H (in gapmers) | +4 to +8°C | Very High | Hepatotoxicity at high doses; sequence-dependent [33] |
Mechanism-Based Classification
Table 2: Guidance on modification selection based on desired mechanism of action.
| Mechanism of Action | Recommended Modification Patterns | Example ASO Drugs |
|---|---|---|
| RNase H-mediated Knockdown | Gapmer design: Central DNA/PS gap with modified flanks (2'-MOE, LNA) | Mipomersen (2'-MOE), Inotersen (2'-MOE) [35] [12] |
| Splice Switching / Steric Block | Uniform modification (2'-MOE, 2'-OMe, PMO) | Nusinersen (2'-MOE), Eteplirsen (PMO) [35] |
| siRNA (RISC-mediated) | Selective 2' modifications on sense/antisense strands | (Investigational, 2'-MOE shows promise) [35] |
Experimental Protocols for ASO Evaluation
Protocol: In Vitro Splicing Modulation Assay
Objective: Evaluate the efficacy of differently modified ASOs to modulate pre-mRNA splicing in cell culture [36].
Materials:
- Splice Reporter Vector (Midigene): Plasmid containing genomic region of target gene with splice sites of interest [36].
- Cell Line: Appropriate mammalian cells (e.g., HEK-293T, mIMCD3) [36].
- Transfection Reagent: Lipid-based (e.g., FuGENE HD) for 2'-OMe/2'-MOE/PS; Scraping method for PMOs [36].
- ASOs: Sequence-matched ASOs with different chemical modifications (2'-OMe/PS, 2'-MOE/PS, PMO) and scrambled control oligonucleotide (SON) [36].
- RNA Isolation & RT-PCR Kit: For analyzing splicing patterns.
Procedure:
- Day 1: Cell Seeding: Seed ~300,000–400,000 cells per well in a 6-well plate.
- Day 2: Midigene Transfection: Transfect 1.2 µg midigene using FuGENE HD at 3:1 reagent:DNA ratio in Opti-MEM.
- Day 3: Cell Splitting: Split transfected cells 1:6 into 12-well plates.
- Day 3: ASO Transfection:
- For 2'-OMe/PS and 2'-MOE/PS: Transfect at 0.5 µM final concentration using FuGENE HD.
- For PMOs: Use 2.5 µM final concentration in fresh medium; remove old medium, add PMO-containing medium, and gently detach cells by scraping to facilitate uptake [36].
- Day 5: Harvest and Analysis: Collect cells 48 hours post-ASO transfection.
- Isolate total RNA.
- Perform RT-PCR across the spliced region of interest.
- Analyze PCR products by gel electrophoresis or capillary electrophoresis to quantify splicing changes (e.g., exon skipping or inclusion).
Protocol: In Vivo Efficacy and Toxicity Assessment
Objective: Determine the efficacy and safety profile of modified ASOs in an animal model [36] [37].
Materials:
- Animals: Wild-type mice (e.g., C57BL/6J).
- ASOs: Chemically modified ASOs in sterile saline.
- Delivery Equipment: Micropipettes for intracerebroventricular (ICV) or intravitreal injection.
- Behavioral Analysis System: Open field test apparatus.
- Histology Reagents: Fixatives, stains for morphological analysis.
Procedure:
- ASO Administration:
- Efficacy Assessment:
- After a predetermined period (e.g., 2-4 weeks), sacrifice animals and harvest target tissues.
- Isolate RNA and protein from tissues.
- Quantify target gene expression using qRT-PCR (for RNA knockdown) or western blot (for protein reduction).
- For splice-switching ASOs, analyze RNA by RT-PCR to detect splicing modifications.
- Toxicity Assessment:
- Clinical Observation: Monitor animals externally for phenotypic changes (e.g., ocular abnormalities) [36].
- Behavioral Testing: Perform open field tests to assess acute neurotoxicity, such as changes in locomotor activity [37].
- Histological Analysis: Fix tissues, section, and stain (e.g., H&E) to evaluate morphological alterations and cellular integrity [36].
Signaling Pathways and Experimental Workflows
ASO Mechanisms of Action Pathway
Diagram Title: Primary ASO Mechanisms of Action
In Vitro to In Vivo Screening Workflow
Diagram Title: ASO Screening Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential reagents and resources for ASO research.
| Reagent/Resource | Function/Application | Example Suppliers / Notes |
|---|---|---|
| 2'-MOE-modified ASOs | Steric-blocking splice-switching ASOs; high stability & affinity | ProQR Therapeutics [36] |
| PMO Oligonucleotides | Steric-blocking applications; uncharged backbone | Gene Tools, LLC [36] |
| LNA-modified ASOs | High-affinity gapmers for potent knockdown | Exiqon, Qiagen; monitor for hepatotoxicity [33] |
| PS Backbone Reagents | Phosphoramidites for nuclease-resistant synthesis | Glen Research, ChemGenes |
| Splice Reporter Vectors | Midigene constructs for splicing assays | Custom generation via Gateway Cloning [36] |
| FuGENE HD Transfection Reagent | Lipid-based delivery of charged ASOs (2'-OMe/PS, 2'-MOE/PS) | Promega [36] |
| Scraping Method | Mechanical delivery for uncharged PMOs | Alternative to transfection reagents [36] |
The strategic selection and application of chemical modifications—including PS, PMO, LNA, and 2' modifications—are fundamental to developing ASOs with optimal efficacy and safety profiles. The protocols and comparative data provided here offer a framework for systematic evaluation of these modifications in both in vitro and in vivo settings. As the field advances, continued refinement of chemical architectures and delivery methods will expand the therapeutic potential of ASOs to target tissues beyond the liver and central nervous system, addressing an increasingly broad range of genetic disorders.
The therapeutic potential of Antisense Oligonucleotides (ASOs) and other nucleic acid therapeutics is often hampered by significant delivery challenges that must be overcome to achieve clinical efficacy. These macromolecules face numerous physiological barriers including nuclease-mediated degradation, renal clearance, inefficient cellular uptake, and entrapment within endolysosomal compartments [38] [39]. Due to their inherent properties—including high molecular weight, negative charge, and hydrophilicity—naked oligonucleotides struggle to cross biological membranes and reach their intracellular sites of action [39] [40].
To address these limitations, two primary delivery strategies have emerged: liposomal encapsulation and biomolecular conjugation. These approaches enhance the stability, bioavailability, and targeted delivery of ASOs, thereby improving their therapeutic index and expanding their potential applications in gene silencing research [38] [41]. This application note provides a structured comparison of these platforms and detailed protocols for their evaluation in preclinical research settings.
Liposomal Delivery Systems
Liposomes are spherical vesicles composed of phospholipid bilayers that can encapsulate nucleic acids, protecting them from degradation and facilitating cellular uptake. Advanced liposomal formulations, particularly lipid nanoparticles (LNPs), have become a cornerstone for systemic delivery of RNA therapeutics [38] [42]. These systems excel at encapsulating large nucleic acid payloads and can be engineered with targeting ligands for tissue-specific delivery. The first FDA-approved siRNA therapeutic, patisiran, utilizes a nanoparticle delivery system, demonstrating the clinical validity of this approach [11].
Biomolecular Conjugation Strategies
Conjugation involves the covalent attachment of biomolecules directly to oligonucleotides to enhance their pharmacokinetic properties and cellular uptake. This strategy typically results in smaller, more defined molecular entities compared to nanoparticle systems. Common conjugates include GalNAc for hepatocyte targeting, lipids for membrane interaction and improved biodistribution, and antibodies for cell-specific targeting [8] [41] [43].
Table 1: Comparison of Nucleic Acid Delivery Platforms
| Feature | Liposomal/Nanoparticle Systems | Biomolecular Conjugates |
|---|---|---|
| Size Range | 50-200 nm | Molecular (5-15 nm) |
| Typical Payload | Multiple oligonucleotides per particle | Single oligonucleotide per conjugate |
| Targeting Mechanism | Surface-functionalized with ligands | Direct ligand-receptor interaction |
| Manufacturing Complexity | High (multi-component assembly) | Medium (chemical conjugation) |
| Clinical Examples | Patisiran (LNP) | Givosiran (GalNAc-siRNA), Inclisiran (GalNAc-siRNA) |
| Primary Applications | Systemic delivery, large payloads | Targeted organ delivery (e.g., liver) |
Quantitative Analysis of Conjugation Efficacy
Recent comparative studies have provided quantitative data on the efficacy of various conjugation strategies for ASO delivery. A 2025 study systematically evaluated aptamer, vitamin E, and cholesterol conjugates of the ASO PNAT524 for cellular uptake and exon-skipping activity in cancer cell models [41]. The results demonstrated significant differences in performance between conjugation approaches.
Table 2: Efficacy Comparison of ASO Conjugation Strategies
| Conjugation Type | Exon-Skipping Efficiency | Cellular Uptake | Cytotoxic Effects | Key Characteristics |
|---|---|---|---|---|
| Unconjugated ASO | Low (baseline) | Low | Minimal | Requires transfection reagent for internalization |
| Aptamer (AS1411) | Not significant | Moderate | Minimal | Target-specific (nucleolin); limited efficacy enhancement |
| Aptamer (S2.2) | Not significant | Moderate | Minimal | Target-specific (MUC1); limited efficacy enhancement |
| Vitamin E | High, dose-dependent | High | Potent | Natural lipid; uptake via lipoprotein receptors |
| Cholesterol | Highest, dose-dependent | Highest | Most potent | Enhanced cellular uptake via LDL receptor; superior efficacy |
The cholesterol-conjugated ASO (524-Chol) demonstrated the highest efficacy in splice-modulating activity and cytotoxic outcomes, establishing cholesterol conjugation as a particularly promising strategy for enhancing ASO delivery in cancer therapeutic applications [41].
Experimental Protocol: Evaluating Cholesterol-ASO Conjugates
Conjugate Synthesis and Characterization
Materials:
- PNAT524 ASO (2'-O-methyl phosphorothioate backbone)
- Cholesterol-NHS ester or cholesterol-thiol reagents
- C6 thiol linker or triethylene glycol (TEG) linker
- Purification equipment (HPLC)
- Characterization instruments (LC-MS, MALDI-TOF)
Methodology:
- Conjugation Chemistry: Conjugate cholesterol to the 5' end of PNAT524 using a thiol linker (e.g., C6 thiol) to create 524-S-S-Chol [41].
- Purification: Purify the conjugate using reverse-phase HPLC to remove unreacted components.
- Quality Control: Verify conjugate identity and purity using LC-MS. Ensure >95% purity for cellular assays.
- Storage: Prepare stock solutions in nuclease-free water or DMSO and store at -20°C.
Cellular Uptake and Efficacy Assessment
Materials:
- Cancer cell lines relevant to research goals (e.g., HeLa, A549)
- Fluorescence microscope with appropriate filters
- qRT-PCR equipment and reagents
- Cell viability assay kits (MTT, CCK-8)
- Serum-free cell culture media
Methodology:
- Cell Seeding: Plate cells in 24-well plates at 5×10⁴ cells/well and culture for 24 hours.
- Treatment Application:
- Prepare serial dilutions of cholesterol-ASO conjugates in serum-free medium (e.g., 10 nM to 1 μM).
- Apply treatments to cells and incubate for 24-48 hours.
- Include untransfected ASO controls and vehicle controls.
- Uptake Analysis:
- For fluorescently labeled ASOs, fix cells after treatment and image using fluorescence microscopy.
- Quantify fluorescence intensity using image analysis software.
- Functional Assessment:
- Extract total RNA and perform qRT-PCR to measure target mRNA levels.
- Analyze exon-skipping efficiency using RT-PCR with flanking primers.
- Viability Assessment:
- Perform cell viability assays (e.g., MTT) according to manufacturer protocols.
- Calculate IC₅₀ values for cytotoxic effects.
Intracellular Trafficking and Mechanism of Action
Understanding the cellular fate of delivered ASOs is crucial for optimizing delivery strategies. Both liposomal and conjugate-based systems must overcome the endosomal barrier to release ASOs into the cytoplasm and allow translocation to the nucleus for certain mechanisms of action.
Key Mechanisms:
- Liposomal Systems: Employ pH-sensitive or fusogenic lipids that disrupt endosomal membranes through the proton sponge effect or membrane fusion [38] [42].
- Cholesterol Conjugates: Enhance uptake through LDL receptor-mediated endocytosis and may promote endosomal escape through hydrophobic interactions with membranes [41].
- GalNAc Conjugates: Utilize the asialoglycoprotein receptor (ASGPR) on hepatocytes for highly efficient receptor-mediated endocytosis [8] [11].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for ASO Delivery Research
| Reagent/Category | Specific Examples | Function/Application | Research Notes |
|---|---|---|---|
| Lipid Nanoparticles | Ionizable lipids (DLin-MC3-DMA), Phospholipids, Cholesterol, PEG-lipids | ASO encapsulation and protection; enhances cellular uptake and biodistribution | Optimal N:P ratio critical for efficiency; PEG content affects circulation time |
| Conjugation Ligands | GalNAc, Cholesterol, Vitamin E (α-tocopherol), Antibodies | Targeted delivery; improved cellular uptake and pharmacokinetics | Linker choice (TEG, C6 thiol) affects release and activity |
| Chemical Modifications | Phosphorothioate (PS), 2'-O-methyl (2'-OMe), Locked Nucleic Acid (LNA) | Enhanced nuclease resistance; improved binding affinity; reduced immunogenicity | LNA modifications require careful design to minimize hepatotoxicity |
| Cell Lines | HepG2 (hepatocytes), HeLa (epithelial), patient-derived organoids | In vitro modeling of ASO uptake and activity | Primary cells or 3D models may better recapitulate in vivo conditions |
| Analytical Tools | LC-MS/MS, fluorescence microscopy, qRT-PCR, flow cytometry | Quantification of ASO uptake, distribution, and functional activity | LC-MS/MS offers specificity for parent vs. metabolite differentiation |
Protocol for Lipid Nanoparticle Formulation and Testing
Microfluidic LNP Preparation
Materials:
- Ionizable lipid (e.g., DLin-MC3-DMA)
- Helper lipids (DSPC, cholesterol)
- PEG-lipid (DMG-PEG2000)
- ASO in citrate buffer (pH 4.0)
- Ethanol (100%)
- Microfluidic device (NanoAssemblr, staggered herringbone mixer)
Methodology:
- Lipid Solution Preparation: Dissolve ionizable lipid, DSPC, cholesterol, and PEG-lipid in ethanol at specific molar ratios (50:10:38.5:1.5).
- Aqueous Phase Preparation: Dilute ASO in citrate buffer (pH 4.0) to 0.2 mg/mL.
- Mixing Procedure:
- Set total flow rate to 12 mL/min with aqueous:organic flow rate ratio of 3:1.
- Use microfluidic device to rapidly mix aqueous and organic phases.
- Collect resulting LNP suspension.
- Dialyze against PBS (pH 7.4) for 2 hours to remove ethanol.
- Characterize particle size (Zetasizer), polydispersity index, encapsulation efficiency (RiboGreen assay).
In Vivo Biodistribution Study
Materials:
- Fluorescently labeled ASO (Cy5, Cy7)
- Animal model (mice, rats)
- IVIS imaging system
- Tissue homogenization equipment
Methodology:
- Dose Administration: Inject fluorescent ASO-LNPs via tail vein (dose: 1-5 mg ASO/kg).
- Time Points: Image animals at 1, 4, 24, and 48 hours post-injection.
- Ex Vivo Analysis:
- Euthanize animals at endpoint.
- Collect tissues (liver, spleen, kidney, lung).
- Image excised tissues using IVIS.
- Homogenize tissues and quantify ASO content using LC-MS/MS or fluorescence measurement.
- Data Analysis: Calculate percentage of injected dose per gram of tissue (%ID/g).
The parallel development of liposomal systems and biomolecular conjugates provides researchers with complementary tools for overcoming biological barriers to ASO delivery. While liposomal formulations offer versatility for systemic administration and complex payloads, conjugate strategies provide precise targeting and favorable pharmacokinetic profiles with simpler manufacturing requirements [38] [8] [41].
Emerging directions in the field include the development of antibody-oligonucleotide conjugates (AOCs) that combine cell-specific targeting with potent gene regulation [43], non-cationic delivery systems with improved safety profiles [40], and advanced formulation techniques that enhance stability and tissue penetration. As these technologies mature, they will expand the therapeutic landscape for ASOs, enabling treatment of previously undruggable targets across a broader range of tissues and diseases.
The protocols and comparative data presented herein provide a foundation for researchers to systematically evaluate and optimize ASO delivery strategies for their specific applications in gene silencing research.
Antisense oligonucleotides (ASOs) are short, synthetic nucleic acids designed to bind complementary RNA sequences through Watson-Crick base pairing, modulating gene expression through mechanisms including RNase H-mediated degradation, translational arrest, or splicing modulation [23] [12]. The rational design of ASOs has been revolutionized by computational approaches that significantly enhance the efficiency and precision of screening processes, reducing reliance on extensive experimental trial-and-error [44] [45]. This application note details established in silico protocols for designing and screening ASOs, providing researchers with structured methodologies to accelerate therapeutic development.
Computational Tools for ASO Design and Screening
Advanced computational tools enable the prediction of ASO efficacy based on target sequence analysis, energy calculations, and machine learning models. The table below summarizes core platforms for ASO design.
Table 1: Key Computational Tools for ASO Design and Screening
| Tool Name | Primary Application | Key Parameters | Access |
|---|---|---|---|
| eSkip-Finder [45] | Predicts exon-skipping efficacy | ASO sequence, target motifs, skipping efficacy score | Web server |
| Sfold [44] | Designs siRNAs & antisense oligos | Binding energy, GC content, target accessibility | Web server |
| Molecular Docking (Schrödinger PIPER) [44] | Models ASO-mRNA interactions | Binding affinity (kcal/mol), interaction mapping | Commercial software |
| n-Lorem Algorithm [46] | Designs RNase H1-activating gapmers | Sequence motifs, mismatch tolerance, off-target potential | Proprietary platform |
Quantitative Design Parameters
Successful in silico design requires optimization of several physicochemical and thermodynamic parameters. Based on analyses of effective ASOs, the following quantitative thresholds guide candidate selection:
Table 2: Key Quantitative Parameters for Optimal ASO In Silico Selection
| Parameter | Optimal Range | Rationale | Calculation Method |
|---|---|---|---|
| Binding Affinity (ΔG) [44] | ≤ -8 kcal/mol | Stronger hybridization indicated by more negative values | Weighted sum of DNA/RNA stacking energies |
| GC Content [44] | 30-60% | Balances affinity and specificity; extremes can promote non-specific binding | Percentage of Guanine and Cytosine nucleotides |
| Sequence Length [23] [46] | 16-20 nucleotides | Sufficient for specificity while maintaining cellular uptake and efficiency | Number of nucleotides in the ASO |
| Target Accessibility [45] | Low local folding energy | Prefers single-stranded, accessible mRNA regions to facilitate binding | Calculated from mRNA secondary structure prediction |
Experimental Protocols
Protocol 1: Initial Sequence Screening and Selection for Transcript Knockdown
This protocol utilizes the Sfold software to identify optimal ASO sequences for RNase H1-mediated degradation [44].
3.1.1 Materials and Reagents
- Target mRNA Sequence: in FASTA format (e.g., from NCBI GenBank).
- Sfold Web Server: Accessible at
http://sfold.wadsworth.org/[44]. - Computer Workstation: Standard modern computer capable of running bioinformatics software.
3.1.2 Procedure
- Input Preparation: Retrieve the complete mRNA sequence of the target gene, including 5' and 3' untranslated regions (UTRs), from a database such as NCBI GenBank.
- Software Submission: Input the target sequence into the Sfold Soligo module.
- Parameter Setting:
- Set the desired ASO length (typically 16-20 mer).
- Define parameters to avoid problematic sequence motifs (e.g., GGGG runs, CpG dinucleotides) [46].
- Analysis Execution: Run the software to generate a list of candidate ASOs.
- Candidate Filtering:
- Select ASOs with a calculated binding energy of ≤ -8 kcal/mol [44].
- Filter candidates based on GC content (30-60%).
- Cross-reference candidate sequences against transcriptome databases (e.g., BLAST) to minimize off-target binding, allowing no more than two central mismatches in any non-target RNA [46].
Protocol 2: Predicting and Selecting Exon-Skipping ASOs
This protocol employs eSkip-Finder to design splice-switching ASOs (ssASOs) for modulating pre-mRNA splicing [45].
3.2.1 Materials and Reagents
- Pre-mRNA Target Sequence: encompassing the exon and flanking intronic regions.
- eSkip-Finder Web Server: Publicly accessible online tool.
3.2.2 Procedure
- Target Definition: Identify the specific exon targeted for skipping and obtain its genomic context.
- Tool Utilization:
- Input the target sequence into eSkip-Finder.
- Specify the desired ASO length as per experimental requirements.
- Efficacy Prediction: Run the tool to obtain a ranked list of candidate ASO sequences based on predicted exon-skipping efficacy.
- Sequence Selection: Prioritize ASOs predicted with high skipping efficacy scores for experimental validation.
Protocol 3: Molecular Docking for ASO-mRNA Interaction Analysis
This protocol uses molecular docking to visualize and quantify the interaction between a designed ASO and its target mRNA, providing a structural basis for efficacy [44].
3.3.1 Materials and Reagents
- 3D Structure of Target mRNA: Predicted using tools like mfold or other RNA modeling software.
- 3D Structure of ASO: Modeled as a single-stranded nucleic acid.
- Molecular Docking Software: Such as the PIPER module in Schrödinger.
3.3.2 Procedure
- Structure Preparation:
- Predict the secondary structure of the target mRNA using mfold under physiological ionic conditions [44].
- Generate the 3D structure of the mRNA from the secondary structure.
- Model the 3D structure of the candidate ASO.
- Docking Setup: Prepare both structures for docking, ensuring correct protonation states.
- Docking Execution: Perform protein-protein docking using PIPER to simulate the ASO-mRNA interaction.
- Interaction Analysis:
- Analyze the resulting complexes for binding affinity (kcal/mol). Values around -10 kcal/mol indicate strong binding [44].
- Visually inspect the docking poses to confirm hybridization at the intended target site.
Workflow Visualization
Diagram 1: Computational ASO screening workflow. This diagram outlines the sequential steps for the in silico screening of ASOs, from target identification to the selection of lead candidates for experimental testing.
Diagram 2: Primary ASO mechanisms of action. This diagram illustrates the two main mechanistic pathways for ASOs: the RNase H1-dependent degradation of target mRNA by gapmer ASOs and the modulation of pre-mRNA splicing by steric-blocking splice-switching ASOs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for ASO Screening
| Item | Function/Application | Example/Notes |
|---|---|---|
| Target mRNA Sequence | Serves as the input for in silico design | Retrieved from NCBI GenBank (e.g., NM_001278599.2 for AXL gene) [44] |
| Chemically Modified ASO Libraries | Experimental validation of in silico predictions | Phosphorothioate (PS) backbones; 2'-MOE, LNA, or PMO modifications [23] [12] |
| Patient-Derived Cells / iPSCs | Physiologically relevant in vitro screening | Confirm ASO potency and assess toxicity in a human genetic context [47] [46] |
| qPCR/ddPCR Reagents | Quantifying target mRNA knockdown | Optimize primers, probes, and housekeeping genes for sensitive detection [47] |
| BJAB Cell Line | Screening for potential immunotoxicity | Identifies ASOs that may activate the innate immune system [46] |
| High-Content Imaging Systems | Multiplexed efficacy and toxicity readouts | Quantify protein-level changes and cellular health markers [47] |
The integration of sophisticated computational tools like Sfold, eSkip-Finder, and molecular docking platforms into the ASO development pipeline provides an efficient and rational framework for candidate screening. By adhering to the detailed protocols and optimal parameters outlined in this document, researchers can significantly enhance the precision of initial ASO selection, thereby accelerating the development of promising therapeutic candidates and reducing costly late-stage failures.
Antisense oligonucleotides (ASOs) represent a transformative class of gene-silencing therapeutics that have redefined treatment paradigms for previously untreatable genetic disorders. These short, synthetic single-stranded DNA or RNA molecules modulate gene expression through precise, sequence-specific binding to target RNA transcripts [4] [48]. The successful clinical translation of ASOs marks a milestone in precision medicine, offering life-changing interventions for rare monogenic diseases with significant unmet needs. This application note details the clinical success stories, indications, and experimental protocols for key FDA/EMA-approved ASO therapies, providing drug development professionals with essential methodological frameworks for their research.
Approved ASO Therapies: Clinical Indications and Outcomes
Table 1: FDA/EMA-Approved ASO Therapies and Their Clinical Applications
| ASO Name (Generic) | Brand Name | Target Gene | Indication | Year Approved | Key Clinical Outcome | Mechanism of Action |
|---|---|---|---|---|---|---|
| Nusinersen | Spinraza | SMN2 | Spinal Muscular Atrophy (SMA) | 2016 | Improved motor function, survival in infants [4] | Splice-switching (Exon 7 inclusion) [4] |
| Tofersen | Qalsody | SOD1 | SOD1-ALS | 2023 | Reduced neurofilament light (biomarker) [8] | RNase H-mediated degradation [4] |
| Inotersen | Tegsedi | TTR | Hereditary Transthyretin Amyloidosis | 2018 | Improved neuropathy, quality of life [8] | RNase H-mediated degradation [4] |
| Eplontersen | Wainua | TTR | Hereditary Transthyretin Amyloidosis | 2023 | - [8] | RNase H-mediated degradation |
| Mipomersen | Kynamro | ApoB-100 | Homozygous Familial Hypercholesterolemia | 2013 | Reduced LDL-C [8] | RNase H-mediated degradation |
Table 2: Notable Investigational ASOs in Advanced Clinical Development (2025)
| ASO Name | Target Gene | Indication | Development Status (2025) | Key Reported Outcome |
|---|---|---|---|---|
| Ulefnersen (jacifusen) | FUS | FUS-ALS | Phase 3 Trial | Functional recovery; 83% decrease in neurofilament light [49] [50] |
| Donidalorsen | KLKB1 (Prekallikrein) | Hereditary Angioedema (HAE) | NDA Accepted (PDUFA 2025) | >90% reduction in attack rate [51] |
Detailed Clinical Success Stories
Nusinersen for Spinal Muscular Atrophy (SMA)
Spinal Muscular Atrophy (SMA), a devastating autosomal recessive disorder, is primarily caused by biallelic loss-of-function variants in the SMN1 gene, leading to a deficiency of survival motor neuron (SMN) protein [4]. Nusinersen, the first FDA-approved ASO for this disease, targets the paralogous SMN2 gene. Underlying pathomechanism involves alternative splicing that predominantly excludes exon 7, producing a truncated, non-functional SMN protein [4].
- Mechanism of Action: As a splice-switching ASO (SSO), nusinersen binds to a specific regulatory sequence within intron 7 of SMN2 pre-mRNA. This binding sterically blocks the association of splicing repressors, thereby promoting the inclusion of exon 7 in the mature mRNA transcript [4].
- Clinical Impact: This intervention enables the production of full-length, functional SMN protein, restoring motor neuron function and dramatically slowing disease progression. Nusinersen administration requires intrathecal injection to bypass the blood-brain barrier, leveraging the slow clearance of ASOs from the cerebrospinal fluid [4]. Its success laid the foundational delivery strategy for subsequent neurological ASO therapies.
Ulefnersen for FUS-Amyotrophic Lateral Sclerosis (ALS)
Mutations in the FUS gene cause one of the most aggressive forms of ALS, representing 1-2% of all cases and often affecting adolescents and young adults [49] [50]. These mutations lead to the accumulation of toxic FUS proteins within motor neurons, resulting in rapid cell death [50].
- Clinical Evidence: A 2025 case series published in The Lancet detailed unprecedented outcomes in patients treated with the investigational ASO ulefnersen. One young female patient, treated since late 2020, regained the ability to walk unaided and breathe without a ventilator, achieving the longest known survival for this juvenile-onset form of FUS-ALS [49] [50]. An asymptomatic male patient with a strong family history and abnormal electrophysiological findings has remained symptom-free after three years of preventive treatment [49] [50].
- Biomarker Response: Across the cohort, treatment resulted in up to an 83% decrease in neurofilament light chain, a key biomarker of nerve damage, confirming the therapy's biological activity [49] [50].
- Mechanism: Ulefnersen is an allele-selective gapmer ASO designed to silence the FUS gene and reduce the production of the toxic protein [4] [50].
The diagram below illustrates the mechanistic pathway of ASO-mediated gene silencing for FUS-ALS.
Milasen and the Dawn of N-of-1 Therapies
The case of milasen exemplifies the ultimate personalization of ASO therapy. Milasen was developed for a single patient, Mila Makovec, who was diagnosed with a rare, fatal form of Batten disease (neuronal ceroid lipofuscinosis, CLN7) caused by a unique deep intronic pathogenic variant in the MFSD8 gene [4] [52]. This variant caused the inclusion of a pseudo-exon, leading to a loss-of-function protein [4].
- Drug Development Timeline: From genome sequencing to initial treatment, milasen was developed and administered in under one year, showcasing the remarkable speed of personalized ASO development [52].
- Mechanism: Milasen is a splice-switching ASO designed to bind the cryptic exon recognition sequence within MFSD8 pre-mRNA. By sterically blocking the spliceosome machinery, it prevents the inclusion of the pseudo-exon, restoring proper splicing and production of functional MFSD8 protein [4].
- Outcome: While not a cure, treatment with milasen slowed the progression of Mila's neurodegenerative disease, providing a profound proof-of-concept for ultra-rare, individualized genetic therapies [52].
Essential Experimental Protocols for ASO Research
Protocol: In Vitro Screening for ASO Candidate Selection
Objective: To identify the most potent and specific ASO lead candidates for further development by assessing their efficacy in target cell models.
Materials:
- Research Reagent Solutions:
- Synthetic ASO Library: A panel of 5-20 ASOs (typically 16-20 mer) targeting different regions of the pre-mRNA/mRNA, with phosphorothioate (PS) backbones and 2'-O-methoxyethyl (2'-MOE) or other modifications [4] [48].
- Cell Line Models: Patient-derived fibroblast/lymphoblastoid cells or engineered cell lines expressing the target gene/mutation [4].
- Transfection Reagent: Lipofectamine 3000 or other cationic lipid-based transfection agents suitable for oligonucleotide delivery.
- Lysis Buffer: Commercially available RNA/DNA/Protein co-extraction kits (e.g., TRIzol).
- qRT-PCR Assay Kits: For quantifying target RNA levels and splicing changes.
- Western Blot Systems: Antibodies against the target protein and a loading control (e.g., GAPDH).
Procedure:
- Cell Seeding: Plate cells in 24-well or 48-well plates at an optimal density (e.g., 5 x 10⁴ cells/well) and culture until they reach 60-80% confluency.
- ASO Transfection: Transfect cells with individual ASO candidates (e.g., 10-100 nM range) using the appropriate transfection reagent. Include a scrambled sequence ASO as a negative control and a positive control if available.
- Incubation: Incubate cells for 24-48 hours post-transfection to allow for sufficient target engagement and degradation/splicing modulation.
- RNA/Protein Harvest: Lyse cells to simultaneously isolate total RNA and protein.
- Efficacy Analysis:
- For Gapmers (RNase H1-dependent): Perform qRT-PCR to measure the reduction in target mRNA levels relative to the control ASO [4].
- For Splice-Switching ASOs: Design qRT-PCR assays or perform RT-PCR with gel electrophoresis to detect and quantify changes in splicing isoforms (e.g., exon inclusion/exclusion) [4].
- Confirm Protein Knockdown/Correction: Perform Western blot analysis to measure changes in target protein expression.
- Data Analysis: Normalize data to housekeeping genes/proteins. Select 2-3 lead candidates showing the highest potency and lowest half-maximal inhibitory concentration (IC₅₀) for subsequent in vivo testing.
Protocol: Bioanalytical Method for ASO Quantification in Plasma
Objective: To accurately measure the concentration of ASO therapeutics in biological matrices (e.g., plasma, CSF) during pharmacokinetic (PK) studies using Liquid Chromatography-Mass Spectrometry (LC-MS) [8].
Materials:
- Research Reagent Solutions:
- Internal Standard (IS): A stable isotope-labeled analog of the ASO of interest.
- Solid-Phase Extraction (SPE) Kit: Anion-exchange or mixed-mode SPE cartridges for oligonucleotide purification.
- LC-MS/MS System: Liquid chromatography system coupled to a triple quadrupole mass spectrometer.
- Mobile Phases: A) Hexafluoroisopropanol (HFIP) with Triethylamine (TEA) in water; B) Methanol. These are critical for optimal oligonucleotide separation.
Procedure:
- Sample Preparation: Precipitate proteins from plasma/CSF samples (e.g., 50-100 µL) by adding a mixture of methanol and IS. Centrifuge and collect the supernatant.
- Solid-Phase Extraction (SPE): Load the supernatant onto a pre-conditioned SPE cartridge. Wash with appropriate buffers to remove impurities. Elute the ASO with a volatile salt solution in an organic solvent mixture.
- LC-MS/MS Analysis:
- Chromatography: Separate the ASO on a reversed-phase column (e.g., C18) using a gradient of the HFIP/TEA mobile phase and methanol. This removes salts and endogenous interference.
- Mass Spectrometry Detection: Use negative-ion electrospray ionization (ESI-) and Multiple Reaction Monitoring (MRM) to detect and quantify the ASO and its IS based on their unique mass-to-charge (m/z) transitions [8].
- Quantification: Generate a standard curve using blank matrix spiked with known concentrations of the ASO. Calculate the concentration of the ASO in unknown samples by comparing the peak area ratio (ASO/IS) to the standard curve. The Lower Limit of Quantification (LLOQ) for modern LC-MS methods can reach sub-ng/mL levels [8].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for ASO Research & Development
| Research Reagent | Function/Application in ASO R&D |
|---|---|
| Phosphorothioate (PS) Backbone | First-generation modification; increases nuclease resistance and prolongs half-life; promotes protein binding which can aid tissue distribution but may contribute to toxicity [48]. |
| 2'-MOE/2'-OMe Modifications | Second-generation sugar modifications; enhance binding affinity to RNA, improve nuclease resistance, and reduce pro-inflammatory side effects compared to first-generation ASOs [48]. |
| Locked Nucleic Acid (LCA) | High-affinity RNA analog; increases thermal stability (Tm) of the ASO-RNA duplex, improving potency and allowing for shorter ASO sequences [52]. |
| GalNAc Conjugation | Triantennary N-acetylgalactosamine ligand; enables highly efficient receptor-mediated uptake into hepatocytes via the asialoglycoprotein receptor (ASGPR), revolutionizing liver-targeted ASO therapy [51] [8]. |
| Cationic Lipid Transfection Agents | Form complexes with negatively charged ASOs to facilitate cellular uptake in in vitro assays for initial candidate screening [8]. |
| LC-MS/MS Bioanalytical Platforms | Gold-standard method for the specific and sensitive quantification of ASOs and their metabolites in complex biological matrices during PK/PD studies [8]. |
The documented clinical successes of ASOs, from nusinersen to the personalized therapy milasen, validate their profound potential to address the root cause of genetic diseases. The ongoing clinical development of drugs like ulefnersen for FUS-ALS and donidalorsen for HAE signals a rapidly expanding frontier [49] [51]. The experimental frameworks and tools detailed herein provide a foundational roadmap for researchers aiming to advance new ASO candidates. As chemical modifications and delivery technologies continue to evolve, the scope of ASO therapeutics is poised for significant growth, solidifying their role as a cornerstone of precision genetic medicine.
Application Notes
Antisense oligonucleotides (ASOs) are short, synthetic DNA or RNA strands designed to bind complementary target RNA sequences, modulating gene expression through various mechanisms such as RNA degradation or splice modulation [53] [54]. Their versatility enables precise targeting of disease-causing genes, making them powerful tools for treating rare genetic disorders, neurodegenerative diseases, and cancers, including those once considered "undruggable" [55] [56].
Rare Monogenic Diseases
ASOs are particularly suited for rare monogenic diseases, approximately 85% of which are caused by mutations in a single gene [57]. The therapeutic strategy is chosen based on the disease's underlying pathological mechanism: loss-of-function (LoF) or gain-of-function (GoF) [12].
- For GoF Mutations: Knockdown approaches using gapmer ASOs or siRNAs are employed to reduce the levels of toxic proteins [55] [12]. For example, in TUBB4A-related leukodystrophies like H-ABC, a ASO is designed to silence the mutant TUBB4A gene, reducing the production of the toxic protein that disrupts myelin formation in the brain. Preclinical models show this not only reduces toxic protein levels but can also reverse some symptoms [58] [57].
- For LoF Mutations: Splice-switching ASOs (ssASOs) can restore functional protein production. The pioneering example is nusinersen for spinal muscular atrophy (SMA). It targets the SMN2 pre-mRNA to promote the inclusion of exon 7, resulting in increased production of full-length, functional survival motor neuron (SMN) protein [55] [59].
A critical consideration is that not all genetic disorders are amenable to ASO therapy. Factors such as the target tissue, delivery route, and timing of intervention are crucial for success, as some symptoms may cause irreversible damage if treatment is initiated too late [12] [57].
Oncology
In oncology, ASOs provide a strategy to target oncogenes that have been resistant to small-molecule drugs [55]. A prominent target is the KRAS oncogene, which is mutated in over 90% of pancreatic cancers and many lung and colorectal cancers [56].
- Novel Combination Therapy: A breakthrough approach involves combining a KRAS-targeting ASO with an immunomodulatory RNA (immRNA) agonist for the RIG-I pathway. The ASO silences the mutant KRAS gene, while the immRNA activates the innate immune system [56].
- Mechanism and Outcome: This dual-action simultaneously inhibits oncogenic driving and stimulates an immune response against the tumor. It converts immunologically "cold" tumors into "hot" ones, enabling the immune system to recognize and attack the cancer. In preclinical models of pancreatic ductal adenocarcinoma (PDAC), this therapy suppressed tumor growth, limited metastasis, and extended survival without observable toxicity [56].
- Delivery System: This combination therapy utilizes red blood cell-derived extracellular vesicles (RBCEVs) as a natural, biocompatible carrier, enabling targeted delivery and overcoming historical barriers to nucleic acid delivery in cancer [56].
Neurodegenerative Disorders
The ability of ASOs to target the root cause of diseases at the RNA level makes them a promising therapeutic option for neurodegenerative disorders [59]. Multiple ASOs are in preclinical and clinical development for conditions such as Amyotrophic Lateral Sclerosis (ALS), Huntington's disease, Alzheimer's disease, and Parkinson's disease [59] [57]. For instance, ASOs are in trials to target the production of the Tau protein in Alzheimer's disease [58] [57].
- Challenge of Neurotoxicity: A significant challenge for CNS-applied ASOs is neurotoxicity, which can be acute or late-onset [60]. Late-onset neurotoxicity involves a different mechanism, characterized by the abnormal aggregation of paraspeckle proteins and activation of p53-related cell death pathways, leading to neuronal cell death days after administration [60].
- Mitigation Strategy: Recent research indicates that specific chemical modifications in the gap region of gapmer ASOs can mitigate this toxicity. The 5'-CP modification was found to prevent aberrant protein interactions and protect against late-onset neurotoxicity while maintaining target gene knockdown activity. Replacing phosphorothioate (PS) bonds with phosphodiester (PO) bonds in the ASO backbone further enhanced the safety profile by maintaining efficacy and reducing toxic side effects [60].
Table 1: Clinical and Preclinical Applications of ASOs
| Disease Area | Target / Indication | ASO Therapeutic (Examples) | Mechanism of Action | Development Stage / Key Outcome |
|---|---|---|---|---|
| Rare Disease | SMN2 in Spinal Muscular Atrophy | Nusinersen (Spinraza) | Splice-switching (exon 7 inclusion) | FDA approved (2016); improved motor milestones and survival [55] [61] |
| Rare Disease | TUBB4A in H-ABC Leukodystrophy | SynaptixBio ASO (proprietary) | Transcript knockdown (gapmer) | Preclinical; reduced toxic protein, symptom reversal in mice [58] [57] |
| Oncology | Mutant KRAS in Pancreatic, Lung, Colorectal Cancer | KRAS ASO + RIG-I immRNA | Transcript knockdown + Immune activation | Preclinical; reduced tumor burden, extended survival, no toxicity [56] |
| Neurodegenerative | TTR in Amyloidosis | Eplontersen | Not Specified | Phase III (positive interim results) [61] |
| Neurodegenerative | Tau protein in Alzheimer's | UCLH trial ASO (investigational) | Transcript knockdown | Clinical Trials [58] [57] |
Experimental Protocols
Protocol 1: In Vivo Combination ASO-immunotherapy for KRAS-Mutant Cancers
This protocol outlines a therapeutic strategy for KRAS-mutant cancers using a combination of ASOs and an immunomodulatory RNA, delivered via extracellular vesicles [56].
- Objective: To evaluate the efficacy and safety of a combined KRAS-targeting ASO and RIG-I agonist therapy in preclinical models of pancreatic ductal adenocarcinoma (PDAC).
Materials:
- Research Reagent Solutions:
- ASOs: Chemically modified gapmer ASOs designed to target and silence mutant KRAS mRNA sequences via RNase H1-mediated degradation [55] [56].
- Immunomodulatory RNA (immRNA): RNA molecules designed to activate the RIG-I immune pathway, triggering an interferon response [56].
- Red Blood Cell-Derived Extracellular Vesicles (RBCEVs): Biocompatible natural carriers used for the co-delivery of ASO and immRNA [56].
- KRAS-mutant cancer cell lines: Including pancreatic (e.g., PANC-1), colorectal, and lung cancer lines.
- Animal model: Immunocompromised or humanized mouse models with subcutaneous or orthotopic KRAS-mutant tumors [56].
- Patient-derived organoids (PDOs): For ex vivo validation of therapy response [56].
- Research Reagent Solutions:
Methodology:
- Therapeutic Formulation:
- Load the KRAS-targeting ASO and RIG-I-activating immRNA separately into RBCEVs using an established method like electroporation.
- Purify and characterize the loaded EVs for size, concentration, and nucleic acid loading efficiency.
- In Vitro Validation:
- Treat a panel of KRAS-mutant cancer cells with the ASO-immRNA-EV formulation.
- Assess KRAS mRNA and protein knockdown via qRT-PCR and Western blot.
- Measure immune activation by analyzing interferon-stimulated gene (ISG) expression.
- Evaluate cell viability and immunogenic cell death markers (e.g., ATP release, calreticulin exposure).
- In Vivo Efficacy:
- Administer the formulation systemically (e.g., via intravenous injection) to mouse models bearing established KRAS-mutant tumors.
- Monitor tumor volume regularly using caliper measurements or in vivo imaging.
- Analyze survival outcomes in treated versus control groups.
- Immune Monitoring and Histology:
- At endpoint, harvest tumors and analyze the tumor immune microenvironment by flow cytometry (e.g., for T-cell infiltration) and immunohistochemistry.
- Assess for any signs of toxicity in major organs (e.g., liver, spleen) through histopathological examination.
- Therapeutic Formulation:
Table 2: Key Research Reagent Solutions for ASO-based Experiments
| Reagent / Material | Function / Role in Experiment |
|---|---|
| Gapmer ASOs | Single-stranded ASOs with a DNA core flanked by modified nucleotides; designed to induce RNase H1-mediated degradation of complementary target RNA [55] [12]. |
| Splice-Switching ASOs (ssASOs) | Single-stranded ASOs that bind to pre-mRNA and modulate splicing by blocking splice-regulatory elements, leading to exon inclusion or exclusion [55] [12]. |
| Lipid Nanoparticles (LNPs) | A delivery system used to encapsulate and protect oligonucleotides, facilitating cellular uptake and endosomal escape [55] [61]. |
| GalNAc Conjugates | A targeted delivery system where ASOs are conjugated to N-acetylgalactosamine, enabling highly specific uptake by hepatocytes via the asialoglycoprotein receptor [55]. |
| Phosphorothioate (PS) Backbone | A first-generation chemical modification where a sulfur atom replaces a non-bridging oxygen in the phosphate backbone, increasing nuclease resistance and protein binding for improved pharmacokinetics [54]. |
| 2'-O-methoxyethyl (2'-O-MOE) | A sugar modification that increases binding affinity to target RNA and provides resistance to nucleases, often used in the "wings" of gapmer designs [54]. |
| Red Blood Cell-Derived EVs (RBCEVs) | A natural, biocompatible vesicle system used for the targeted delivery of nucleic acid therapeutics, offering a potential safety advantage over synthetic carriers [56]. |
Protocol 2: Evaluating and Mitigating ASO-Induced Neurotoxicity
This protocol describes methods to assess late-onset neurotoxicity of CNS-targeting ASOs and validate chemical modifications that mitigate it [60].
- Objective: To screen ASO candidates for late-onset neurotoxicity and confirm the safety-enhancing effect of 5'-CP and PO bond modifications in preclinical models.
- Materials:
- Research Reagent Solutions:
- Test ASOs: Gapmer ASOs with varying chemical modifications (e.g., standard 2'-OMe, 5'-CP, PS vs. PO backbone).
- Control ASOs: A known neurotoxic ASO and a non-toxic control ASO.
- Animal model: Wild-type mice for intracerebroventricular (ICV) or intrathecal injection.
- Primary neuronal cultures: For in vitro mechanistic studies.
- Research Reagent Solutions:
- Methodology:
- In Vivo Toxicity Screening:
- Administer a single dose of each test ASO to mice via the intended CNS delivery route (e.g., ICV injection).
- Monitor animals daily for at least 14 days for behavioral signs of neurotoxicity, such as hypoactivity, motor deficits, and reduced consciousness.
- Compare the time of onset and duration of symptoms between ASOs with different chemical modifications.
- Histopathological and Biochemical Analysis:
- After the observation period, euthanize the animals and perfuse-fix the brains.
- Process brain tissue for histological analysis (e.g., H&E staining) to assess neuronal cell death in regions like the hippocampus and cortex.
- Perform immunohistochemistry or Western blotting for markers of p53 activation and paraspeckle protein (e.g., NONO, SFPQ) mislocalization.
- Efficacy Confirmation:
- In parallel groups, confirm that the modified ASOs (e.g., with 5'-CP) retain their gene-silencing activity against the intended target in the brain by measuring target mRNA and protein levels.
- In Vitro Mechanistic Confirmation:
- Treat primary neuronal cultures with the ASOs.
- Use immunofluorescence to visualize the subcellular localization of paraspeckle proteins and assess co-localization with stress granules or apoptotic markers.
- In Vivo Toxicity Screening:
Pathway and Workflow Visualizations
Diagram 1: ASO Design to Application Workflow
Diagram 2: ASO and Immunotherapy Combination Mechanism
Diagram 3: ASO Neurotoxicity Challenge and Solution
Antisense oligonucleotides (ASOs) represent a transformative therapeutic modality for ultra-rare genetic diseases, enabling the development of personalized medicines for conditions affecting single-digit patient populations. These short, synthetic DNA or RNA molecules are designed to bind to specific target messenger RNA (mRNA) sequences through Watson-Crick base pairing, modulating gene expression through various mechanisms including RNase H-mediated degradation, splice switching, and translational blockade [55] [2]. The platform nature of ASO technology facilitates rapid customization for individual patients with unique genetic mutations, compressing traditional drug development timelines from years to months [62]. This application note examines pioneering case studies, quantitative outcomes, and standardized protocols that establish a framework for developing n-of-1 ASO therapies within the broader context of gene silencing research.
Case Studies and Clinical Outcomes
Documented Cases of Personalized ASO Interventions
Table 1: Documented Case Studies of Personalized ASO Therapies
| Patient/Cohort | Genetic Condition | Target Gene | ASO Mechanism | Reported Outcomes | Reference |
|---|---|---|---|---|---|
| Mila Makovec | Batten disease (CLN7) | MFSD8 | Splice-switching | Reduction in seizures; stabilization of symptoms | [63] |
| Susannah Rosen | KIF1A-associated neurological disorder | KIF1A | Not specified | Reduced pain, improved movement control, increased energy | [64] |
| Leo | Neurodevelopmental disorder | TNPO2 | Not specified | Development ongoing (by Creyon Bio) | [63] |
| n-Lorem Foundation cohort | Various nano-rare diseases | Multiple | Multiple | Meaningful clinical benefit across various genes, mutations, and disease types | [32] |
| TUBB4A-related leukodystrophy mouse model | H-ABC | TUBB4A | mRNA reduction | Significantly reduced toxic protein; reversal of some symptoms | [57] |
The growing body of evidence demonstrates that personalized ASOs can produce meaningful clinical benefits even in patients with severe, progressive diseases [32]. The n-Lorem Foundation reported in 2025 that their experience with multiple nano-rare patients showed clinical benefits "spanning a wide range of variables, including different genes, mutations, ASO strategies, disease types, patient ages, and stages of disease progression" [32]. These findings support earlier and more proactive treatment approaches for ultra-rare conditions.
Quantitative Development Metrics
Table 2: Personalized ASO Development Statistics and Metrics
| Parameter | Traditional Drug Development | Personalized ASO Development | Sources |
|---|---|---|---|
| Timeline from target identification to treatment | 10-15 years | ~10-12 months | [63] [62] |
| Design and initial synthesis | Several years | Months | [62] |
| FDA-approved ASO therapies | N/A | At least 11 as of late 2024 | [62] |
| Global rare disease population | ~300 million people | ~72-80% have genetic origins | [62] |
| Rare diseases with FDA-approved treatments | <10% | Growing number of n-of-1 approvals | [62] |
The compressed development timeline for personalized ASOs represents a paradigm shift in therapeutic development. Documented n-of-1 programs have achieved first dosing in approximately 10-12 months from mutation identification, with design and initial synthesis completed within months [62]. This acceleration is particularly critical for pediatric patients with rapidly progressive neurodegenerative conditions.
Experimental Protocols and Methodologies
ASO Design and Screening Workflow
Protocol 1: ASO Design and Optimization
Mutation Identification and Analysis
- Perform whole genome sequencing to identify pathogenic variants
- Validate mutation through Sanger sequencing and familial segregation analysis
- Assess RNA accessibility, splice-site characteristics, and mechanistic feasibility using AI-driven platforms [62]
ASO Sequence Design
In Silico Screening
- Predict RNA secondary structures using computational tools
- Evaluate hybridization kinetics and binding affinity
- Screen for potential immunostimulatory motifs
- Select 3-5 lead candidates for synthesis and testing
Preclinical Efficacy and Safety Assessment
Protocol 2: Preclinical Efficacy and Safety Assessment
In Vitro Testing Using Patient-Derived Cells
- Culture patient-derived fibroblasts or induced pluripotent stem cells (iPSCs)
- Transfert ASO candidates using appropriate methods (e.g., electroporation, lipid nanoparticles)
- Measure target mRNA reduction via quantitative RT-PCR
- Assess protein-level changes via Western blot or immunofluorescence
- Evaluate functional endpoints relevant to the specific disease pathology
Animal Model Studies
- Utilize genetically modified animals carrying patient-specific mutations when available
- Administer ASO via clinically relevant route (e.g., intracerebroventricular infusion for neurological disorders)
- Conduct dose-ranging studies to establish therapeutic window
- Evaluate biodistribution in target tissues using labeled ASOs
- Monitor for potential toxicities through clinical observations, clinical pathology, and histopathology
Toxicology Assessment
- Conduct in vitro cytotoxicity assays in relevant cell types
- Evaluate potential for immune activation through cytokine release assays
- Assess complement activation and coagulation parameters
- Leverage platform toxicology data from chemically similar oligonucleotides when appropriate [62]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Personalized ASO Development
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Chemical Modification Reagents | Phosphorothioate, 2'-MOE, LNA monomers | Enhance nuclease resistance, binding affinity, and pharmacokinetics | Balance stability with potential toxicity; PS backbones may cause thrombocytopenia [55] |
| Delivery Systems | Lipid nanoparticles, GalNAc conjugates, dynamic polyconjugates | Facilitate cellular uptake and target tissue delivery | GalNAc enables efficient liver delivery; CNS targets require intrathecal administration [55] [62] |
| Analytical Standards | HPLC standards, mass spectrometry reagents | Quality control, characterization of synthetic ASOs | Ensure purity >95%; confirm identity and sequence fidelity |
| Cell-Based Assay Systems | Patient-derived iPSCs, recombinant cell lines | In vitro efficacy screening and mechanism validation | Patient-specific models may better predict clinical response |
| Enzymes for Mechanism Studies | RNase H, T4 DNA ligase (for circular ASOs) | Study mechanism of action; novel ASO formats | Circular ASOs show enhanced stability against exonuclease digestion [65] |
Emerging Technologies and Future Directions
Advanced ASO Platforms
Circular ASOs (C-ASOs) represent an innovative approach that addresses key limitations of traditional linear ASOs. These covalently closed structures lack free 3' and 5' ends, conferring inherent resistance to exonuclease degradation [65]. Studies demonstrate that C-ASOs remain intact four times longer than linear counterparts in serum (t1/2 = 24.96 h vs 5.99 h) and sustain >50% target knockdown for 96 hours after a single 25 nM dose [65]. This enhanced stability is particularly advantageous for targeting highly structured or repeat-rich RNAs that accumulate in pathological condensates, as in C9orf72-linked amyotrophic lateral sclerosis/frontotemporal dementia (ALS/FTD) [65].
Collaborative Frameworks and Data Sharing
The N=1 Collaborative (N1C) has emerged as a critical global platform for knowledge and data sharing across academia, industry, regulatory agencies, and patient communities [63]. This nonprofit organization facilitates progress by providing guidance, frameworks, and shared infrastructure rather than directly developing n-of-1 treatments. Working groups focus on specific aspects including patient identification, preclinical development, chemistry, manufacturing, controls, and clinical outcomes [63]. The collaborative emphasizes open sharing of data and experiences across n-of-1 programs to accelerate progress and fulfill an ethical imperative to maximize learning from each therapeutic effort.
Personalized ASO therapy represents a paradigm shift in the treatment of ultra-rare genetic conditions, moving from traditional drug development models to patient-specific approaches. The documented cases, standardized protocols, and emerging technologies outlined in this application note provide researchers and drug development professionals with a framework for advancing n-of-1 therapies. As the field evolves, continued innovation in ASO design, delivery technologies, and collaborative frameworks will be essential to overcome remaining challenges in scalability, manufacturing, and regulatory approval. The aggregation of data across individualized treatments through initiatives like the N=1 Collaborative will further accelerate this transformative approach, ultimately expanding treatment options for patients with conditions previously considered untreatable.
Navigating the Challenges: Strategies for Optimizing ASO Safety and Efficacy
A critical challenge in realizing the therapeutic potential of antisense oligonucleotides (ASOs) involves overcoming biological barriers to achieve efficient delivery to target tissues and subsequent cellular uptake. ASOs are short, synthetic nucleic acid strands designed to modulate gene expression by binding to specific RNA targets [3] [12]. However, their inherent properties—including high molecular weight, polyanionic nature, and susceptibility to nuclease degradation—hinder passive diffusion across cell membranes and often result in poor bioavailability [8] [66]. Furthermore, even upon internalization, a significant majority (>90%) of oligonucleotides remain trapped in endosomal compartments, unable to reach their intended sites of action in the cytoplasm or nucleus [66]. This article details advanced strategies and practical methodologies to address these delivery hurdles, providing a framework for researchers to enhance the efficacy of ASO-based therapeutics.
Strategic Approaches for Enhanced ASO Delivery
The successful intracellular delivery of ASOs relies on strategic modifications and carrier systems. The following table summarizes the primary technologies used to overcome key delivery challenges.
Table 1: Strategies to Overcome ASO Delivery Challenges
| Challenge | Strategy | Mechanism | Example |
|---|---|---|---|
| Cellular Uptake | Ligand Conjugation [41] [8] | Targets specific receptors to facilitate receptor-mediated endocytosis. | GalNAc (targets ASGPR on hepatocytes), Cholesterol [8]. |
| Cellular Uptake | Lipid Conjugation [41] | Enhances interaction with cell membranes and promotes uptake via endocytosis. | Vitamin E (α-Tocopherol), Cholesterol conjugates [41]. |
| Endosomal Escape | Nanoparticle Formulations [8] [66] | Protects the ASO and utilizes lipid materials to disrupt endosomal membranes. | Lipid Nanoparticles (LNPs) [66]. |
| Stability & Pharmacokinetics | Polymer Conjugation (e.g., PEG) [8] | Increases hydrodynamic size, reducing renal clearance and improving plasma half-life. | Polyethylene Glycol (PEG) conjugation [8]. |
| Tissue-Specific Targeting | Antibody-Oligonucleotide Conjugates [8] | Uses antibody specificity to deliver ASOs to cells expressing a particular surface antigen. | Anti-CD22 antibody conjugated to a TLR9 agonist [8]. |
Ligand Conjugation for Targeted Delivery
Conjugating ASOs to targeting ligands is a highly effective method for achieving tissue-specific delivery. The most prominent example is N-acetylgalactosamine (GalNAc), which binds with high affinity to the asialoglycoprotein receptor (ASGPR) abundantly expressed on hepatocytes [8]. This approach has led to several approved therapies for liver diseases [8]. The efficacy of this system is demonstrated by GalNAc-conjugated siRNAs like Givosiran and Inclisiran, which show potent and sustained target gene silencing in the liver [8] [61].
Lipid conjugation is another powerful strategy to improve cellular uptake. Cholesterol and Vitamin E (α-tocopherol) are natural lipids easily taken up by cells, often through lipoprotein receptors such as the LDL receptor [41]. A 2025 comparative study demonstrated that cholesterol and vitamin E conjugates of the ASO PNAT524 exhibited potent, dose-dependent exon-skipping activity and cytotoxic effects in cancer cells, whereas aptamer conjugates provided minimal benefit [41]. Among the tested formulations, the cholesterol-conjugated ASO (524-Chol) showed the highest efficacy, with superior splice-modulating and cytotoxic outcomes [41].
Nanoparticle and Other Delivery Systems
For broader tissue targeting or nucleic acids that are difficult to conjugate, nanoparticle formulations provide an alternative. Lipid Nanoparticles (LNPs), such as those used in the approved siRNA therapy Patisiran, protect the oligonucleotide during circulation and facilitate cellular entry and endosomal escape [66] [61].
Antibody-oligonucleotide conjugates represent a frontier in precision delivery, enabling targeting of specific cell types, such as cancer cells. For instance, an anti-CD22 antibody conjugated to a TLR9 agonist (TAC-001) is currently in clinical trials for advanced solid tumors and B-cell lymphoma [8].
Table 2: Quantitative Efficacy of Different ASO Conjugation Strategies
| Conjugation Type | ASO Backbone | Target/Cell Model | Key Efficacy Metric | Reported Outcome |
|---|---|---|---|---|
| Cholesterol [41] | PNAT524 (2'-OMe PS) | EGFR / Cancer cell lines | Exon-skipping efficiency & Cytotoxicity | Highest efficacy; potent, dose-dependent activity. |
| Vitamin E (α-Tocopherol) [41] | PNAT524 (2'-OMe PS) | EGFR / Cancer cell lines | Exon-skipping efficiency & Cytotoxicity | Potent, dose-dependent activity. |
| Aptamer (AS1411) [41] | PNAT524 (2'-OMe PS) | Nucleolin / Cancer cell lines | Exon-skipping efficiency | No significant enhancement vs. unconjugated ASO. |
| GalNAc [8] | Various siRNAs/ASOs | ASGPR / Hepatocytes | Target mRNA Knockdown | Highly efficient liver-specific delivery; multiple approved drugs. |
Experimental Protocols for Evaluating ASO Delivery
Robust experimental protocols are essential for evaluating the success of ASO delivery strategies. The following section outlines key methodologies.
Protocol: Synthesis of Biomolecule-ASO Conjugates
This protocol outlines the conjugation of lipids or other molecules to an ASO backbone, based on methods used in a recent comparative study [41].
- Reagents: 2'-O-methyl phosphorothioate (2'-OMe PS) ASO (e.g., PNAT524), Cholesterol-NHS ester, Vitamin E derivative (e.g., α-tocopherol-succinate-NHS), C6 Thiol linker, Triethylene Glycol (TEG) linker, appropriate conjugation buffer (e.g., 0.1 M phosphate buffer, pH 8.5), purification equipment (HPLC or FPLC).
- Procedure:
- Linker Attachment: First, covalently attach a bifunctional linker to the 5' or 3' end of the synthesized ASO. For cholesterol and vitamin E, a C6 thiol linker was used to create a disulfide bond (524-S-S-Chol, 524-S-S-VitE) [41]. For some aptamer conjugates, a TEG linker was employed (524-TEG-S2.2) [41].
- Ligand Conjugation: Incubate the linker-modified ASO with a 2-5 molar excess of the ligand (e.g., cholesterol or vitamin E derivative) for 12-16 hours at 4°C in conjugation buffer with gentle agitation. The disulfide bond is cleavable in the reductive intracellular environment, facilitating ASO release.
- Purification: Purify the conjugate from unreacted starting materials using reverse-phase or ion-exchange HPLC/FPLC.
- Characterization: Verify the identity and purity of the final product using analytical HPLC and mass spectrometry (LC-MS).
Protocol: Assessing Cellular Uptake and Subcellular Localization
This protocol describes how to quantitatively and qualitatively assess the internalization of conjugated ASOs into cells.
- Reagents: Fluorescently labeled ASOs (e.g., Cy3 or Cy5 tagged), relevant cell culture lines, culture media, transfection reagents (for positive control), fixation solution (e.g., 4% paraformaldehyde), mounting medium with DAPI, fluorescence microscope or confocal microscope.
- Procedure [41]:
- Cell Seeding: Seed cells onto glass-bottom culture dishes or multi-well plates and culture until they reach 60-80% confluency.
- ASO Treatment: Treat cells with a range of concentrations (e.g., 100 nM - 1 µM) of fluorescently labeled, conjugated ASOs and unconjugated ASOs as a control. Incubate for a defined period (e.g., 4-24 hours). A positive control using a transfection reagent can be included.
- Fixation and Staining: Wash cells with PBS to remove non-internalized ASOs. Fix cells with 4% PFA for 15 minutes, then permeabilize if intracellular staining is required. Counterstain nuclei with DAPI.
- Imaging and Analysis: Visualize using fluorescence or confocal microscopy. Co-localization studies with organelle-specific markers (e.g., LysoTracker for endosomes/lysosomes) can determine subcellular localization. Quantify fluorescence intensity using image analysis software to compare uptake efficiency between different ASO formulations.
Protocol: Evaluating Functional Efficacy (Exon Skipping)
This protocol measures the functional consequence of successful ASO delivery, using splice-switching as a model.
- Reagents: Treated cells from Protocol 3.2, RNA extraction kit (e.g., TRIzol), Reverse Transcription kit, quantitative PCR (qPCR) system, primers spanning the target exon and a control gene, agarose gel electrophoresis system.
- Procedure [41]:
- RNA Isolation: Extract total RNA from treated and control cells 24-48 hours post-ASO treatment.
- cDNA Synthesis: Synthesize cDNA from equal amounts of RNA using a reverse transcription kit.
- RT-PCR Analysis: Perform PCR using primers that flank the target exon. Resolve the PCR products by agarose gel electrophoresis. Successful exon skipping will result in a shorter PCR product band compared to the full-length product.
- Quantification: Quantify the relative intensity of the bands to calculate the percentage of exon skipping. Alternatively, use quantitative RT-PCR (RT-qPCR) with specific assays to quantify the different transcript isoforms.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their functions for conducting research on ASO delivery.
Table 3: Key Research Reagents for ASO Delivery Studies
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| N-Acetylgalactosamine (GalNAc) [8] | Ligand for targeted delivery to hepatocytes via ASGPR. | Industry-standard for liver-targeting; high affinity and specificity. |
| Cholesterol [41] [8] | Lipid conjugate to enhance cellular uptake via lipoprotein receptors. | Improves pharmacokinetics and facilitates entry into various cell types. |
| Vitamin E (α-Tocopherol) [41] | Lipid conjugate for receptor-mediated uptake via LRP/LDLR. | Can form micelle-like structures for improved internalization. |
| Triethylene Glycol (TEG) Linker [41] | Spacer between ASO and ligand to reduce steric hindrance. | Critical for maintaining the bioactivity of both the ASO and the ligand. |
| C6 Thiol Linker [41] | Creates a cleavable disulfide bond for intracellular ASO release. | Enhances efficacy by facilitating the release of the free ASO in the cytoplasm. |
| Lipid Nanoparticles (LNPs) [66] [61] | Delivery system for protecting ASOs and facilitating endosomal escape. | Essential for delivering large or double-stranded RNAs (e.g., siRNA). |
| Fluorescent Dyes (Cy3, Cy5) [41] | Labeling ASOs for visualization and quantification of cellular uptake. | Allows for tracking via fluorescence microscopy or flow cytometry. |
Visualizing Key Pathways and Workflows
Diagram: Receptor-Mediated ASO Uptake Pathway
The following diagram illustrates the primary pathway for targeted ASO delivery via ligand conjugation.
Diagram 1: Receptor-mediated ASO uptake and intracellular trafficking, highlighting the critical endosomal escape step.
Diagram: Experimental Workflow for ASO Delivery Evaluation
This workflow charts the key steps from conjugate synthesis to functional validation.
Diagram 2: Sequential workflow for synthesizing and evaluating ASO conjugates, from creation to functional analysis.
Mitigating Off-Target Effects and Immune Stimulation
Antisense oligonucleotides (ASOs) represent a promising class of therapeutic agents that specifically target gene transcription or translation mechanisms through Watson-Crick base pairing, demonstrating significant potential for treating genetic disorders, malignancies, and metabolic diseases [67]. However, unintended toxicity remains a considerable challenge in oligonucleotide therapeutic (ONT) development, primarily arising from two distinct mechanisms: hybridization-dependent off-target effects and hybridization-independent effects, including unintended immune stimulation [67] [68]. These effects can result in diminished transcript levels, decreased translation rates, anomalous splicing, or activation of inflammatory pathways, employing the same molecular pathways and protein machinery as the desired on-target effects [67]. Understanding and mitigating these unintended effects is crucial for improving the therapeutic index of ASO drugs and ensuring their clinical safety.
The phosphorothioate (PS) backbone, a common modification used to enhance nuclease resistance and cellular uptake of ASOs, contributes significantly to these challenges by facilitating non-specific protein interactions [69] [70]. Furthermore, certain ASO sequences can activate innate immune sensors, particularly Toll-like receptors (TLRs), leading to potentially severe inflammatory responses [71]. This application note provides a comprehensive overview of the mechanisms underlying these effects and offers detailed protocols for their systematic evaluation and mitigation during ASO drug development.
Mechanisms of Unintended Effects
Hybridization-Dependent Off-Target Effects
Hybridization-dependent off-target effects occur when ASOs bind to RNA transcripts with sequences similar but not identical to the intended target. This partial complementarity can lead to unintended RNA degradation or modulation, potentially causing adverse phenotypic outcomes [67] [72]. The risk of such effects increases significantly with the number of tolerated mismatches between the ASO and off-target transcripts. Research demonstrates that for an 18-mer ASO, the theoretical number of perfectly complementary sites in the human pre-mRNA database is less than 1, but this increases dramatically to approximately 23 sites with two mismatches and 375 sites with three mismatches [72]. This exponential increase highlights the substantial challenge of achieving perfect specificity with ASO therapeutics.
The gapmer design, which incorporates high-affinity ribose modifications (such as 2'-MOE or LNA) on the wings with a central DNA region for RNase H1 activation, is particularly susceptible to these effects due to its potent RNA degradation capability [72]. Gapmer ASOs can bind not just to mRNA but also to pre-mRNA introns, cleaving and degrading pre-mRNA, thereby expanding the potential off-target landscape [72]. Conventional animal studies often cannot adequately assess toxicity induced by these off-target effects due to differences in genome sequences between humans and other animals, necessitating specialized in silico and in vitro approaches for proper evaluation [72].
Hybridization-Independent Effects and Immune Stimulation
Hybridization-independent effects primarily stem from sequence- or chemistry-dependent interactions between ASOs and cellular proteins, leading to various toxicities without involving RNA hybridization [68]. A significant concern is the unintended activation of the innate immune system, which can occur through multiple pathways:
Toll-like Receptor (TLR) Activation: Non-CpG PS-ASOs can activate TLR9, an endosomal-localized receptor that typically recognizes unmethylated cytosine-phosphate-guanine (CpG) motifs in bacterial and viral DNA [69] [71]. This activation occurs despite the absence of traditional CpG motifs, with the strength of immune response varying based on ASO sequence, PS content, and specific 2' modifications [69]. TLR9 activation triggers a signaling cascade involving MyD88 and UNC93B1, ultimately leading to NF-κB activation and the expression of pro-inflammatory cytokines [71]. The phosphorothioate backbone enhances protein binding, facilitating TLR9 engagement, while certain extracellular proteins (e.g., HMGB1, S100A8, HRG) can further potentiate these immune responses by forming complexes with PS-ASOs [69].
Other Nucleic Acid Sensors: Beyond TLR9, ASOs can potentially activate other pattern recognition receptors, including TLR3 (double-stranded RNA), TLR7/8 (single-stranded RNA), RIG-I (cytoplasmic RNA), MDA5 (double-stranded RNA), and cGAS-STING (cytosolic DNA) pathways [71]. The structural features of ASOs, including backbone chemistry and secondary structures, influence which sensors are engaged and the resulting immune profile.
Sequence and Chemistry Dependencies: Immune stimulation varies significantly with ASO design parameters. PS content is a critical factor, with ASOs containing fewer than 10 phosphorothioate linkages being unlikely to bind TLR9 or activate innate immunity [71]. Similarly, 2' modifications influence immunostimulatory potential, where more hydrophobic modifications like constrained ethyl (cEt) tend to be more immune-stimulatory than 2'-MOE modifications [71]. Sequence context, particularly the presence and positioning of CpG dinucleotides, also significantly impacts TLR9 activation, with higher CpG content generally correlating with increased immune stimulation [71].
Figure 1: ASO-mediated immune stimulation can occur through the TLR9 pathway in endosomal compartments. PS-ASOs can bind TLR9 directly or as complexes with extracellular proteins, leading to downstream signaling and pro-inflammatory cytokine production.
Quantitative Assessment of Off-Target Effects
In Silico Prediction of Off-Target Interactions
Computational approaches provide a foundational method for identifying potential off-target candidates during ASO design. These methods involve screening ASO sequences against comprehensive human RNA databases to identify transcripts with significant complementarity.
Table 1: Theoretical Number of Complementary Sites in Human Pre-mRNA for ASOs of Different Lengths [72]
| ASO Length (nt) | 0 Mismatches | 1 Mismatch | 2 Mismatches | 3 Mismatches | 4 Mismatches | 5 Mismatches |
|---|---|---|---|---|---|---|
| 27 | <0.1 | <0.1 | <0.1 | <0.1 | <0.1 | 1.3 |
| 26 | <0.1 | <0.1 | <0.1 | <0.1 | 0.31 | 4.1 |
| 25 | <0.1 | <0.1 | <0.1 | <0.1 | 1.1 | 13 |
| 20 | <0.1 | <0.1 | 1.8 | 33 | 417 | 4,005 |
| 18 | <0.1 | 0.92 | 23 | 375 | 4,216 | >10,000 |
| 16 | 0.27 | 13 | 294 | 4,115 | >10,000 | >10,000 |
| 15 | 1.1 | 49 | 1,029 | >10,000 | >10,000 | >10,000 |
| 14 | 4.4 | 183 | 3,566 | >10,000 | >10,000 | >10,000 |
| 13 | 17 | 679 | >10,000 | >10,000 | >10,000 | >10,000 |
| 12 | 70 | 2,508 | >10,000 | >10,000 | >10,000 | >10,000 |
| 11 | 279 | 9,196 | >10,000 | >10,000 | >10,000 | >10,000 |
| 10 | 1,114 | >10,000 | >10,000 | >10,000 | >10,000 | >10,000 |
The data reveal the dramatic increase in potential off-target sites as the number of allowed mismatches increases, particularly for shorter ASOs. This underscores the importance of comprehensive in silico screening during the design phase to identify and mitigate potential off-target risks.
Experimental Assessment Using Microarray Analysis
Following in silico prediction, experimental validation is essential to confirm actual off-target effects in biological systems. Microarray analysis provides a comprehensive approach to evaluate genome-wide expression changes following ASO treatment.
Protocol: Evaluation of Gapmer ASO Off-Target Effects by Microarray Analysis [72]
Materials and Reagents:
- Human cell line relevant to target biology (e.g., Huh-7 hepatocyte cell line for liver targets)
- Gapmer ASO and appropriate control oligonucleotides
- Transfection reagent or system for efficient ASO delivery
- RNA extraction kit (e.g., RNeasy Mini Kit)
- Microarray platform or RNA-seq reagents
- qRT-PCR reagents for validation
Procedure:
- Cell Seeding and Transfection: Plate cells at optimal density (typically 30-50% confluency for adherent cells) and allow to adhere overnight. Transfect with gapmer ASO at concentrations ranging from 10-100 nM using appropriate transfection methods. Include negative control (scrambled sequence) and positive control (known effective ASO) in experimental design.
- RNA Extraction: At 24-72 hours post-transfection, extract total RNA using validated methods. Ensure RNA integrity numbers (RIN) >8.0 for quality microarray data.
- Microarray Processing: Process RNA samples according to microarray manufacturer specifications. This typically includes cDNA synthesis, labeling, hybridization to array chips, and scanning.
- Data Analysis: Identify significantly differentially expressed genes (e.g., >2-fold change, p-value <0.05). Compare expression profiles between ASO-treated and control samples.
- In Silico Correlation: Cross-reference differentially expressed genes with in silico predictions of off-target candidates based on sequence complementarity. Calculate the "distance" (d) as the total number of mismatches, insertions, or deletions between ASO and off-target RNA sequences.
- Validation: Confirm key off-target hits using qRT-PCR with specific primers for identified genes.
Expected Outcomes: This protocol typically identifies numerous off-target candidate genes with varying degrees of complementarity to the administered ASO. Research shows that the magnitude of off-target effects correlates with the degree of complementarity, with perfect matches causing the most significant effects, followed by single mismatches, then double mismatches [72]. This approach provides experimental evidence of actual off-target effects at the cellular level, complementing in silico predictions.
Assessment of Immune Stimulation
In Vitro Models for Evaluating ASO-Induced Immune Activation
Multiple in vitro systems are available for assessing the innate immune potential of ASO candidates, each offering different advantages for mechanistic studies or screening.
Table 2: In Vitro Systems for Assessing ASO-Induced Immune Stimulation
| Cell System | Applications | Key Readouts | Advantages | Limitations |
|---|---|---|---|---|
| Human Peripheral Blood Mononuclear Cells (PBMCs) [71] | Screening immune potential of ASO candidates | Cytokine secretion (IL-6, TNF-α, IFNs), activation markers | Primary human cells with native immune repertoire, clinically relevant | Donor variability, complex data interpretation |
| BJAB Cells [71] | Mechanistic studies of TLR9 signaling | NF-κB activation, cytokine production, gene expression | B-cell line endogenously expressing TLR9, consistent responses | Limited to specific immune cell type |
| HEK293-TLR9 Reporter Cells [69] [71] | Specific TLR9 pathway activation | Reporter gene expression (luciferase, SEAP), NF-κB activation | High sensitivity for TLR9, low background, suitable for screening | Overexpression system, may not reflect native physiology |
| Plasmacytoid Dendritic Cells (pDCs) [73] | Evaluation of interferon response | Type I interferon production (IFN-α, IFN-β), maturation markers | Highly specialized IFN-producing cells, gold standard for IFN response | Limited availability, technical challenges in culture |
Protocol: Assessment of PS-ASO Innate Immune Responses in Immune Cell Models [69] [71]
Materials and Reagents:
- Appropriate cell model (e.g., PBMCs, BJAB cells, or HEK293-TLR9 cells)
- Test PS-ASOs and controls (including known immune-stimulatory and non-stimulatory ASOs)
- Cell culture medium and supplements
- Cytokine detection kits (ELISA or multiplex immunoassays for IL-6, TNF-α, IFN-α)
- RNA extraction and qRT-PCR reagents
- Transfection reagents (if required)
Procedure:
- Cell Preparation: Isolate PBMCs from fresh human blood using density gradient centrifugation or thaw cryopreserved PBMCs. Alternatively, culture immortalized cell lines (BJAB, HEK293-TLR9) according to standard protocols.
- ASO Treatment: Treat cells with ASOs across a concentration range (typically 0.1-10 μM). For some cell types (e.g., PBMCs), delivery reagents may not be required due to inherent PS-ASO uptake; for others, optimize transfection conditions.
- Incubation and Sampling: Incubate cells for 6-48 hours, collecting supernatants and cell pellets at multiple time points to capture kinetic differences in immune responses.
- Cytokine Measurement: Analyze culture supernatants using ELISA or multiplex assays for key cytokines (IL-6, TNF-α, IFN-α, IP-10). Include standard curves for accurate quantification.
- Gene Expression Analysis: Extract RNA from cell pellets and perform qRT-PCR for immune-related genes (e.g., NF-κB target genes, interferon-stimulated genes).
- Pathway Analysis: For mechanistic studies, utilize specific inhibitors (e.g., TLR9 antagonists) or genetic approaches (siRNA knockdown) to confirm involvement of specific pathways.
Data Interpretation: Immune-stimulatory ASOs typically show dose-dependent increases in cytokine production and immune-related gene expression. The kinetics of response may vary, with full agonists generating rapid induction and partial agonists showing delayed or attenuated responses [71]. Comparison to established controls helps classify the immune potential of novel ASOs.
Strategic Mitigation of Unintended Effects
Chemistry-Based Mitigation Approaches
Strategic chemical modifications can significantly reduce both off-target hybridization and immune stimulation while maintaining on-target potency:
Backbone and Sugar Modifications: Reducing phosphorothioate content or introducing site-specific modifications (e.g., mesyl-phosphonate or methoxy modifications at gap positions 2-3) can decrease protein binding and subsequent immune activation without compromising efficacy [71] [68]. The incorporation of 2'-MOE modifications in the wings of gapmer ASOs dramatically reduces immune stimulation compared to unmodified oligodeoxynucleotides while enhancing target affinity [71] [70].
Sequence Optimization: Avoiding CpG dinucleotides, particularly in specific sequence contexts, minimizes TLR9-mediated immune responses [71] [27]. Substituting 5-methyl-dC for dC in CpG motifs can further reduce immune recognition while slightly increasing Tm [27]. Additionally, screening ASO sequences for homopolymeric stretches or other problematic motifs helps prevent aggregate formation and unintended protein interactions.
Table 3: Chemical Modification Strategies to Mitigate Unintended Effects
| Modification Type | Specific Approach | Impact on Off-Target Effects | Impact on Immune Stimulation | Considerations |
|---|---|---|---|---|
| Backbone | Reduced PS content (<10 PS) | Minimal direct impact | Significant reduction | May affect pharmacokinetics and cellular uptake |
| Backbone | Site-selective mesyl-phosphonate | Moderate reduction | Moderate reduction in some cases | Position-dependent effects |
| Sugar | 2'-MOE modifications | Reduces affinity for mismatched targets | Dramatic reduction | Enhanced nuclease resistance and target affinity |
| Sugar | Constrained ethyl (cEt) | Reduces affinity for mismatched targets | Generally more immune-stimulatory | Higher potency but potentially worse toxicity profile |
| Base | 5-Methyl-dC substitution in CpG motifs | No direct impact | Significant reduction in TLR9 activation | Slight increase in Tm |
| Design | Gapmer with 5-10-5 2'MOE design | Balanced specificity and potency | Reduced compared to full PS ODNs | Industry standard for RNase H-dependent ASOs |
Advanced Design Strategies
Toehold-Mediated Strand Displacement (BROTHERS Technology): A novel approach involves creating ASO/peptide nucleic acid (PNA) duplexes called BROTHERS (BRace On a THERapeutic aSo), where a partially complementary PNA strand acts as a safety mechanism [68]. This system operates through toehold-mediated strand displacement (TMSD), enhancing specificity by requiring more precise complementarity for effective target binding. The BROTHERS architecture reduces both hybridization-independent protein interactions and hybridization-dependent off-target effects while maintaining on-target activity [68].
Optimized Screening Strategies: Implementing comprehensive screening workflows that include in silico prediction followed by experimental validation in relevant human cell models helps identify problematic sequences early in development [72]. This involves:
- Initial bioinformatic screening against human transcriptome databases
- Primary in vitro testing for on-target efficacy
- Secondary screening for off-target effects (microarray/RNA-seq) and immune stimulation (immune cell assays)
- Counter-screening against protein binding panels to identify sequences with favorable interaction profiles
Figure 2: The BROTHERS technology utilizes toehold-mediated strand displacement to enhance ASO specificity. The brother strand (BS) dissociates only when perfect complementarity is detected, preventing off-target binding while maintaining on-target activity.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for ASO Off-Target and Immune Effect Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Control ASOs | Scrambled sequence, Mismatch controls, Known immune-stimulatory ASOs | Experimental controls for baseline comparison | Essential for distinguishing specific from non-specific effects |
| Cell Models | Huh-7 hepatocytes, HEK293-TLR9, BJAB cells, Primary PBMCs | Evaluating ASO activity and toxicity in relevant biological systems | Select models based on research question (mechanistic vs. screening) |
| Detection Assays | ELISA/multiplex cytokine panels, RNA extraction kits, microarray/RNA-seq platforms | Quantifying immune responses and transcriptome changes | Multiplex approaches provide comprehensive profiling |
| Transfection Reagents | Lipofection agents, Electroporation systems | ASO delivery for in vitro studies | Consider reagent-associated toxicity; some ASOs are self-delivering |
| Chemical Modification Kits | Phosphorothioate, 2'-MOE, 2'-OMe, LNA incorporation | Synthesis of modified ASOs for structure-activity studies | Custom synthesis often required for complex modifications |
| Bioinformatics Tools | BLAST, Off-target prediction algorithms, Transcriptome databases | In silico prediction of potential off-target interactions | Essential for rational ASO design prior to synthesis |
| Specialized ASO Formats | BROTHERS (ASO/PNA duplex), GalNAc-conjugates | Advanced delivery and specificity enhancement | Require specialized synthesis expertise |
Mitigating off-target effects and immune stimulation remains a critical challenge in ASO therapeutic development. A multifaceted approach combining thoughtful sequence design, strategic chemical modifications, and comprehensive screening strategies offers the most effective path forward. The implementation of robust assessment protocols, including both in silico predictions and experimental validations, enables researchers to identify and address potential toxicity issues early in the development process. Emerging technologies such as BROTHERS ASO/PNA duplexes demonstrate promising approaches to enhance specificity and reduce unintended interactions while maintaining therapeutic efficacy. As the field advances, continued refinement of these strategies will be essential for realizing the full potential of ASO therapeutics across a broadening spectrum of diseases.
Toxicity Profiles and Strategies for Risk Management
Antisense oligonucleotides (ASOs) represent a promising class of therapeutics that target disease-causing genes through precise RNA-mediated mechanisms. By binding to specific RNA sequences, ASOs can prevent the production of harmful proteins or alter gene expression, offering potential treatments for previously difficult-to-address genetic disorders [74]. However, their development is accompanied by complex toxicity profiles that necessitate careful risk management strategies throughout the preclinical and clinical development process. This document provides a detailed overview of ASO toxicity mechanisms, monitoring biomarkers, and experimental protocols for risk assessment, framed within the context of gene silencing research for scientific and drug development professionals.
ASO Toxicity Profiles: Mechanisms and Target Organs
ASOs exhibit distinctive toxicological challenges that differ from traditional small molecules or biologics. These toxicities are primarily mediated through hybridization-dependent off-target effects, RNase-H1-dependent reduction in off-target RNAs, and non-specific chemical interactions [75]. The accumulation of ASOs in specific tissues, particularly the liver and kidneys, is central to many observed toxic effects.
Table 1: Primary Toxicity Profiles of ASOs
| Toxicity Type | Primary Mechanisms | Target Organs/Tissues | Key Contributing Factors |
|---|---|---|---|
| Hepatotoxicity | Binding to unintended RNA sequences; disruption of metabolism; induction of stress in hepatocytes [74] | Liver | Sequence specificity; systemic delivery; high tissue accumulation |
| Nephrotoxicity | Accumulation in lysosomes of proximal tubules leading to cellular damage [74] | Kidneys | Primarily accumulation-related; largely sequence unspecific |
| Thrombocytopenia | Inhibition of coagulation pathways [74] | Blood/coagulation system | Plasma concentrations exceeding threshold levels |
| Inflammatory Responses | Activation of immune pathways; complement activation [74] | Systemic/local tissues | Delivery route; chemical modifications |
| Neurotoxicity | Acute: disturbances in calcium ion flow between neurons [60]; Late-onset: p53-activated pathways & paraspeckle protein mislocalization [76] | Central Nervous System | Intrathecal or intracerebroventricular administration; specific chemical structures |
The persistence and accumulation of ASOs in tissues, especially the liver and kidneys, are central to these toxic effects [75]. The pattern of toxicity also varies significantly based on administration route. Systemically delivered ASOs may result in hepatotoxicity, nephrotoxicity, thrombocytopenia, and local/systemic inflammation, while those directly delivered to the central nervous system (CNS) are associated with CNS-specific toxicities [74].
Late-Onset Neurotoxicity Mechanisms
Recent research has identified late-onset neurotoxicity as a distinct adverse event separate from acute neurotoxicity, with fundamentally different mechanisms [60]. This condition typically presents with hypoactivity in motor function and consciousness persisting for six days or more after ASO administration. The molecular mechanism involves abnormal aggregation of paraspeckle proteins, which in turn promotes cell-death pathways regulated by p53 [76] [60]. This pathway represents a significant challenge for CNS-targeting ASO therapies and requires specific risk mitigation strategies.
Diagram 1: Late-onset neurotoxicity pathway
Biomarker Monitoring and Risk Assessment
Comprehensive biomarker monitoring is essential for characterizing ASO safety profiles. The following parameters should be incorporated into toxicology studies for thorough evaluations, particularly in early preliminary studies to establish reliable safety signals [74].
Table 2: Essential Biomarkers for ASO Toxicity Monitoring
| Toxicity Category | Biomarkers | Sample Type | Monitoring Frequency |
|---|---|---|---|
| Liver Toxicity | ALT, AST [74] | Serum | Single dose & multiple dose studies |
| Kidney Toxicity | BUN, serum creatinine [74] | Serum | Single dose & multiple dose studies |
| Inflammatory Responses | Clinical observations, fever, inflammatory cytokines [74] | Serum, clinical assessment | Throughout study duration |
| Coagulation Activation | Split products Bb and C5a [74] | Plasma | Peak exposure periods |
| Immunogenicity | Anti-drug antibody (ADA) responses [74] | Serum | Preclinical and clinical trials |
Early integration of these biomarkers allows developers to identify risks at an initial stage before advancing to clinical trials [74]. The analysis should be guided by pharmacokinetic (PK), pharmacodynamic (PD), and early toxicity profiles to establish correlation with exposure levels.
Risk Mitigation Strategies
Chemical Modifications to Enhance Safety
Chemical modifications play a critical role in improving ASO stability and specificity while reducing toxic side effects. These modifications can also reduce the minimum therapeutic dose required to achieve pharmacodynamic effects, subsequently improving safety margins [74].
Table 3: Chemical Modification Strategies for Toxicity Reduction
| Modification Type | Toxicity Addressed | Mechanism of Action | Impact on Efficacy |
|---|---|---|---|
| 5′-cyclopropylene (5′-CP) | Late-onset neurotoxicity [76] | Prevents undesired interactions with toxicity-related factors; reduces paraspeckle protein mislocalization [60] | Maintains knockdown activity with optimized positioning [60] |
| Phosphodiester (PO) bonds | General neurotoxic effects [60] | Replaces phosphorothioate (PS) bonds to improve ASO-mRNA binding affinity while reducing toxic side effects | Preserves knockdown activity [60] |
| 2′-O-methoxyethyl (MOE) | Nuclease degradation; stability [75] | Improves binding affinity and reduces susceptibility to degradation | Enhances stability and prolongs activity |
| GalNAc conjugation | Off-target effects [75] | Targets ASOs to hepatocytes, minimizing exposure to other tissues | Enhances liver-specific delivery and potency |
| Phosphorothioate (PS) backbone | Nuclease degradation [75] | Reduces degradation by nucleases, extending ASO stability | Improves pharmacokinetic properties |
There can be a tradeoff between reducing toxicity and maintaining gene silencing activity with some modifications [60]. However, by optimizing the number, position, and combination of new chemical modifications, it is possible to achieve both safety and efficacy goals [60]. For instance, the 5′-CP modification significantly reduces late-onset neurotoxicity without compromising knockdown activity when properly positioned [76].
Diagram 2: Chemical modification strategies for toxicity reduction
Pharmacokinetic Considerations
ASOs possess unique pharmacokinetic profiles that differ significantly from traditional small molecules or biologics. They generally distribute rapidly and have short plasma half-lives of less than an hour, but can accumulate in tissues, resulting in long tissue half-lives [74]. This discrepancy necessitates thorough characterization of PK properties following single and multiple doses early in drug development.
When systemic PK properties do not adequately reflect target tissue distribution, researchers should include PD biomarkers in studies to accurately assess ASO effects [74]. Species selection is also critical, with developers ensuring pharmacological activity in at least one relevant species for toxicity assessment [74].
Experimental Protocols for Toxicity Assessment
Protocol 1: Comprehensive In Vivo Toxicity Study
Objective: To evaluate the potential toxicities of ASO candidates following systemic administration and identify target organs of toxicity.
Test System: Rodent species (rats or mice) and non-rodent species (e.g., monkeys) as appropriate for pharmacological activity [74].
Dose Design:
- At least three dose levels plus control group
- Include a maximum tolerated dose (MTD) that produces minimal toxicity
- Include a low dose that provides exposure comparable to anticipated human exposure
Study Duration: 14-28 days with recovery group to assess reversibility
Key Procedures:
- Daily clinical observations for behavioral changes and physical condition
- Detailed weekly clinical pathology assessments including:
- Hematology: complete blood count with platelet quantification
- Clinical chemistry: ALT, AST, BUN, serum creatinine
- Coagulation parameters: split products Bb and C5a
- Regular measurement of inflammatory cytokines
- Toxicokinetic sampling at multiple time points to characterize exposure
- Comprehensive gross necropsy and histopathological examination of all major organs
Deliverables: Detailed study report with dose-toxicity relationships, target organ identification, and recommended safety parameters for clinical trials [74].
Protocol 2: CNS Toxicity Assessment for Intrathecally Administered ASOs
Objective: To evaluate potential neurotoxicity of ASO candidates targeting the central nervous system.
Test System: Rodent models with intracerebroventricular (ICV) or intrathecal (IT) administration [76]
Dose Design:
- Dose escalation study to identify neurotoxic threshold
- Include vehicle control group
- Doses should bracket anticipated human therapeutic exposure
Study Duration: Acute (24-72 hours) and extended (14-28 days) observation periods to capture both acute and late-onset neurotoxicity [60]
Key Procedures:
- Continuous monitoring for acute neurotoxicity signs (tremors, seizures) in first 24 hours
- Automated motor activity assessment at multiple time points
- Functional observational battery (FOB) including:
- Neuromuscular function assessment
- Sensorimotor responses
- Autonomic function measurements
- Histopathological evaluation of brain and spinal cord tissues
- Immunohistochemistry for p53 activation and paraspeckle protein localization [76]
- Assessment of specific biomarkers associated with neuronal injury
Deliverables: Neurotoxicity risk assessment with identification of safe dosing parameters for CNS-targeted ASOs.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for ASO Toxicity Assessment
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| Gapmer ASOs | Transcript knockdown via RNase H mechanism [12] | Various sequences with chemical modifications |
| Splice-Switching ASOs | Modulation of pre-mRNA splicing [12] | Sequence-specific designs for target exons |
| siRNA Controls | Alternative knockdown approach for comparison studies [55] | Validated siRNA sequences for target genes |
| Cytokine Panels | Monitoring inflammatory responses to ASO treatment [74] | Multiplex assays for IL-6, TNF-α, IFN-γ |
| Liver Toxicity Assays | Assessment of hepatotoxicity [74] | ALT, AST measurement kits |
| Kidney Function Assays | Evaluation of nephrotoxicity [74] | BUN, serum creatinine test kits |
| Coagulation Markers | Monitoring thrombocytopenia risk [74] | Bb and C5a split product assays |
| Neurotoxicity Markers | Assessment of CNS-specific toxicity [76] | p53 pathway biomarkers, paraspeckle protein detection |
| ADA Assays | Immunogenicity assessment [74] | Anti-drug antibody detection protocols |
Regulatory and Safety Considerations
ASOs follow a hybrid regulatory pathway because they share characteristics with both small molecules and biologics [74]. Their development generally follows the pathway of small molecules (ICH M3), but additional immunogenicity and target specificity considerations align them with biologics [75].
Regulatory bodies have developed tailored frameworks for ASOs, including accelerated pathways for those targeting rare genetic disorders [74]. This allows patients faster access to treatments while developers gather safety data post-approval. Consequently, developers must implement robust post-marketing surveillance programs that monitor safety and efficacy over extended periods [74].
Effective risk management throughout the development lifecycle should focus on:
- Species selection ensuring pharmacological activity in at least one species [74]
- Early PK/PD characterization establishing relationships between dosing, PK profile, and therapeutic effects [74]
- Biomarker integration monitoring common ASO toxicities throughout development [74]
- Chemical modification optimization to enhance safety profiles while maintaining efficacy [60]
- Long-term safety monitoring to address the relatively limited experience with chronic ASO exposure [75]
By implementing these comprehensive risk assessment and management strategies, developers can navigate the complex toxicity profiles of ASOs while advancing promising therapeutics for patients with genetic disorders.
Scalability and Manufacturing Considerations for Clinical Translation
The clinical translation of Antisense Oligonucleotides (ASOs) from research to therapeutic application is a complex process that hinges on overcoming significant scalability and manufacturing challenges. ASOs, short, synthetic single-stranded DNA or RNA molecules, are designed to selectively bind target RNA sequences to modulate gene expression for treating genetic disorders, cancers, and other diseases [12]. While their therapeutic potential is substantial, their successful development requires a comprehensive understanding of key factors including bioconjugation, tailored bioanalytical techniques, and rigorous characterization to ensure consistency, purity, and functionality at commercial scales [8] [77]. This document outlines critical considerations, recommended practices, and standardized protocols to guide researchers and drug development professionals in navigating the path from laboratory-scale synthesis to industrial Good Manufacturing Practice (GMP) production.
Key Scalability Challenges and Industrial Strategies
Scaling ASO production presents unique hurdles not typically encountered with traditional small-molecule drugs. The following table summarizes the primary challenges and corresponding industry-adopted strategies to mitigate them.
Table 1: Key Scalability Challenges and Industrial Mitigation Strategies for ASO Therapeutics
| Challenge Domain | Specific Scalability Challenge | Industry Strategy & Solution |
|---|---|---|
| Chemical Synthesis & Purification | Long oligonucleotide sequences with complex modifications are difficult to synthesize with high yield and purity at large scale [78]. | Invest in and optimize solid-phase phosphoramidite synthesis; develop robust, scalable purification techniques (e.g., HPLC, tangential flow filtration) [78]. |
| Delivery System Manufacturing | Complexity of nanocarrier formulations (e.g., Lipid Nanoparticles - LNPs) and ensuring batch-to-batch consistency [77] [78]. | Implement scalable, reproducible nanocarrier production methods like microfluidic mixing; rigorous control over lipid ratios, particle size, and polydispersity [78]. |
| Bioanalytical & Quality Control | Developing sensitive, specific, and high-throughput methods to characterize ASO purity, stability, and metabolites in complex biological matrices [8]. | Employ a platform approach combining LC-MS, ligand-binding assays (LBA), and PCR-based methods tailored to the ASO's chemistry and intended target [8]. |
| Tissue-Specific Targeting | Achieving efficient delivery to extrahepatic tissues beyond the liver, which remains a major hurdle [77]. | Develop advanced bioconjugation strategies (e.g., GalNAc for liver targeting; antibodies, peptides for other tissues) and optimize nanocarrier surfaces for active targeting [8] [78]. |
| Regulatory & Cost | Navigating evolving regulatory guidelines for novel oligonucleotide modalities and maintaining cost-efficiency for large-scale GMP production [8]. | Early and close collaboration with regulatory agencies; development of robust, streamlined conjugation and purification techniques to reduce costs [8]. |
Bioanalytical Method Development for ASOs
Robust bioanalytical methods are essential for assessing the Absorption, Distribution, Metabolism, and Excretion (ADME) properties, pharmacokinetics (PK), pharmacodynamics (PD), and safety of ASO therapeutics [8]. The selection of a suitable platform depends on the specific data required.
Table 2: Bioanalytical Platforms for ASO Therapeutics in Drug Development
| Assay Platform | Key Principle | Advantages | Limitations | Typical LLOQ (Approved Drugs) |
|---|---|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Physical separation followed by mass-based detection [8]. | High specificity; can differentiate parent drug from metabolites; no need for analyte-specific reagents [8]. | Relatively lower sensitivity and throughput compared to other methods [8]. | ~1-20 ng/mL in plasma (e.g., Inclisiran: 10 ng/mL) [8]. |
| Ligand-Binding Assay (LBA) | Relies on capture and detection of ASO using binding partners (e.g., complementary oligonucleotides, antibodies) [8]. | High sensitivity and throughput [8]. | Lower specificity; may not distinguish between parent and metabolites with the same epitope [8]. | ~0.1-1 ng/mL (e.g., Inotersen: 1 ng/mL; Eplontersen: 0.129 ng/mL) [8]. |
| Polymerase Chain Reaction (PCR)-Based Assays | Amplification of ASO sequence after reverse transcription (e.g., SL RT-qPCR) [8]. | Very high sensitivity and throughput [8]. | Lower specificity; potential for amplification artifacts; cannot detect metabolites [8]. | Information not explicitly provided in sources. |
Application Note: Protocol for LC-MS Bioanalysis of ASOs in Plasma
This protocol outlines a standardized method for the quantification of ASOs in plasma using Liquid Chromatography coupled with Mass Spectrometry (LC-MS), a workhorse platform in oligonucleotide bioanalysis [8].
3.1.1. Principle ASOs are extracted from the plasma matrix, separated using liquid chromatography, and detected based on their mass-to-charge ratio (m/z). This method provides high specificity for the intact parent oligonucleotide and its major metabolites.
3.1.2. Research Reagent Solutions & Materials
Table 3: Essential Reagents and Materials for ASO LC-MS Bioanalysis
| Item | Function / Specification | Notes / Rationale |
|---|---|---|
| Solid-Phase Extraction (SPE) Plate | Anion-exchange or mixed-mode sorbents. | Efficiently captures negatively charged ASOs from plasma. Critical for achieving desired sensitivity [8]. |
| Internal Standard (IS) | Stable Isotope-Labeled (SIL)-ASO or close structural analog. | Corrects for variability in extraction efficiency and ionization. |
| Ammonium Hydroxyacetate Buffer | Volatile ion-pairing agent (e.g., 100 mM, pH 9.0). | Promotes chromatography separation; compatible with MS detection. |
| LC System | Ultra-High-Performance Liquid Chromatography (UHPLC). | Provides high-resolution separation. |
| Mass Spectrometer | Triple Quadrupole (QQQ) or High-Resolution Mass Spectrometer (HRMS). | QQQ for targeted quantification; HRMS for confident analyte identification. |
| Mobile Phase A | Water with volatile ion-pairing agent (e.g., 15 mM Triethylamine + 400 mM Hexafluoro-2-propanol). | Enables reverse-phase separation of ASOs. |
| Mobile Phase B | Methanol or Acetonitrile. | Organic solvent for elution. |
3.1.3. Step-by-Step Experimental Workflow
Sample Preparation (All steps on ice or at 4°C):
- Aliquot: Transfer 50-100 µL of plasma sample, calibration standard, and quality control (QC) sample to a 96-well plate.
- Spike IS: Add a fixed volume of the Internal Standard working solution to all samples (except blanks).
- Pre-treatment: Add a protein-precipitating agent (e.g., acetonitrile containing an amine) or a denaturing buffer to release protein-bound ASOs.
- Vortex and Centrifuge: Mix thoroughly and centrifuge to pellet precipitated proteins.
Solid-Phase Extraction:
- Condition: Condition the SPE sorbent with methanol followed by water or an equilibration buffer.
- Load: Transfer the supernatant from step 1 to the SPE plate.
- Wash: Wash with a buffer (e.g., 50-100 mM ammonium acetate, pH ~8) to remove salts and interfering compounds.
- Elute: Elute the ASOs using a small volume of an elution solvent (e.g., methanol/water with high salt concentration or pH shift).
LC-MS Analysis:
- Chromatography: Inject the eluent onto a UHPLC system equipped with a C18 or phenyl-hexyl column. Use a gradient of Mobile Phase A and B.
- Mass Spectrometry: Operate the mass spectrometer in negative ionization mode. Use Multiple Reaction Monitoring (MRM) for QQQ or monitor specific precursor ions for HRMS.
3.1.4. Data Analysis
- Plot the peak area ratio (Analyte/Internal Standard) against the nominal concentration of calibration standards to create a linear regression curve.
- Use this curve to back-calculate the concentration of ASO in unknown and QC samples.
- Assay acceptance is typically based on accuracy (85-115%) and precision (≤15% CV) of QCs.
The following workflow diagram illustrates the complete LC-MS bioanalysis protocol.
Bioconjugation for Targeted Delivery and Scalability
Bioconjugation is a critical strategy to overcome the inherent challenges of ASO delivery, such as rapid nuclease degradation and poor cellular uptake. It involves covalently attaching ligands to the ASO to enhance stability, facilitate uptake, and enable tissue-specific targeting [8] [78].
Common Bioconjugation Strategies
- GalNAc Conjugation: Attachment of N-acetylgalactosamine (GalNAc) targets the asialoglycoprotein receptor (ASGPR) on hepatocytes, enabling highly efficient liver delivery. This is a well-established approach for treating liver diseases [8] [78].
- Antibody-Oligonucleotide Conjugates (AOCs): Conjugation to antibodies allows for targeted delivery to specific cell types (e.g., tumor cells) by leveraging the antibody's antigen-binding specificity [8] [43].
- Lipid Conjugation: Adding lipid moieties (e.g., cholesterol) improves interaction with cell membranes, promotes cellular uptake through endocytosis, and protects from degradation [8].
- PEGylation: Conjugation with polyethylene glycol (PEG) increases solubility, prevents rapid renal elimination, and enhances the pharmacokinetic profile [8].
Protocol: Synthesis and Purification of GalNAc-Conjugated ASOs
This protocol describes a standard method for conjugating a trivalent GalNAc cluster to an ASO via a solid-phase synthesis and post-synthetic conjugation approach.
4.2.1. Principle The ASO is first synthesized on a solid support using standard phosphoramidite chemistry. A GalNAc cluster, pre-synthesized and activated, is then conjugated to the 5' end of the support-bound ASO, typically through a click chemistry reaction (e.g., strain-promoted alkyne-azide cycloaddition). The final conjugate is cleaved from the support, deprotected, and purified.
4.2.2. Research Reagent Solutions & Materials
- Solid Support: Controlled Pore Glass (CPG) support.
- Phosphoramidites: DNA/RNA phosphoramidites with standard (e.g., DMT-off) or necessary protecting groups.
- Activated GalNAc Cluster: e.g., a trivalent GalNAc ligand with an NHS ester or DBCO group.
- Conjugation Buffer: Anhydrous DMSO or an appropriate aqueous buffer (e.g., phosphate buffer, pH 8.5).
- Purification Systems: Analytical and Preparative High-Performance Liquid Chromatography (HPLC) systems with anion-exchange or reverse-phase columns.
- Desalting Columns: NAP columns or tangential flow filtration devices.
4.2.3. Step-by-Step Experimental Workflow
- ASO Synthesis: Synthesize the full-length ASO sequence on the solid support using an automated DNA/RNA synthesizer and standard phosphoramidite coupling cycles.
- On-Support Conjugation:
- After sequence synthesis, remove the 5'-DMT group to expose a primary amine or azide functionality.
- Wash the support and transfer it to a reaction vial.
- Dissolve the activated GalNAc cluster in conjugation buffer and add it to the support.
- React with agitation for 4-16 hours at room temperature.
- Cleavage & Deprotection:
- Wash the support to remove excess conjugation reagents.
- Cleave the ASO-GalNAc conjugate from the support and remove protecting groups using concentrated ammonium hydroxide at an elevated temperature (e.g., 55°C for 12-16 hours).
- Purification & Analysis:
- Purify: Use preparative HPLC to isolate the full-length conjugate from failure sequences and impurities.
- Desalt: Exchange the buffer into water or a volatile ammonium salt buffer using desalting columns or dialysis.
- Lyophilize: Freeze-dry the purified product to obtain a solid.
- Analyze: Confirm identity and purity using analytical HPLC, LC-MS, and UV spectrometry.
The strategic decision-making process for selecting and developing a bioconjugation strategy is summarized below.
The regulatory landscape for oligonucleotide therapeutics is still evolving. A proactive approach is essential for successful clinical translation. Key considerations include:
- Early Engagement: Collaborate closely with regulatory agencies (e.g., FDA, EMA) throughout the development process to align on chemistry, manufacturing, and controls (CMC) requirements [8].
- Comprehensive Characterization: Provide detailed information on the conjugation process, physicochemical characteristics, and potential safety concerns associated with chemical modifications [8].
- Tissue Pharmacokinetics: Emphasize tissue PK data in cases where plasma PK does not reflect therapeutic activity, as ASOs often act in specific tissues [8].
In conclusion, the scalable manufacturing and successful clinical translation of ASO therapeutics require a meticulous, integrated strategy that addresses challenges in synthesis, analytics, delivery, and regulation. By adopting the industry insights, best practices, and standardized protocols outlined in this document, researchers and developers can accelerate the development of these promising precision medicines, ensuring they are safe, efficacious, and accessible to patients.
Cost-Effectiveness and Accessibility in Rare Disease Treatment
Antisense oligonucleotides (ASOs) represent a transformative class of gene-silencing therapeutics that have revolutionized treatment prospects for rare genetic diseases. These short, synthetic nucleic acid strands modulate gene expression by binding to specific messenger RNA (mRNA) sequences, enabling precise targeting of disease-causing genes [79] [80]. The fundamental appeal of ASO technology lies in its ability to address previously "undruggable" targets, offering hope for conditions with significant unmet medical needs [80]. However, the development, manufacturing, and delivery of these sophisticated therapeutics present substantial challenges in cost-effectiveness and accessibility that must be addressed to maximize their patient impact. This application note provides researchers and drug development professionals with structured data, experimental protocols, and analytical frameworks to advance ASO therapeutics while navigating economic and accessibility constraints.
Market Landscape and Economic Analysis
The ASO therapeutics market demonstrates robust growth driven by technological advancements and increasing regulatory approvals. Understanding this landscape is crucial for strategic planning and resource allocation in research and development.
Table 1: Global ASO Therapeutics Market Projections
| Metric | 2024 Value | 2025 Value | 2032 Value | 2034 Value | CAGR (2025-2032/2034) |
|---|---|---|---|---|---|
| Market Size | USD 2.2 Billion [81] | USD 2.18 Billion [79] | USD 5.35 Billion [79] | USD 9.1 Billion [81] | 13.4% [79] |
Table 2: ASO Market Segmentation and Dominant Applications
| Segmentation Basis | Dominant Segment | Market Share/Rationale | Fastest-Growing Segment |
|---|---|---|---|
| Product Type | Modified ASOs [79] | 58% share; superior nuclease resistance & binding affinity [79] | Gapmers [79] |
| Therapeutic Application | Oncology [79] | Substantial investment & number of clinical trials [79] | Neurological Disorders [79] |
| Therapeutic Use | Rare Genetic Disorders [79] | Growing FDA orphan drug approvals [79] | Chronic Diseases [79] |
| Type of Therapy | Monotherapy [81] | Rise in regulatory approvals for monotherapy drugs [81] | Information Not Available |
| Geography | North America [79] [81] | >45% share; mature biotech ecosystem & strong funding [79] | Asia Pacific [79] |
Technological advancements are positively impacting production economics. Improvements in solid-phase synthesis technology have reportedly led to an approximately 15% reduction in overall manufacturing costs in 2025 compared to 2023 levels [79]. This trend is critical for enhancing the cost-effectiveness of ASO therapies, particularly for rare diseases with limited patient populations.
Experimental Protocols for ASO Development
Protocol: Preclinical Efficacy and Safety Assessment for Novel ASOs
Objective: To evaluate the gene silencing efficiency, mechanism of action, and preliminary toxicology of a novel ASO candidate in vitro.
Materials:
- Research Reagent Solutions: See Table 4 for a complete list.
- Equipment: Cell culture hood, CO₂ incubator, nano-spectrophotometer, electroporator/system for transfection, qRT-PCR machine, western blot apparatus, fluorescence microscope.
Methodology:
- ASO Design and Synthesis: Design ASO sequence (typically 15-25 bases) complementary to the target mRNA region. Incorporate chemical modifications (e.g., 2'-O-Methoxyethyl, Phosphorothioate backbone) to enhance stability and binding affinity [79]. Synthesize using solid-phase phosphoramidite chemistry [82] [83].
- Cell Culture: Maintain appropriate human cell lines (e.g., HEK293, HeLa) or patient-derived primary cells in recommended media with serum at 37°C and 5% CO₂.
- Transfection: Seed cells in 24-well plates at 70-80% confluence. The following day, transfert cells with a concentration gradient of the ASO (e.g., 10 nM, 50 nM, 100 nM) using a suitable transfection reagent. Include a scrambled-sequence ASO as a negative control and a well-characterized positive control ASO if available.
- RNA Isolation and qRT-PCR: 48 hours post-transfection, lyse cells and isolate total RNA. Synthesize cDNA and perform qRT-PCR using primers specific for the target gene and a housekeeping gene (e.g., GAPDH) to quantify mRNA expression levels relative to controls.
- Protein Analysis: 72 hours post-transfection, lyse cells for western blotting. Use antibodies against the target protein and a loading control (e.g., β-Actin) to confirm reduction at the protein level.
- Viability and Cytotoxicity Assessment: Perform an MTT or CellTiter-Glo assay alongside the transfection to assess cell viability. Measure lactate dehydrogenase (LDH) release in the culture supernatant as a marker of cytotoxicity.
Data Analysis: Calculate percentage mRNA and protein knockdown relative to scrambled control. Determine the half-maximal inhibitory concentration (IC₅₀) for the ASO. Correlate efficacy data with viability metrics to establish a preliminary therapeutic index.
Protocol: Intrathecal Delivery in Murine Models for Neurological Applications
Objective: To assess the biodistribution, efficacy, and tolerability of an ASO targeting a central nervous system (CNS) gene via intracerebroventricular (ICV) injection in a mouse model.
Materials:
- Animals: Transgenic or wild-type mice (e.g., SOD1 model for ALS [84]).
- ASO: Sterile, endotoxin-free ASO in artificial cerebrospinal fluid (aCSF).
- Equipment: Stereotaxic instrument, microinjection pump, Hamilton syringe, isoflurane anesthesia system, surgical tools.
Methodology:
- Pre-surgical Preparation: Anesthetize the mouse with isoflurane (3-4% for induction, 1-2% for maintenance). Secure the head in the stereotaxic frame. Maintain body temperature at 37°C.
- Stereotaxic Injection: Make a midline scalp incision and identify Bregma. Calculate coordinates for the lateral ventricle (e.g., -0.5 mm AP, ±1.0 mm ML from Bregma, -2.0 mm DV). Drill a burr hole carefully. Insert a 33-gauge needle connected to the microinjection pump.
- ASO Administration: Infuse the ASO solution (e.g., 10-50 µg in 5 µL aCSF) at a slow, constant rate (e.g., 1 µL/min). Leave the needle in place for an additional 5 minutes post-injection to prevent backflow. Withdraw the needle slowly. Suture the incision.
- Post-operative Care: Administer analgesic (e.g., buprenorphine) and allow the animal to recover on a warm pad. Monitor until fully ambulatory.
- Analysis: After a predetermined period (e.g., 4-8 weeks), euthanize the animals. Collect brain, spinal cord, and other organs (e.g., liver, kidney). Process tissues for:
- Molecular Analysis: Homogenize tissues to quantify ASO concentration (hybridization ELISA) and target engagement (mRNA/protein reduction).
- Histopathology: Fix tissues in formalin, section, and stain with H&E for general morphology and Nissl for neurons to assess signs of toxicity.
Data Analysis: Compare target mRNA/protein levels in the CNS of ASO-treated vs. aCSF-treated control animals. Evaluate ASO concentration in peripheral organs to assess off-target distribution. Correlate molecular findings with any observed behavioral or histopathological changes.
Visualization of Workflows and Pathways
The following diagrams outline key processes and considerations in the development and application of ASO therapeutics for rare diseases.
ASO Therapeutic Development Pipeline
Barriers to Rare Disease ASO Accessibility
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for ASO Research & Development
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Nucleoside Phosphoramidites | Building blocks for solid-phase oligonucleotide synthesis [82]. | Require high purity; availability of modified versions (2'-O-Me, LNA) is critical [82]. |
| Solid-Phase Synthesis Support | Insoluble polymer support (e.g., controlled-pore glass) for sequential nucleotide addition [82]. | |
| Transfection Reagents | Facilitate cellular uptake of ASOs in vitro (e.g., lipofectamine) [82]. | Optimization required for different cell lines; can impact cytotoxicity. |
| qRT-PCR Kits | Quantify mRNA expression levels to assess target engagement and silencing efficacy. | Must include reverse transcriptase and hot-start DNA polymerase. |
| Delivery System Components | Lipid nanoparticles (LNPs), GalNAc conjugates for in vivo delivery [79] [82]. | LNPs for tissue-agnostic delivery; GalNAc for hepatocyte-specific targeting. |
| HPLC/FPLC Systems | Purify and analyze synthetic oligonucleotides to ensure sequence fidelity and purity [82]. | Critical for therapeutic-grade ASOs; required for regulatory compliance. |
Advancing Accessibility: N-of-1 and Ultra-Rare Disease Protocols
For ultra-rare "nano-rare" diseases caused by unique genetic variants, conventional drug development is not economically viable. The N-of-1 trial paradigm represents a pioneering approach to address this unmet need.
Protocol: Framework for an Individualized ASO (N-of-1) Study
Objective: To develop, safety-test, and administer a patient-customized ASO for a single individual with a unique, disease-causing genetic variant [85].
Ethical and Regulatory Framework:
- Informed Consent: Obtain extensive, multi-stage informed consent that clearly distinguishes research from clinical care goals and emphasizes uncertainties [85].
- IRB/FDA Oversight: Submit protocol for approval by an Institutional Review Board (IRB) and the FDA under an expanded-access Investigational New Drug (IND) application [85].
- Funding and Resources: Secure funding (often through non-profits or crowdfunding) and assemble a multi-disciplinary team [85].
Methodology:
- Variant Identification: Confirm the pathogenic role of the unique genetic variant via whole-genome sequencing and functional studies.
- ASO Design and Screening: Design a panel of ASOs targeting the mutant allele. Screen for efficacy (e.g., using patient-derived cell lines or splicing assays) and selectivity over the wild-type allele [32].
- Preclinical Safety Testing: Conduct toxicology assessments in relevant cell models. If feasible, test in animals transgenic for the human target sequence [85].
- IND Application: Compile data on ASO characterization, preclinical efficacy, and safety for FDA review.
- Treatment and Monitoring: Administer the ASO (e.g., intrathecally) following an escalating dose regimen. Implement a rigorous safety monitoring protocol. Employ individualized, patient-centered outcome measures [85] [32].
- Data Collection and Sharing: Systematically collect data on safety and clinical outcomes. Report findings in peer-reviewed literature and clinical databases to contribute to scientific knowledge [85].
Visualization of the N-of-1 Process:
Individualized ASO (N-of-1) Workflow
The field of ASO therapeutics holds immense promise for treating rare diseases, but realizing its full potential requires a concerted effort to enhance cost-effectiveness and ensure equitable access. Strategies such as advancing synthesis technologies to reduce manufacturing costs, optimizing delivery systems to improve therapeutic indices, and developing ethical and scalable frameworks for ultra-rare diseases are paramount. Furthermore, navigating the evolving healthcare access landscape, including challenges posed by alternative funding programs and pharmacy benefit manager integration, is essential for ensuring that pioneering therapies can reach the patients who need them [86]. By integrating robust scientific methods with innovative access strategies, the research community can help translate the power of ASO technology into tangible benefits for all patients affected by rare diseases.
Proof of Concept: Validating ASO Performance and Comparing Therapeutic Modalities
The pharmaceutical industry is increasingly recognizing the limitations of traditional preclinical models, such as two-dimensional (2D) cell cultures and animal models, which often fail to faithfully recapitulate human-specific pathophysiology, contributing to high attrition rates in clinical trials [87]. In response, patient-derived organoids (PDOs) have emerged as a transformative technology that bridges the gap between conventional models and human physiology. These three-dimensional (3D) miniaturized structures that self-organize to mimic the architecture and functionality of native organs offer enhanced physiological relevance by preserving patient-specific genetic and phenotypic features [87] [88]. The recent FDA roadmap for reducing animal testing, which encourages alternative models within three to five years, provides regulatory impetus for this shift, confirming that human-relevant models can offer superior predictive power for drug development [89].
For research focusing on antisense oligonucleotides (ASOs) for gene silencing, PDOs present particularly valuable opportunities. ASOs are short, synthetic nucleic acids designed to modulate gene expression by targeting specific RNA transcripts through various mechanisms, including RNase H-mediated degradation and splice modulation [23] [12]. The ability of PDOs to maintain the genetic landscape of original patient tissue makes them ideally suited for validating ASO efficacy, optimizing chemical modifications, and identifying predictive biomarkers of response while accounting for human genetic diversity [87] [90]. This Application Note provides a comprehensive framework for integrating PDOs into preclinical validation pipelines for ASO therapeutics, offering structured protocols and analytical tools for researchers and drug development professionals.
Comparative Analysis of Preclinical Models
Key Characteristics of Patient-Derived Organoids vs. Animal Models
Table 1: Comparative analysis of patient-derived organoids and traditional animal models for preclinical validation.
| Feature | Patient-Derived Organoids (PDOs) | Traditional Animal Models |
|---|---|---|
| Physiological Relevance | Preserve patient-specific genetics, cellular heterogeneity, and tissue architecture [87] [88] | Species-specific differences in genetics, physiology, and immune system [89] |
| Human Disease Modeling | Directly derived from human patient tissue; excellent for human-specific pathology [87] [90] | Require genetic engineering or xenotransplantation; may not fully mimic human disease [89] |
| Throughput & Scalability | Suitable for medium-to-high throughput screening; biobanking possible [87] [88] | Low throughput; time-consuming and expensive [88] |
| Timeline & Cost | Rapid establishment (weeks); lower cost per model [88] | Long breeding and experimentation cycles; high maintenance costs [88] |
| Tumor Microenvironment | Can be co-cultured with immune cells/stroma but requires advanced engineering [87] [88] | Intact native microenvironment but is of animal origin [88] |
| ASO Therapeutic Validation | Direct human target validation; study of human-specific splicing events [12] [91] | Off-target effects may not be human-relevant; differences in RNA processing [23] |
| Regulatory Acceptance | Gaining traction with FDA's push for human-relevant models [89] | Current gold standard but facing ethical and translational pressure [89] |
Advantages of PDOs in ASO Research
The application of PDOs in ASO research provides distinct advantages for therapeutic development. Unlike conventional cell lines that adapt to 2D culture and lose original biological characteristics, organoids maintain the genetic and cellular makeup of a patient's tissue, enabling more accurate assessment of ASO binding affinity and specificity for human targets [89]. For diseases caused by specific genetic variants, PDOs enable personalized therapeutic testing, as demonstrated by their use in predicting patient responses to cystic fibrosis treatments targeting rare mutations [89]. Furthermore, PDOs facilitate the study of splice-modulating ASOs in a human physiological context, preserving native splicing machinery and enabling functional assessment of exon skipping or inclusion strategies [12].
Application Notes: Integrating PDOs into ASO Preclinical Validation
Establishing PDOs for ASO Testing
Patient-Derived Organoid Biobanks: The generation of living biobanks from healthy and diseased tissue serves as a repository of patient avatars for ASO screening and toxicology studies [89]. These biobanks better capture the diversity and complexity of human health and disease than animal models, enabling researchers to assess ASO efficacy across diverse genetic backgrounds [89] [87]. For oncology applications, patient-derived tumor organoids (PDTOs) retain histological and genomic features of original tumors, including intratumoral heterogeneity and drug resistance patterns, making them invaluable for testing ASOs designed to target specific oncogenic drivers or resistance mechanisms [87] [88].
Cryopreservation and Quality Control: Organoids can be cryopreserved while maintaining viability and functionality, enabling the creation of reproducible assay systems for standardized ASO testing [89]. Robust quality control measures are essential and should include genomic sequencing to confirm the presence of target mutations or polymorphisms, immunohistochemistry to verify tissue-specific marker expression, and functional assays to validate physiological responses [87] [90].
Experimental Design for ASO Validation
Dose-Response Studies: PDOs enable precise quantification of ASO potency through comprehensive dose-response curves. Treatment typically spans 24-96 hours, with concentration ranges varying based on ASO chemistry and delivery efficiency [27]. Key metrics include IC₅₀ values for knockdown efficiency or EC₅₀ for splice-switching outcomes, providing critical data for lead ASO selection and dosage prediction for in vivo studies [12] [27].
Temporal Response Assessment: The stability of ASO effects can be evaluated through extended culture timelines, with monitoring of target gene expression and functional recovery post-treatment. This is particularly relevant for ASOs with chemical modifications designed to enhance duration of action, such as phosphorothioate backbones and 2'-O-methoxyethyl (2'-MOE) modifications [23] [27].
Combinatorial Treatment Strategies: PDO platforms are ideal for testing ASOs in combination with standard-of-care therapeutics, especially in oncology. For example, organoids derived from treatment-resistant tumors can assess whether ASO-mediated knockdown of resistance genes resensitizes tumors to conventional chemotherapy [87] [88].
Analytical Approaches for ASO Efficacy Assessment
Table 2: Key analytical methods for evaluating ASO efficacy in patient-derived organoids.
| Analysis Type | Methodology | Application in ASO Testing | Key Outcome Measures |
|---|---|---|---|
| Molecular Analysis | RT-qPCR, RNA-seq [27] | Quantify target mRNA knockdown or splice variant changes | mRNA expression levels, % splice correction |
| Protein Analysis | Western blot, Immunofluorescence [91] | Confirm reduction in target protein or detection of modified protein | Protein expression levels, subcellular localization |
| Functional Assays | Cell viability, apoptosis, migration assays [87] | Assess phenotypic consequences of ASO treatment | IC₅₀ values, apoptosis rate, functional recovery |
| Morphological Analysis | Histology, 3D imaging [89] [88] | Evaluate tissue-level effects and structural preservation | Organoid size, lumen formation, architecture |
| Biochemical Assays | Metabolomics, enzyme activity tests [87] | Detect downstream metabolic or enzymatic changes | Metabolite levels, pathway activity restoration |
Experimental Protocols
Protocol 1: Evaluating Gapmer ASO-Mediated Knockdown in PDOs
Principle: Gapmer ASOs contain a central DNA core flanked by modified nucleotides (e.g., 2'-MOE, LNA) that recruit RNase H to cleave complementary target mRNA, reducing gene expression [23] [27]. This protocol is suitable for targeting genes with toxic gain-of-function mutations [12].
Materials:
- Patient-derived organoids (e.g., intestinal, hepatic, or tumor organoids)
- Gapmer ASO with phosphorothioate backbone and appropriate chemical modifications [27]
- Transfection reagent compatible with 3D cultures
- Organoid culture medium with appropriate growth factors [87] [90]
- Lysis buffer for RNA/protein extraction
Procedure:
- Organoid Preparation: Dissociate PDOs into single cells or small clusters (3-10 cells) using enzymatic digestion [87].
- ASO Transfection:
- Seed 10,000-50,000 cells per well in 96-well U-bottom plates
- Complex ASO with transfection reagent in serum-free medium (0.1-100 nM final concentration)
- Incubate with organoids for 4-6 hours, then replace with complete medium
- Culture and Maintenance:
- Maintain organoids in appropriate 3D culture matrix (e.g., Matrigel)
- Refresh medium every 2-3 days
- Harvest organoids at 24, 48, 72, and 96 hours post-transfection
- Downstream Analysis:
- Extract RNA for RT-qPCR to quantify target mRNA reduction
- Process for protein analysis at 72-96 hours to assess knockdown efficiency
- Perform functional assays based on target gene function
Protocol 2: Testing Splice-Switching ASOs in PDOs
Principle: Splice-switching ASOs (ssASOs) are typically fully modified oligonucleotides (e.g., 2'-OMe, PMO) that sterically block splicing regulatory elements without activating RNase H, redirecting pre-mRNA processing to exclude or include specific exons [23] [12]. This approach is valuable for restoring reading frames in diseases like Duchenne muscular dystrophy or skipping exons containing deleterious mutations [12].
Materials:
- Disease-specific PDOs harboring splicing mutations
- Splice-switching ASOs with 2'-OMe, PMO, or PNA chemistry [23] [12]
- Appropriate delivery reagents (e.g., electroporation equipment for PMOs)
- RNA extraction kit with DNase treatment
- RT-PCR reagents for splice variant analysis
Procedure:
- Organoid Preparation: Establish PDOs from patients with target splicing mutations; confirm aberrant splicing pattern by RNA analysis [87].
- ASO Delivery:
- For charged ASOs (e.g., 2'-OMe PS): Use lipid-based transfection as in Protocol 1
- For neutral ASOs (e.g., PMO, PNA): Use electroporation or specialized peptide-based delivery
- Include negative control ASO with scrambled sequence
- Culture Conditions:
- Maintain transfected organoids for 5-10 days to allow protein turnover
- Refresh medium every 2-3 days
- Sample organoids at multiple time points to assess persistence of splicing correction
- Splicing Analysis:
- Extract high-quality RNA, treat with DNase
- Perform RT-PCR across the target exon/intron region
- Analyze products by capillary electrophoresis or sequencing to quantify corrected vs. aberrant splicing
- Assess functional protein expression by Western blot or immunofluorescence when possible
Protocol 3: Toxicological Assessment of ASOs in Normal PDOs
Principle: Normal tissue-derived organoids provide a human-relevant system for evaluating ASO safety, detecting sequence-dependent off-target effects or chemical modification-related toxicity [89] [87].
Materials:
- Normal organoids from target tissue (e.g., hepatocyte, renal, cardiac organoids)
- ASO candidates and appropriate controls
- Cell viability assay reagents (e.g., ATP-based assays)
- Histology materials for structural assessment
- Clinical chemistry analyzers for organ-specific markers
Procedure:
- Organoid Establishment: Generate organoids from healthy human tissue sources [87].
- ASO Exposure:
- Treat organoids with ASOs across a concentration range (0.1-100 μM)
- Include multiple biological replicates
- Maintain for 7-14 days with periodic re-dosing to simulate chronic exposure
- Toxicity Endpoint Assessment:
- Viability Metrics: Measure ATP content, organoid size quantification
- Morphological Assessment: Process for histology (H&E staining) and immunohistochemistry for tissue-specific markers
- Functional Assessment: Measure organ-specific functions (e.g., albumin production for hepatocytes, beat rate for cardiomyocytes)
- Transcriptomic Analysis: Perform RNA-seq to identify off-target effects and pathway disturbances
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents and solutions for ASO testing in patient-derived organoids.
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| ASO Chemistries | Phosphorothioate backbones, 2'-MOE, 2'-OMe, LNA, PMO [23] [27] | Enhance nuclease resistance, binding affinity, and cellular uptake; different chemistries suit various mechanisms |
| Delivery Systems | Lipid nanoparticles, electroporation systems, cell-penetrating peptides [12] | Facilitate ASO entry into organoid cells; method choice depends on ASO chemistry and organoid type |
| Organoid Culture Matrices | Matrigel, collagen-based hydrogels, synthetic scaffolds [87] [90] | Provide 3D environment that supports organoid growth and polarization |
| Cell Culture Media | Intestinal stem cell media, hepatocyte culture media, tumor organoid media [89] [87] | Tissue-specific formulations containing essential growth factors and nutrients |
| Analysis Reagents RNase H activity assays, splicing reporter systems, apoptosis detection kits [23] [27] | Enable mechanistic studies and functional assessment of ASO effects |
Visualizing Experimental Workflows and ASO Mechanisms
Workflow for ASO Validation Using Patient-Derived Organoids
ASO Mechanisms of Action in Organoid Models
Patient-derived organoids represent a paradigm shift in preclinical validation for ASO therapeutics, offering human-relevant systems that complement and increasingly reduce reliance on traditional animal models. By preserving the genetic landscape and cellular heterogeneity of patient tissues, PDOs enable more accurate assessment of ASO efficacy, safety, and mechanism of action. The protocols and analytical frameworks presented in this Application Note provide researchers with practical tools to integrate PDOs into their ASO development pipelines, potentially enhancing translational predictability while aligning with ethical principles and regulatory trends favoring human-relevant testing platforms [89] [87]. As organoid technology continues to evolve with improvements in standardization, scalability, and microenvironment complexity, its role in de-risking ASO therapeutic development is poised to expand significantly.
Within the development of antisense oligonucleotides (ASOs), the rigorous analysis of clinical trial efficacy and safety outcomes is paramount. ASOs are short, synthetic molecules designed to bind to specific RNA sequences, modulating gene expression through mechanisms such as RNA degradation or splice modulation [12] [92]. Their clinical success hinges on a robust evaluation framework that accurately measures intended therapeutic effects (efficacy) and monitors adverse events (safety). This document outlines detailed application notes and protocols for analyzing these critical outcomes, contextualized specifically for ASO-based therapeutics in gene silencing research. The structured approaches described herein are designed to meet the needs of researchers, scientists, and drug development professionals navigating the complexities of oligonucleotide drug development.
Data Presentation: Frameworks for Efficacy and Safety
Effective data presentation is crucial for interpreting clinical trial results. The selection of appropriate visual displays significantly impacts how healthcare providers comprehend information, with studies showing that comprehension of complex data varies significantly depending on the format used [93].
Quantitative Data Tables for Clinical Outcomes
Structured tables provide a foundational element for clear data communication. The following tables exemplify standard formats for presenting efficacy and safety data from ASO clinical trials.
Table 1: Efficacy Outcomes from a Hypothetical ASO Clinical Trial
| Outcome Measure | Intervention Group (n=100) | Comparator Group (n=100) | P-value | Statistical Method |
|---|---|---|---|---|
| Primary Endpoint | ||||
| ≥50% Target Protein Reduction | 68% | 22% | <0.0001 | Chi-square |
| Mean Change in Biomarker (SD) | -45.2 (12.1) | -5.3 (18.7) | <0.001 | ANCOVA |
| Secondary Endpoints | ||||
| Clinical Response Score | 7.2 (1.5) | 4.1 (2.2) | 0.003 | Mixed Model Repeated Measures |
| Patient-Reported Improvement | 65% | 28% | 0.015 | Logistic Regression |
Table 2: Safety Profile Summary from a Hypothetical ASO Clinical Trial
| Adverse Event Category | Intervention Group (n=100) | Comparator Group (n=100) | Severity Grade 3+ (%) |
|---|---|---|---|
| Overall AEs | 75% | 72% | 8% |
| Treatment-Related AEs | 45% | 42% | 5% |
| Serious Adverse Events (SAEs) | 12% | 10% | 12% |
| Most Common AEs | |||
| Injection Site Reaction | 25% | 8% | 2% |
| Fever | 15% | 12% | 1% |
| Fatigue | 18% | 16% | 0% |
| AEs Leading to Discontinuation | 5% | 4% | 5% |
Table 3: Essential Research Reagents for ASO Bioanalysis
| Reagent / Solution | Function in ASO Research | Application Example |
|---|---|---|
| LC-MS/MS Systems | High-specificity quantification of ASOs and their metabolites | Pharmacokinetic analysis of parent ASO in plasma and tissues [8] |
| Ligand-Binding Assay (LBA) Kits | High-sensitivity detection of oligonucleotides | Measuring low-concentration ASO levels in biological matrices [8] |
| Stem-loop RT-qPCR Reagents | Highly sensitive amplification-based ASO detection | Quantifying siRNA molecules in tissue samples [8] |
| Solid-Phase Extraction Cartridges | Sample purification and concentration prior to analysis | Clean-up of plasma samples for LC-MS analysis [8] |
| GalNAc Conjugation Reagents | Targeted delivery to hepatocytes | Enhancing liver-specific uptake of siRNA therapeutics [8] |
| Stable Isotope-Labeled ASO Standards | Internal standards for mass spectrometry | Accurate quantification via LC-MS/MS [8] |
Experimental Protocols
Protocol 1: Bioanalytical Method for ASO Quantification
Principle: This protocol describes the quantification of ASO concentrations in biological matrices using liquid chromatography-mass spectrometry (LC-MS), a preferred platform for its ability to differentiate between parent ASO and metabolites [8].
Materials:
- LC-MS/MS system with electrospray ionization
- Solid-phase extraction plates
- Stable isotope-labeled internal standard
- Mobile phase A: 10mM hexafluoro-2-propanol/triethylamine in water
- Mobile phase B: Methanol
- Tissue homogenizer (for tissue distribution studies)
Procedure:
- Sample Collection: Collect plasma, urine, or tissue samples at predetermined time points. For tissues, homogenize in appropriate buffer (e.g., phosphate-buffered saline).
- Sample Extraction:
- Aliquot 100 µL of plasma or tissue homogenate into a microcentrifuge tube.
- Add 20 µL of internal standard working solution.
- Precipitate proteins with 300 µL of acetonitrile.
- Vortex mix for 1 minute and centrifuge at 15,000 × g for 10 minutes.
- Solid-Phase Extraction:
- Load supernatant to pre-conditioned SPE cartridges.
- Wash with 1 mL 5% methanol in water.
- Elute ASO with 0.5 mL 80% methanol in water.
- Evaporate eluent under nitrogen at 40°C and reconstitute in 100 µL water.
- LC-MS/MS Analysis:
- Column: C18, 2.1 × 50 mm, 2.6 µm
- Gradient: 10-90% Mobile phase B over 5 minutes
- Flow rate: 0.4 mL/min
- Detection: Multiple reaction monitoring (MRM) in negative ion mode
- Data Analysis: Calculate ASO concentrations using the internal standard method with a calibration curve (1-1000 ng/mL).
Validation Parameters: Establish specificity, sensitivity (LLOQ), accuracy, precision, matrix effects, and stability according to regulatory guidelines [8].
Protocol 2: Analysis of Splice-Modulating ASO Efficacy
Principle: This protocol assesses the efficacy of splice-switching ASOs (ssASOs) by measuring alternative splicing patterns in treated cells or tissues using RT-PCR analysis [12].
Materials:
- Cell line or patient-derived cells with target mutation
- ssASO and scrambled control ASO
- RNA extraction kit
- Reverse transcription reagents
- PCR master mix
- Agarose gel electrophoresis system or capillary electrophoresis instrument
Procedure:
- ASO Treatment:
- Seed cells in 6-well plates at 300,000 cells/well.
- Transfect with 100 nM ssASO using appropriate transfection reagent.
- Include untreated and scrambled ASO controls.
- Incubate for 48 hours at 37°C, 5% CO₂.
- RNA Isolation:
- Extract total RNA using commercial kits.
- Quantify RNA concentration by spectrophotometry.
- Reverse Transcription:
- Use 1 µg total RNA for cDNA synthesis with reverse transcriptase.
- Apply gene-specific primers or random hexamers.
- PCR Amplification:
- Design primers flanking the targeted exon.
- Set up PCR reactions with 2 µL cDNA template.
- Run 35 cycles with appropriate annealing temperature.
- Product Analysis:
- Separate PCR products by agarose gel electrophoresis or capillary electrophoresis.
- Quantify band intensities using imaging software.
- Data Calculation:
- Calculate exon inclusion rate as: (Intensity of inclusion band / Total intensity of all bands) × 100
- Compare inclusion rates between ssASO-treated and control samples.
Validation: Confirm splicing changes by Sanger sequencing of PCR products or quantitative RT-PCR with isoform-specific probes.
Visualizing Clinical Trial Data Flow and ASO Mechanisms
Clinical Trial Data Analysis Workflow
Clinical Trial Data Analysis Pipeline
ASO Mechanisms of Action in Clinical Outcomes
ASO Mechanisms and Clinical Outcome Assessment
Advanced Analytical Approaches
Structured Data Representation for Evidence Synthesis
Modern clinical trial analysis extends beyond traditional statistical approaches. The creation of structured datasets that link efficacy with safety results at the experimental arm group level enables more comprehensive evidence synthesis [94]. This approach facilitates:
- Dual-faceted understanding of interventions through simultaneous evaluation of efficacy and safety
- Cross-trial comparisons through standardized data representation
- Knowledge graph construction that connects studies, interventions, outcomes, and results
- Incorporation of both positive and negative results to minimize publication bias
This finer-grained representation of clinical trial results moves beyond the traditional PICO framework to create computable evidence structures that can be reused for systematic reviews and health technology assessments [94].
ASO-Specific Pharmacokinetic Considerations
The analysis of ASO clinical trials requires special consideration of their unique pharmacokinetic properties:
- Tissue distribution is more relevant than plasma levels for many ASO therapeutics [8]
- Metabolite identification requires specialized bioanalytical approaches
- Long tissue half-lives enable extended dosing intervals but complicate safety monitoring
- Conjugation strategies (e.g., GalNAc) significantly alter distribution patterns and must be accounted for in outcome analyses [8]
These properties necessitate tailored statistical plans and outcome measurement schedules that differ from those used for traditional small molecule drugs.
The rigorous analysis of efficacy and safety outcomes in ASO clinical trials requires specialized methodologies that account for their unique mechanisms of action and pharmacokinetic properties. By implementing the structured data presentation formats, experimental protocols, and analytical workflows described in this document, researchers can generate robust evidence to advance ASO therapeutics through the drug development pipeline. The integration of modern data science approaches, including structured results databases and knowledge graphs, further enhances the utility of clinical trial data for evidence synthesis and informed decision-making in oligonucleotide-based drug development.
Antisense oligonucleotides (ASOs) and small interfering RNAs (siRNAs) represent two pivotal classes of molecules in gene silencing research and therapeutic development. Both are synthetic oligonucleotides designed to hybridize with target RNA sequences through Watson-Crick base pairing, yet they leverage fundamentally distinct biological pathways and possess unique pharmacological characteristics [6] [95]. ASOs are single-stranded DNA or RNA molecules typically ranging from 15-25 nucleotides in length, while siRNAs are double-stranded RNA molecules generally 19-23 base pairs long [95] [96]. The choice between these platforms significantly impacts experimental design, delivery strategies, and potential applications, making a thorough comparative analysis essential for research and drug development professionals working in antisense gene silencing.
Fundamental Mechanisms of Action
ASO-Mediated Gene Silencing
ASOs function through multiple mechanistic pathways based on their design and chemical properties. The primary mechanism for many therapeutic ASOs involves RNase H1-mediated degradation [95] [23]. These ASOs, typically designed as "gapmers," form DNA-RNA heteroduplexes with their target mRNA, recruiting the ubiquitous enzyme RNase H1 which cleaves the RNA strand [23]. This cleavage renders the mRNA untranslatable and leads to its degradation. Alternatively, ASOs can act through steric blockade mechanisms, where binding to specific mRNA regions physically obstructs ribosomal scanning or splice site recognition without degrading the RNA [95] [23]. This approach is particularly valuable for splice-switching applications, such as with nusinersen (Spinraza) for spinal muscular atrophy, where ASO binding modulates pre-mRNA splicing to promote production of functional protein [5] [97].
siRNA-Mediated RNA Interference
siRNAs operate exclusively through the RNA interference (RNAi) pathway [95] [5]. These double-stranded molecules are loaded into the RNA-induced silencing complex (RISC) within the cytoplasm. The complex undergoes activation through adenosine triphosphate-dependent unwinding, discarding the passenger strand while retaining the guide strand [6] [5]. The activated RISC then uses this guide strand to scan for complementary mRNA sequences. Upon perfect complementarity, the Argonaute 2 (Ago2) protein within RISC cleaves the target mRNA, enabling catalytic recycling of RISC for multiple rounds of silencing [6] [5]. This mechanism provides potent, sustained gene silencing even at low intracellular concentrations.
Structural and Chemical Properties
The structural differences between single-stranded ASOs and double-stranded siRNAs fundamentally influence their physicochemical behaviors and pharmacological optimization strategies [6].
Table 1: Comparative Structural Properties of ASOs and siRNAs
| Property | ASOs | siRNAs |
|---|---|---|
| Structure | Single-stranded | Double-stranded |
| Typical Length | 15-25 nucleotides [95] | 19-23 base pairs [96] |
| Molecular Weight | ~5-8 kDa | ~13 kDa [6] [55] |
| Hydrophobicity | More hydrophobic due to single-stranded flexibility [6] | Highly hydrophilic, behaves as rigid rods [6] |
| Chemical Modification Scope | Broad - virtually every position can be modified [6] | Limited by RISC and Ago2 structural requirements [6] |
| Common Modifications | Phosphorothioate backbones, 2'-O-methyl, 2'-MOE, LNA [23] [97] | Limited 2'-modifications (methoxy, fluoro), selective PS modifications [6] |
ASOs offer greater flexibility for extensive chemical modifications due to their single-stranded nature and lack of protein complex loading requirements. Almost every position not involved in Watson-Crick base pairing can be chemically optimized to enhance nuclease resistance, binding affinity, and pharmacokinetic properties [6] [23]. In contrast, siRNAs face significant constraints because they must be recognized by the RISC loading complex and fit within the Ago2 catalytic center. The phosphate on the sense strand is essential for binding to Ago2's phosphate-binding pocket, and 2' modifications are restricted to specific sites with primarily methoxy and fluoro groups being tolerated [6].
Pharmacokinetics and Delivery Considerations
Delivery challenges represent significant hurdles for both ASO and siRNA platforms, though the specific obstacles differ based on their distinct physicochemical properties [6] [55].
Table 2: Pharmacokinetic and Delivery Properties
| Parameter | ASOs | siRNAs |
|---|---|---|
| Systemic Distribution | Broad tissue distribution (liver, kidney, fat, bone marrow) [6] | Limited without delivery systems; rapid renal clearance [6] |
| CNS Penetration | Broad distribution after intrathecal administration [6] | Enhanced CNS distribution possible with intrathecal administration [6] |
| Primary Delivery Strategies | Chemical modifications, conjugates (GLP1 analogs, transferrin receptors) [6] | GalNAc conjugation, lipid nanoparticles (LNPs) [6] [8] |
| GalNAc Conjugation Impact | Does not alter bulk distribution; increases hepatocyte potency 20-30 fold [6] | Dramatically increases bulk delivery to liver [6] |
| Administration Routes | Subcutaneous, intravenous, intrathecal, intravitreal [97] | Primarily subcutaneous (GalNAc-conjugates), intravenous (LNP) [6] |
Unmodified siRNAs face rapid renal clearance due to their relatively small size and hydrophilic nature, necessitating delivery systems for therapeutic efficacy [6] [55]. Early siRNA therapies utilized lipid nanoparticles (LNPs), which enabled hepatic delivery but required intravenous administration and sometimes provoked inflammatory responses [6]. The advent of GalNAc conjugation revolutionized siRNA therapeutics by enabling subcutaneous administration and targeted hepatocyte delivery through the asialoglycoprotein receptor [6] [8]. In contrast, phosphorothioate-modified ASOs exhibit favorable pharmacokinetics, binding serum proteins to resist renal clearance and achieving broad tissue distribution [6] [23]. While GalNAc conjugation enhances ASO potency in hepatocytes, it doesn't fundamentally alter their tissue distribution profile [6].
Research Reagent Solutions
Successful gene silencing experiments require careful selection of reagents and delivery systems tailored to each oligonucleotide platform.
Table 3: Essential Research Reagents and Their Applications
| Reagent Category | Specific Examples | Function and Applications |
|---|---|---|
| Chemical Modification Kits | Phosphorothioate, 2'-O-methyl, 2'-MOE, LNA [23] [97] | Enhance nuclease resistance, binding affinity, and cellular uptake |
| Delivery Systems | Lipid nanoparticles (LNPs), GalNAc conjugates, cell-penetrating peptides [8] [55] | Protect oligonucleotides from degradation and facilitate cellular internalization |
| Control Oligonucleotides | Scrambled sequences, mismatch controls, non-targeting siRNAs [96] | Essential for distinguishing specific silencing from non-specific effects |
| Transfection Reagents | Cationic lipids, dendrimers, polymers [98] | Facilitate cellular uptake of oligonucleotides in cell culture systems |
| Analytical Tools | LC-MS/MS, RT-qPCR, Western blot, ligand-binding assays [8] | Quantify oligonucleotide concentrations and evaluate target engagement |
| Validated Oligonucleotides | Nusinersen, eteplirsen, patisiran, givosiran analogs [97] | Benchmark compounds with established performance characteristics |
Experimental Protocols
Protocol 1: In Vitro Gene Silencing in Cell Culture
Objective: Evaluate ASO or siRNA-mediated knockdown of target mRNA and protein in mammalian cell lines.
Materials:
- Custom-designed ASO (gapmer design) or siRNA duplex
- Appropriate control oligonucleotides (scrambled or mismatched sequences)
- Cell culture reagents and appropriate cell line
- Transfection reagent (e.g., cationic lipid-based)
- RNA isolation kit, RT-qPCR reagents
- Western blot equipment and antibodies
Procedure:
- Oligonucleotide Design: Design ASO gapmers with 8-10 DNA nucleotides flanked by 2-5 chemically modified nucleotides (e.g., 2'-MOE, LNA) [23]. Design siRNA duplexes with 19-21 bp including 2-nt 3' overhangs.
- Cell Seeding: Seed cells in 24-well plates at 30-50% confluence in appropriate medium without antibiotics 24 hours before transfection.
- Transfection Complex Formation:
- Dilute ASO or siRNA in serum-free medium (50-100 nM final concentration)
- Dilute transfection reagent separately in serum-free medium
- Combine diluted oligonucleotide with diluted transfection reagent (1:1 ratio)
- Incubate 15-20 minutes at room temperature
- Transfection: Add complexes to cells dropwise. Include untransfected and negative control oligonucleotide treatments.
- Incubation: Incubate cells 24-72 hours at 37°C, 5% CO₂.
- Analysis:
- Harvest cells 24-48h post-transfection for mRNA analysis by RT-qPCR
- Harvest cells 48-72h post-transfection for protein analysis by Western blot
- Include housekeeping genes/proteins for normalization
Troubleshooting: Optimize oligonucleotide concentration (typically 1-100 nM), transfection reagent ratio, and timing based on target turnover rate. Include multiple controls to distinguish sequence-specific effects from non-specific immune activation [23] [96].
Protocol 2: In Vivo Administration and Tissue Analysis
Objective: Assess gene silencing efficacy of ASOs or siRNAs in animal models.
Materials:
- Chemically modified ASO or GalNAc-conjugated siRNA
- Sterile saline or formulation buffer
- Appropriate animal model (e.g., mice, rats)
- Surgical equipment for intrathecal administration (if needed)
- Tissue collection supplies and preservation tools
- Bioanalytical equipment (LC-MS/MS, PCR systems)
Procedure:
- Oligonucleotide Preparation:
- Dosing Regimen:
- Administration:
- Tissue Collection:
- Euthanize animals at predetermined timepoints (e.g., 24h, 72h, 1-2 weeks)
- Collect target tissues (liver, kidney, etc.) and flash-freeze in liquid nitrogen
- Preserve tissues at -80°C until analysis
- Tissue Analysis:
- Homogenize tissues in appropriate buffers
- Extract total RNA for target mRNA quantification by RT-qPCR
- Analyze oligonucleotide concentration using LC-MS/MS [8]
- For protein analysis, use Western blot or ELISA
Troubleshooting: For tissue distribution studies, utilize radiolabeled or fluorescently tagged oligonucleotides. Consider species-specific differences in pharmacokinetics and immune recognition [8].
Therapeutic Applications and Clinical Translation
The distinct mechanisms and properties of ASOs and siRNAs make them suitable for different therapeutic applications. ASOs offer particular advantages for applications requiring nuclear activities such as splice modulation, with demonstrated success in treating neurological disorders like spinal muscular atrophy (nusinersen) and Duchenne muscular dystrophy (eteplirsen, golodirsen) [5] [97]. Their ability to access both nuclear and cytoplasmic compartments and leverage multiple mechanisms of action expands their therapeutic versatility [6]. siRNAs excel in cytoplasmic gene silencing applications, particularly for hepatocyte targets, with approved therapies for conditions including hereditary transthyretin-mediated amyloidosis (patisiran), acute hepatic porphyria (givosiran), and hypercholesterolemia (inclisiran) [8] [5]. The catalytic nature of RISC-mediated silencing and durable effect (months) with single doses represent significant advantages for chronic diseases requiring long-term gene suppression [6] [5].
ASOs and siRNAs offer complementary approaches for gene silencing research and therapeutic development. ASOs provide greater mechanistic versatility, broader tissue distribution, and superior capabilities for nuclear targets and splice modulation. siRNAs deliver highly potent, catalytic cytoplasmic silencing with potential for longer duration effects, particularly for hepatocyte targets. The choice between platforms should be guided by target biology, subcellular localization, desired mechanism, and delivery requirements. Continuing advances in chemical modifications, delivery technologies, and sequence design algorithms are rapidly expanding the utility of both platforms beyond current limitations, promising new treatments for previously undruggable targets across diverse disease areas [6] [99].
For decades, drug discovery has been constrained by the limitations of small molecule therapeutics, which predominantly target proteins with defined binding pockets. This approach leaves approximately 80% of disease-causing proteins, considered 'undruggable,' beyond therapeutic reach [100]. Antisense oligonucleotides (ASOs) represent a transformative class of therapeutics that overcome this fundamental limitation by targeting the RNA and DNA that control protein production [11] [100].
ASOs are short, synthetic single-stranded oligonucleotides, typically 15-30 nucleotides in length, designed to bind to complementary RNA sequences through Watson-Crick base pairing [11] [101]. This mechanism enables precise modulation of gene expression at the RNA level, fundamentally differing from traditional small molecule drugs that interact with proteins after they have been synthesized [102] [100]. The programmable nature of ASOs allows researchers to target virtually any gene with high specificity, unlocking therapeutic opportunities across the entire genome [103] [100].
This application note details the comparative advantages of ASOs over small molecule drugs, provides quantitative comparisons, and outlines essential experimental protocols for researchers developing ASO-based therapies targeting previously undruggable pathways.
Comparative Analysis: ASOs vs. Small Molecule Drugs
Fundamental Advantages of ASOs
Table 1: Fundamental Characteristics of ASOs vs. Small Molecule Drugs
| Property | Small Molecule Drugs | Antisense Oligonucleotides (ASOs) |
|---|---|---|
| Molecular Weight | Usually <500 Da [102] | Usually >7 kDa [102] |
| Primary Targets | Proteins (typically with active sites) [102] [100] | RNA molecules (mRNA, pre-mRNA, non-coding RNAs) [102] [103] |
| Target Scope | ~15% of the proteome ("druggable") [103] | Theoretical access to 100% of the genome and transcriptome [11] [103] |
| Design Basis | Empirical screening; often serendipitous [102] | Rational design based on sequence complementarity [102] |
| Development Timeline | Typically longer [102] | Shorter development cycles [102] |
| Specificity | Moderate; potential for off-target toxicity [102] | High; sequence-specific binding [102] [103] |
ASOs provide strategic advantages that make them particularly suitable for targeting previously undruggable pathways. Unlike small molecules that require specific protein structures for binding, ASOs can be programmed to target any RNA sequence with high specificity [103]. This rational design process significantly reduces the blind spots encountered in conventional drug discovery [102]. Furthermore, ASOs can target non-coding RNAs, which represent the vast majority of transcriptional output and were previously considered untargetable [103].
Mechanisms of Action and Therapeutic Versatility
The therapeutic versatility of ASOs far exceeds that of small molecule drugs, encompassing multiple mechanisms of action that can be strategically selected based on therapeutic need.
Table 2: Mechanisms of Action of ASO Therapeutics
| Mechanism of Action | Functional Principle | Therapeutic Application |
|---|---|---|
| RNase H1-Mediated Degradation | ASO binds to target mRNA, recruiting RNase H1 enzyme which cleaves the RNA strand [11] [12] | Reduction of toxic gain-of-function proteins (e.g., Mipomersen for familial hypercholesterolemia) [103] [26] |
| Splice Modulation | ASO binds to pre-mRNA, masking splice regulatory elements to promote exon inclusion or exclusion [11] [12] | Correction of defective splicing (e.g., Nusinersen for spinal muscular atrophy; Eteplirsen for Duchenne muscular dystrophy) [12] [103] [26] |
| Steric Hindrance/Translation Block | ASO binds to target RNA, physically blocking ribosomal progression or protein binding [11] [101] | Inhibition of protein translation without RNA degradation [11] |
| MicroRNA Inhibition | ASO binds to microRNA, preventing its interaction with target mRNAs [26] | Restoration of natural gene regulation pathways (e.g., Miravirsen for hepatitis C) [26] |
This diversity of mechanisms enables ASOs to address disease pathology at its genetic origins, offering potential treatments for conditions where small molecules have repeatedly failed.
Key Experimental Protocols for ASO Research
Protocol 1: ASO-Mediated Gene Silencing via RNase H1 Mechanism
Objective: To achieve sequence-specific degradation of target mRNA using gapmer ASOs.
Principle: Gapmer ASOs contain a central DNA 'gap' region flanked by chemically modified RNA 'wings.' The DNA gap forms a heteroduplex with the target mRNA, recruiting RNase H1 which cleaves the mRNA strand [11] [12].
Workflow:
Materials and Reagents:
- Gapmer ASOs: Design with 8-10 deoxynucleotides in the gap region and 2'-MOE or LNA modifications in the wings [11] [103]
- Control ASOs: Include scrambled sequence and mismatch controls
- Delivery Vehicles: Lipofectamine 3000 for in vitro studies; GalNAc conjugates for hepatocyte targeting in vivo [8]
- Cell Culture Media: Appropriate medium supplemented with FBS and antibiotics
- qRT-PCR Reagents: Primers for target mRNA, reverse transcriptase, SYBR Green master mix
- Western Blot Materials: Antibodies against target protein and loading control
Procedure:
- ASO Design and Synthesis: Design gapmer ASOs targeting accessible regions of the mRNA (termini, internal loops, bulges). Incorporate phosphorothioate (PS) linkages in the backbone to enhance nuclease resistance and plasma protein binding [103].
- Cell Transfection: Seed cells in 24-well plates to reach 60-70% confluency at time of transfection. Complex ASOs with Lipofectamine 3000 in serum-free medium according to manufacturer's protocol. Apply complexes to cells for 6 hours, then replace with complete medium.
- RNA Isolation and qRT-PCR: Harvest cells 24-48 hours post-transfection using TRIzol reagent. Isolve total RNA and synthesize cDNA using reverse transcriptase. Perform qPCR with gene-specific primers to quantify target mRNA reduction relative to housekeeping genes.
- Protein Analysis: Lyse cells 48-72 hours post-transfection in RIPA buffer. Separate proteins by SDS-PAGE, transfer to PVDF membrane, and probe with specific antibodies. Quantify band intensity using densitometry software.
- Data Analysis: Normalize mRNA levels to housekeeping genes and protein levels to loading controls. Compare treatment groups using appropriate statistical tests (e.g., one-way ANOVA with post-hoc testing).
Protocol 2: Splice-Switching ASO Application
Objective: To modulate pre-mRNA splicing to restore protein function via exon skipping or inclusion.
Principle: Splice-switching ASOs (ssASOs) bind to specific regulatory sequences in pre-mRNA (splice sites, branch points, enhancers, or silencers), blocking access of the spliceosomal machinery to redirect splicing outcomes [12] [26].
Workflow:
Materials and Reagents:
- ssASOs: Fully modified oligonucleotides (e.g., PMO or 2'-MOE throughout) that do not support RNase H1 activity [103] [26]
- Cell Lines: Patient-derived fibroblasts or disease-relevant cell models
- RNA Stabilization Reagents: RNAlater or similar stabilization solution
- RT-PCR Materials: Gene-specific primers flanking the target exon, reverse transcriptase, PCR master mix
- Agarose Gel Electrophoresis: Gel apparatus, agarose, DNA staining dye, molecular weight markers
- Protein Function Assays: Reagents specific to the target protein's function (e.g., enzymatic assays, immunofluorescence)
Procedure:
- Target Identification: Analyze the splicing defect and identify key regulatory elements to target. For exon skipping, target splice enhancer sequences; for exon inclusion, target splice silencer or cryptic splice sites [12].
- ssASO Design and Validation: Design 18-30 nt ssASOs complementary to the identified regulatory elements. Use BLAST to ensure specificity. Synthesize with appropriate chemical modifications (e.g., PMO for exon skipping in DMD) [26].
- Cell Treatment and RNA Isolation: Transfert cells with ssASOs using appropriate methods. Isolate total RNA 24-48 hours post-transfection, ensuring RNA integrity (RIN >8.0).
- Splicing Analysis by RT-PCR: Perform reverse transcription followed by PCR with primers in exons flanking the region of interest. Separate PCR products by agarose gel electrophoresis and quantify band intensities.
- Sequence Validation: Purify alternative PCR products and confirm identity by Sanger sequencing.
- Functional Validation: Assess protein production and function using Western blot, immunofluorescence, or functional assays specific to the target protein.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for ASO Development
| Category | Specific Examples | Function & Application |
|---|---|---|
| ASO Chemistries | Phosphorothioate (PS) backbone [103] | Enhances nuclease resistance, improves pharmacokinetics, and facilitates protein binding for cellular uptake |
| 2'-O-methoxyethyl (2'-MOE) [103] | Increases binding affinity to RNA, enhances nuclease resistance, reduces immunostimulation | |
| Phosphorodiamidate Morpholino (PMO) [103] [26] | Neutral backbone used in splice-switching ASOs; resistant to nucleases, does not activate RNase H | |
| Locked Nucleic Acid (LNA) [26] | Extremely high binding affinity to RNA; used in microRNA inhibition | |
| Delivery Technologies | GalNAc conjugation [8] [100] | Targets asialoglycoprotein receptor on hepatocytes for liver-specific delivery |
| Lipid nanoparticles (LNPs) [8] | Protects ASOs from degradation, enhances cellular uptake, facilitates endosomal escape | |
| Cell-penetrating peptides [8] | Enhances cellular uptake of ASOs, particularly for non-hepatic tissues | |
| Analytical Tools | LC-MS/MS bioanalysis [8] | Quantifies ASO concentrations in biological matrices with high specificity |
| Stem-loop RT-qPCR [8] | Highly sensitive method for quantifying siRNA and microRNA therapeutics | |
| Immunohistochemistry | Determines tissue distribution and cellular localization of ASOs |
ASO technology represents a paradigm shift in therapeutic development, offering direct access to the approximately 80% of disease-causing proteins previously considered undruggable by small molecule approaches [100]. The rational design process, diverse mechanisms of action, and expanding repertoire of chemical modifications position ASOs as powerful tools for addressing genetically defined diseases at their molecular origins [11] [103].
The experimental protocols outlined herein provide a foundation for researchers to develop ASO-based therapies targeting previously inaccessible pathways. As delivery technologies continue to advance and our understanding of ASO pharmacology deepens, the application of ASOs is poised to expand across therapeutic areas, particularly for rare genetic disorders, neurological conditions, and oncology [12] [104]. With the small nucleic acid drug market projected to grow at 18.84% CAGR and reach USD 33.28 billion by 2034, the translational potential of ASO therapeutics continues to accelerate [104].
Application Note: Global ASO Market Dynamics and Key Therapeutic Areas
The antisense oligonucleotides (ASO) market is poised for significant expansion from 2025 to 2035, driven by robust pipeline development and increasing adoption for treating genetic, neurological, and oncological disorders. ASOs are short, single-stranded DNA or RNA molecules designed to bind specifically to target messenger RNA (mRNA), thereby modifying protein expression through various mechanisms [31]. This targeted approach represents a promising therapeutic strategy for impairing protein production and blocking the function of specific genes of interest in the human genome [31].
Table: Global ASO Market Size Projections, 2025-2035
| Year | Market Size (USD Billion) | CAGR (%) | Key Growth Drivers |
|---|---|---|---|
| 2025 | 2.5 [31] - 3.3 [105] | - | Existing approved therapies, strong pipeline |
| 2035 | Projected growth at CAGR of 6.3% [105] to 15% [31] | 6.3-15% | Product approvals, technological advancements, strategic collaborations |
The variation in market size estimates for 2025 stems from different methodological approaches in market analysis, though both sources indicate substantial growth potential through 2035. The higher projected CAGR of 15% [31] reflects anticipation of accelerated adoption and successful commercialization of late-stage pipeline candidates.
Pipeline Analysis and Clinical Trial Landscape
The ASO pipeline is characterized by substantial innovation and diversification across therapeutic areas. Current analysis indicates approximately 30 companies are actively engaged in developing ASO therapies, with over 170 candidate therapies in various development stages [31] [106]. These candidates are being evaluated both as monotherapies and in combination with other interventions, with the majority administered parenterally [31].
Clinical development activity is robust, with over 18,000 patients enrolled across clinical trials evaluating approximately 70 ASO-based therapy candidates [31] [106]. This substantial clinical investment underscores the growing confidence in ASO therapeutic platforms and provides a strong foundation for future market growth.
Table: ASO Pipeline Distribution by Therapeutic Area
| Therapeutic Area | Pipeline Representation | Key Late-Stage Candidates | Patient Enrollment Trends |
|---|---|---|---|
| Genetic Disorders | Dominant area [31] | Tofersen, Pelacarsen [31] | High enrollment in rare genetic diseases |
| Neurological Disorders | Major focus [31] [57] | - | Significant trial populations |
| Oncological Disorders | Substantial pipeline [31] | - | Growing clinical evaluation |
| Ocular Diseases | Established segment [105] | Pegaptanib [105] | Targeted patient populations |
The promising clinical profiles of ASOs are particularly valuable for rare monogenic diseases, which account for approximately 85% of all rare diseases [57]. The ability to design ASOs that specifically target disease-causing mutations once identified makes this platform especially suitable for addressing these conditions with high unmet medical needs.
Application Note: ASO Mechanism of Action and Therapeutic Applications
Molecular Mechanisms of Antisense Oligonucleotides
ASOs function through sophisticated molecular mechanisms that enable precise modulation of gene expression. These short, synthetic single or double-stranded nucleotide sequences are designed to complementarily bind to specific target mRNA molecules, preventing them from producing proteins [57]. The "antisense" designation derives from their binding to the "sense" portion of mRNA in a complementary manner, thereby interfering with protein production [57].
The therapeutic effect of ASOs is achieved through several mechanistic approaches:
- Steric Blockade: ASOs physically obstruct the ribosomal machinery from translating the mRNA into protein [61]
- RNase H Engagement: Some ASO designs recruit RNase H enzymes that degrade the target mRNA [61]
- Splice Modulation: Certain ASOs can alter pre-mRNA splicing patterns to exclude pathogenic exons or include compensatory ones [61]
This targeted approach addresses the molecular causes of disease rather than merely treating symptoms, representing a potentially transformative advancement in therapeutics [57].
Key Therapeutic Applications and Clinical Successes
ASOs have demonstrated particular utility in treating neurodegenerative diseases and rare genetic disorders. Notable successes include:
Neurological Applications: ASOs have shown significant promise in conditions including Duchenne muscular dystrophy, with four ASO therapies currently FDA-approved for this condition [57]. Clinical trials are also underway for ASOs targeting Parkinson's Disease and Motor Neuron Disease [57]. The ability of ASOs to target specific pathogenic mechanisms in the central nervous system represents a major advancement in neurology therapeutics.
Rare Disease Treatment: The predominance of monogenic etiology among rare diseases (approximately 85%) makes them particularly amenable to ASO interventions [57]. Currently, 13 ASOs targeting rare diseases have received regulatory approval from the FDA or European Medicines Agency (EMA) [57]. Research continues to expand the applications of ASOs for rare conditions, such as TUBB4A-related leukodystrophies including Hypomyelination of the Basal ganglia and Cerebellum (H-ABC) [57].
Ocular Diseases: The pegapatanib segment dominates the ocular disease application, holding approximately 35% of the ASO market revenue in 2025 [105]. This segment addresses conditions such as age-related macular degeneration by targeting vascular endothelial growth factor pathways to reduce abnormal blood vessel growth and fluid accumulation [105].
Diagram 1: ASO Mechanism of Action. ASOs bind complementarily to target mRNA, preventing translation of disease-causing proteins.
Protocol: ASO Research and Development Workflow
Target Identification and Validation Protocol
Objective: Systematically identify and validate molecular targets for ASO therapeutic development.
Procedure:
- Target Selection: Prioritize disease-associated genes with strong genetic validation (e.g., monogenic disorders) [57]
- Bioinformatic Analysis:
- Perform sequence alignment to identify conserved regions
- Assess secondary RNA structure using prediction algorithms
- Identify accessible binding sites using RNase H accessibility mapping
- In Silico Design: Utilize computational tools to design ASO sequences with optimal specificity and minimized off-target effects
- In Vitro Validation:
- Transfert candidate ASOs into relevant cell models
- Measure target mRNA reduction via qRT-PCR after 24-48 hours
- Assess protein level reduction via Western blot or immunofluorescence after 48-72 hours
- Evaluate cell viability and apoptosis to exclude cytotoxic effects
Quality Controls:
- Include mismatch controls (ASOs with 3-5 base mismatches) to demonstrate sequence specificity
- Utilize positive control ASOs targeting well-characterized genes
- Employ multiple cell lines or primary cells relevant to the disease pathology
ASO Optimization and Chemical Modification Protocol
Objective: Enhance ASO stability, binding affinity, and cellular uptake through strategic chemical modifications.
Procedure:
- Backbone Modifications:
- Incorporate phosphorothioate (PS) linkages to improve nuclease resistance and protein binding [61]
- Test varying degrees of PS modification (typically 40-60% of linkages)
- Sugar Modifications:
- Implement 2'-O-methoxyethyl (2'-MOE) modifications for increased binding affinity and nuclease resistance [31]
- Evaluate 2'-O-methyl modifications as alternatives
- Test constrained ethyl (cEt) or locked nucleic acid (LNA) modifications for highest affinity
- Terminal Modifications:
- Apply 5-methylcytosine modifications to reduce immunostimulatory potential
- Incorporate 3'-inverted deoxythymidine caps to prevent exonuclease degradation
- Delivery Optimization:
Analytical Assessments:
- Determine melting temperature (Tm) to quantify binding affinity
- Measure stability in serum and cellular extracts
- Assess protein binding properties using electrophoretic mobility shift assays
Table: ASO Generation Classification and Properties
| Generation | Key Modifications | Properties | Representative Therapeutics |
|---|---|---|---|
| First-Generation | Phosphorothioate backbone, some base modifications | Improved nuclease resistance, activated RNase H [31] | Early ASO developments |
| Second-Generation | 2'-O-alkyl modifications (2'-MOE, 2'-O-methyl) | Enhanced affinity, reduced toxicity, maintained RNase H activity [31] | Nusinersen (Spinraza) [107] |
| Third-Generation | Bridged nucleic acids (LNA, cEt), peptide conjugates | Highest binding affinity, improved pharmacokinetics [31] | Novel pipeline candidates |
Protocol: Preclinical Evaluation and Safety Assessment
In Vivo Efficacy Testing Protocol
Objective: Evaluate therapeutic efficacy and pharmacokinetics of lead ASO candidates in animal models.
Procedure:
- Animal Model Selection:
- Utilize genetically modified mice carrying human target sequences when possible
- Select disease-relevant models that recapitulate key pathological features
- Consider transgenic models expressing human target genes for species-specific ASOs
- Dose Administration:
- Pharmacodynamic Assessment:
- Measure target reduction in tissues at 1-4 weeks post-administration
- Evaluate functional endpoints relevant to disease pathology
- Assess duration of effect to inform dosing frequency
- Biomarker Monitoring:
- Quantify target engagement through direct measurement of mRNA reduction
- Monitor downstream protein levels and pathological biomarkers
- Evaluate physiological or behavioral improvements disease-specific metrics
Data Analysis:
- Compare treated versus control groups using appropriate statistical tests
- Establish correlation between target reduction and functional improvement
- Determine therapeutic index based on efficacy versus toxicity endpoints
Safety and Toxicology Assessment Protocol
Objective: Identify potential adverse effects and establish preliminary safety profile for clinical translation.
Procedure:
- In Vitro Safety Screening:
- Evaluate complement activation in human serum
- Assess pro-inflammatory cytokine release in peripheral blood mononuclear cells
- Test for off-target effects using transcriptomic analysis (RNA-seq)
- In Vivo Toxicology Studies:
- Conduct dose-range finding studies in rodent and non-rodent species
- Perform GLP-compliant studies with clinical formulation
- Monitor clinical signs, body weight, food consumption
- Assess clinical pathology (hematology, clinical chemistry, coagulation)
- Conduct histopathological examination of all major organs
- Organ-Specific Toxicity Evaluation:
- Liver: Monitor transaminases, bilirubin, and histopathology
- Kidney: Assess BUN, creatinine, and renal tubular function
- Coagulation: Evaluate platelet counts and coagulation parameters
- Immune System: Characterize immunostimulatory effects
Reporting:
- Identify no-observed-adverse-effect-level (NOAEL)
- Determine target organs of toxicity and reversibility
- Provide recommendations for safe starting dose in clinical trials
Application Note: Clinical Development Pathways and Commercialization
Clinical Trial Design Considerations
Designing clinical trials for ASO therapeutics requires special considerations based on target indication, patient population, and mechanism of action. Key elements include:
Patient Selection: For rare diseases, careful patient identification is crucial, often requiring genetic confirmation of the specific mutation being targeted [57]. The impact of ASOs is greater when administered early in the disease course before irreversible damage occurs [57].
Endpoint Selection:
- For neurological disorders: Composite endpoints incorporating motor function, survival, and patient-reported outcomes
- For rare diseases: Biomarker-based endpoints may be acceptable for accelerated approval
- For ophthalmological indications: Visual acuity, retinal imaging, and disease-specific scales
Dosing Regimen: Based on preclinical pharmacokinetic and pharmacodynamic data, determine initial dose, frequency, and route of administration (intrathecal, subcutaneous, intravenous, intravitreal) [31].
Regulatory and Commercialization Landscape
The regulatory environment for ASOs has evolved with mechanisms to support development of therapies for rare diseases. Orphan drug designations provide incentives including market exclusivity, tax credits, and fee waivers [108]. These advantages reduce development costs and attract investment to previously neglected areas [108].
Commercial success factors include:
- Pricing and Reimbursement: ASO therapies command premium pricing, with examples such as nusinersen costing over $2 million for a five-year treatment [57]
- Market Exclusivity: Orphan drug status provides 7 years of market exclusivity in the United States
- Manufacturing Scalability: Compared to other biologic medicines, commercial scale GMP production of oligonucleotides is relatively straightforward to scale up [107]
Diagram 2: ASO Clinical Development Pathway. The process from target identification through commercialization typically requires 10-15 years.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagent Solutions for ASO Development
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Phosphoramidite Reagents | Chemical building blocks for ASO synthesis | Include standard and modified nucleotides (2'-MOE, LNA, etc.) [61] |
| Lipid Nanoparticles (LNPs) | Delivery vehicles for in vitro and in vivo ASO delivery | Enhance cellular uptake and tissue targeting [61] |
| GalNAc Conjugation Chemistry | Ligand for hepatocyte-specific targeting | Enables subcutaneous administration with liver specificity [61] |
| RNase H Enzymes | Mechanism-specific validation | Confirm RNase H-dependent ASO activity [61] |
| Control ASOs | Experimental controls | Include scrambled sequence, mismatch, and target-specific controls |
| Cell Culture Models | In vitro screening | Disease-relevant cell lines and primary cells |
| Animal Disease Models | In vivo efficacy assessment | Genetically modified models when possible for human sequence targeting |
| qRT-PCR Assays | Target engagement quantification | Species-specific probes for discriminating human vs. animal targets |
| Western Blot Reagents | Protein-level effect confirmation | Antibodies against target protein and loading controls |
| Immunohistochemistry Kits | Tissue distribution assessment | Evaluate ASO distribution and target reduction in tissue sections |
The ASO market landscape from 2025 to 2035 presents substantial growth opportunities driven by technological advancements, expanding therapeutic applications, and supportive regulatory frameworks. Researchers and drug development professionals should focus on optimizing chemical modifications, delivery strategies, and clinical development pathways to fully realize the potential of this promising therapeutic modality. The continued elucidation of genetic mechanisms underlying diseases, combined with advances in ASO technology, positions this field as a cornerstone of precision medicine in the coming decade.
Conclusion
Antisense oligonucleotides represent a paradigm shift in therapeutic development, moving beyond symptomatic treatment to directly target the genetic root of diseases. This synthesis of the four intents confirms that while foundational science is well-established, innovation in chemical design, computational modeling, and delivery systems is rapidly overcoming historical challenges. The successful clinical application of ASOs, particularly for rare monogenic disorders, alongside their growing potential in common conditions like cardiovascular and neurodegenerative diseases, underscores their transformative impact. Future directions will be shaped by advances in personalized screening platforms, such as patient-derived organoids, reducing the time and cost of drug development. Furthermore, the anticipated market growth, projected to reach USD 2.5 billion in 2025 with a 15% CAGR, signals strong confidence and investment in this modality. For researchers and drug developers, the continued convergence of ASO technology with precision medicine promises an expanding frontier for treating previously intractable diseases, ultimately enabling a new era of highly specific, genetically informed therapeutics.
References
- 1. Structure, design, and synthesis of antisense ... [https://www.bocsci.com/resources/structure-design-and-synthesis-of-antisense-oligonucleotides.html?srsltid=AfmBOopRX25znnQjk2SG0V8ZVCHjkw7FvU-Myla5hjhTnMdlidWnsIjr]
- 2. Gene expression silencing therapy in tumors, focus on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1657040/full]
- 3. Application of Antisense Oligonucleotides as an Alternative ... [https://www.mdpi.com/1422-0067/26/21/10524]
- 4. Antisense oligonucleotide therapies for monogenic disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268252/]
- 5. What are RNA therapeutics? mRNA, siRNA, and ASOs ... [https://www.drugdiscoverynews.com/what-are-rna-therapeutics-mrna-sirna-and-asos-explained-16777]
- 6. Lesson 19 – How siRNAs and ASOs Differ [https://www.nlorem.org/lesson-19-how-sirnas-and-asos-differ/]
- 7. Structure-based design of antisense oligonucleotides that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8404888/]
- 8. Translational and clinical development of therapeutic siRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477600/]
- 9. Chemically inducible antisense oligonucleotides for cell- ... [https://pubs.rsc.org/en/content/articlelanding/2025/cb/d5cb00186b]
- 10. Mechanisms of Action of the US Food and Drug Administration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11695194/]
- 11. Landscape of small nucleic acid therapeutics [https://www.nature.com/articles/s41392-024-02112-8]
- 12. Possibilities and limitations of antisense oligonucleotide ... [https://www.nature.com/articles/s43856-023-00419-1]
- 13. What Does RNase H Do & Its Role in ASOs [https://lifesciences.danaher.com/us/en/library/rnase-h.html]
- 14. Nonsense-mediated decay as a terminating mechanism for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4027159/]
- 15. Use of steric blocking antisense oligonucleotides for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11030329/]
- 16. Evolution and Breakthroughs in Exon Skipping and Splice ... [https://pubmed.ncbi.nlm.nih.gov/40720009/]
- 17. Genome-wide functional annotation and interpretation of ... [https://www.nature.com/articles/s10038-025-01424-z]
- 18. Development and future prospects of exon-skipping ... [https://www.sciencedirect.com/science/article/pii/S0387760425001391]
- 19. Development and future prospects of exon-skipping ... [https://pubmed.ncbi.nlm.nih.gov/41033146/]
- 20. Sarepta Announces Completion of ESSENCE Trial for ... [https://www.parentprojectmd.org/sarepta-announces-completion-of-essence-trial-for-exon-45-53-skipping-therapies/]
- 21. Application of Antisense Oligonucleotides as an Alternative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610768/]
- 22. Targeting RNA splicing modulation: new perspectives for ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03279-w]
- 23. Gene silencing by siRNAs and antisense oligonucleotides in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3916955/]
- 24. A Half-Century History of Applications of Antisense ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6099785/]
- 25. Antisense therapy [https://en.wikipedia.org/wiki/Antisense_therapy]
- 26. ASOs: A Short History on the Diversity of Clinical Applications [https://www.criver.com/eureka/asos-a-short-history-on-the-diversity-of-clinical-applications]
- 27. Antisense Oligonucleotides (ASOs) for Gene Silencing | IDT [https://www.idtdna.com/pages/products/functional-genomics/antisense-oligos]
- 28. Antisense Oligonucleotide Therapeutics Pipeline Market [https://www.globenewswire.com/news-release/2025/08/08/3130029/28124/en/Antisense-Oligonucleotide-Therapeutics-Pipeline-Market-Landscape-Report-2025-Explore-Clinical-and-Nonclinical-Stages-Therapeutic-Assessments-and-the-Future-of-ASO-Therapies.html]
- 29. Tailored antisense oligonucleotides for ultrarare CNS ... [https://www.sciencedirect.com/science/article/pii/S2162253125001696]
- 30. Guidelines for Experiments Using Antisense Oligonucleotides ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6555184/]
- 31. Antisense Oligonucleotides Market Trends Report 2025-2035 [https://finance.yahoo.com/news/antisense-oligonucleotides-market-trends-report-080700834.html]
- 32. Nano-rare Patient Colloquium / 2025 – Recap [https://www.nlorem.org/nano-rare-patient-colloquium-2025/]
- 33. The chemical evolution of oligonucleotide therapies of clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5517098/]
- 34. Antisense oligonucleotide based therapeutics and its ... [https://www.sciencedirect.com/science/article/pii/S2590098623000167]
- 35. Know your oligo mod: 2ʹ-MOE - The BiosearchTech Blog [https://blog.biosearchtech.com/know-your-oligo-mod-2%CA%B9-moe]
- 36. Efficacy, biodistribution and safety comparison of chemically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11417397/]
- 37. Favorable efficacy and reduced acute neurotoxicity by ... [https://www.sciencedirect.com/science/article/pii/S2162253124000489;]
- 38. Nano Approaches to Nucleic Acid Delivery: Barriers, Solutions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11994986/]
- 39. RNA Therapeutics: Delivery Problems and Solutions—A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567017/]
- 40. Non-cationic carriers for siRNA delivery [https://www.sciencedirect.com/science/article/abs/pii/S0168365925009769]
- 41. a comparative study of aptamer, vitamin E, and cholesterol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599544/]
- 42. Recent advances in using liposomes for delivery of nucleic ... [https://www.sciencedirect.com/science/article/pii/S2352952023000117]
- 43. Advances in the pharmaceutical development of antibody ... [https://www.sciencedirect.com/science/article/pii/S0928098725002908]
- 44. computational design of antisense oligonucleotides ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1548269/full]
- 45. In Silico Prediction and Selection of Exon-Skipping ... [https://pubmed.ncbi.nlm.nih.gov/40720013/]
- 46. The Science of ASO Design and Screening Using the FDA ... [https://www.linkedin.com/pulse/science-aso-design-screening-using-fda-guidance-nano-rare-crooke-yp18c]
- 47. Antisense Oligonucleotide in vitro screening assays: 5 key ... [https://www.ncardia.com/insights/resources/how-to-design-relevant-aso-invitro-screening]
- 48. The powerful world of antisense oligonucleotides: From bench ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9285911/]
- 49. Experimental Drug May Benefit Some Patients with Rare ... [https://www.cuimc.columbia.edu/news/experimental-drug-may-benefit-some-patients-rare-form-als]
- 50. Experimental Gene-Silencing Therapy May Benefit ... [https://www.nyp.org/advances/article/neurology-neurosurgery/experimental-gene-silencing-therapy-may-benefit-patients-with-rare-form-of-als]
- 51. Small Nucleic Acid Drugs Expected to Be Approved by 2025 [https://www.biochempeg.com/article/420.html]
- 52. Have antisense oligonucleotides hit their stride? - C&EN [https://cen.acs.org/business/antisense-oligonucleotides-hit-stride/96/i45]
- 53. Application of Antisense Oligonucleotides as an Alternative ... [https://pubmed.ncbi.nlm.nih.gov/41226561/]
- 54. Antisense Oligonucleotides: An Emerging Area in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7355792/]
- 55. Gene expression silencing therapy in tumors, focus on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531239/]
- 56. Discovery in RNA therapy for mutated cancer gene [https://www.eurekalert.org/news-releases/1106227]
- 57. A rare opportunity for ASOs - Drug Discovery World (DDW) [https://www.ddw-online.com/a-rare-opportunity-for-asos-34429-202504/]
- 58. Gene silencing: a step forward for rare disease therapy [https://www.drugtargetreview.com/article/157722/gene-silencing-a-step-forward-for-rare-disease-therapy/]
- 59. Oligonucleotide-based therapeutics for neurodegenerative ... disorders [https://pubmed.ncbi.nlm.nih.gov/40118328/]
- 60. Avoiding late-onset neurotoxicity induced by ASOs [https://www.bioxconomy.com/modalities/unleashing-asos-on-neurological-disease-by-solving-late-onset-neurotoxicity]
- 61. Advances in RNA-based therapeutics: current breakthroughs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592931/]
- 62. ASO Therapy Statistics 2025: Data on Rare Disease Treatment [https://www.nome.bio/blog/custom-aso-therapy-statistics]
- 63. The N=1 Collaborative: advancing customized nucleic acid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022754/]
- 64. Hope for Patients with Ultra-Rare Genetic Diseases - QPS [https://www.qps.com/2024/03/18/customized-therapies-offer-hope-for-patients-with-ultra-rare-genetic-diseases/]
- 65. Therapeutic potential of circular antisense oligonucleotides ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025075270]
- 66. Oligonucleotide Therapeutics: Mechanisms & Delivery [https://www.bocsci.com/blog/oligonucleotide-based-therapeutics-mechanisms-challenges-and-opportunities-in-drug-delivery/?srsltid=AfmBOorVHoLoAe737n23JIkHjX-cQ97B7bsXTW1wZEGJU5korKZmGH8B]
- 67. Off-target effects of oligonucleotides and approaches ... [https://www.sciencedirect.com/science/article/pii/S2472555225000474]
- 68. Dynamic and static control of the off-target interactions ... [https://www.nature.com/articles/s41467-023-43714-0]
- 69. Insights into innate immune activation via PS-ASO–protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371907/]
- 70. Antisense Oligonucleotide Therapies for Movement Disorders [https://practicalneurology.com/diseases-diagnoses/movement-disorders/antisense-oligonucleotide-therapies/31573/]
- 71. Lesson 13 – PS ASOs and Innate Immunity [https://www.nlorem.org/lesson-13-ps-asos-and-innate-immunity/]
- 72. Evaluation of off‐target effects of gapmer antisense ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6915909/]
- 73. New approach methodologies to assess wanted and ... [https://www.sciencedirect.com/science/article/pii/S2666027X25000088]
- 74. Challenges of ASO development [https://labtesting.wuxiapptec.com/2025/04/10/5-tips-to-navigating-antisense-oligonucleotide-drug-development/]
- 75. Antisense oligonucleotides: Navigating ethical and safety ... [https://www.ddw-online.com/antisense-oligonucleotides-navigating-ethical-and-safety-challenges-33473-202502/]
- 76. Unraveling and controlling late-onset neurotoxicity of ... [https://www.sciencedirect.com/science/article/pii/S216225312500246X]
- 77. Advances in RNA-based therapeutics: current ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1675209/full]
- 78. Antisense Oligonucleotides - Optimization of ASOs and ... [https://www.linkedin.com/pulse/optimization-asos-delivery-systems-luke-mclaughlin-uls9f]
- 79. Antisense Oligonucleotides Market Size and Forecast – 2025 [https://www.coherentmarketinsights.com/market-insight/antisense-oligonucleotides-market-1879]
- 80. Antisense Oligonucleotide Therapeutics Clinical Trial [https://www.globenewswire.com/news-release/2025/08/28/3141021/0/en/Antisense-Oligonucleotide-Therapeutics-Clinical-Trial-Pipeline-Appears-Robust-With-70-Key-Pharma-Companies-Actively-Working-in-the-Domain-DelveInsight.html]
- 81. Antisense Oligonucleotide Therapeutics Market Current ... [https://www.insightaceanalytic.com/report/global-antisense-oligonucleotide-therapeutics-market/1245]
- 82. The Oligonucleotide Market in 2025 and Beyond, Key ... [https://www.linkedin.com/pulse/oligonucleotide-market-2025-beyond-key-trends-luke-mclaughlin-sghuf]
- 83. Oligonucleotides Market Size and Forecast 2025 to 2034 [https://www.precedenceresearch.com/oligonucleotides-market]
- 84. Accelerating ALS Clinical Trial Recruitment in the U.S [https://mytomorrows.com/blog/biopharma/accelerating-als-clinical-trial-recruitment-in-the-us/]
- 85. Integrating N-of-1 Trials Into Learning Health Care Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068953/]
- 86. 2025 access trends [https://www.bioxconomy.com/access-and-channel/2025-access-trends]
- 87. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 88. Organoid models in oncology: advancing precision cancer ... [https://www.cancerbiomed.org/content/early/2025/07/24/j.issn.2095-3941.2025.0127]
- 89. Beyond animal models: how organoids could transform ... [https://www.nature.com/articles/d42473-025-00219-2]
- 90. iPSC-derived and Patient-Derived Organoids: Applications ... [https://www.sciencedirect.com/science/article/pii/S2666027X24000501]
- 91. The Use of Antisense Oligonucleotides for Gene Silencing [https://huntingtonstudygroup.org/hd-insights/the-use-of-antisense-oligonucleotides-for-gene-silencing/]
- 92. Antisense oligonucleotides: a novel Frontier in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10690781/]
- 93. Healthcare Providers' Understanding of Data Displays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10589436/]
- 94. Constructing a finer-grained representation of clinical trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10771511/]
- 95. ASOs vs siRNA – Which is Right for Me? [https://www.origene.com/blog/asos-vs-sirna]
- 96. What is the difference between therapeutic siRNA and ... [https://synapse.patsnap.com/article/what-is-the-difference-between-therapeutic-sirna-and-antisense-oligonucleotides]
- 97. Small Nucleic Acid Drugs: siRNA vs ASO [https://www.bocsci.com/blog/sirna-vs-aso-small-nucleic-acid-drugs-revolution-unleashed/?srsltid=AfmBOorkcuJBW_y8pVV-5eepZUG9igrGUa80V62mEKsaJxx4PjiznqtF]
- 98. Comparison of antisense oligonucleotides and siRNAs in ... [https://www.sciencedirect.com/science/article/pii/S0006291X02020132]
- 99. Advances in RNA therapeutics: Classes, innovations and ... [https://www.sciencedirect.com/science/article/pii/S3050632825000162]
- 100. Top 3 Opportunities Shaping Oligonucleotide Therapeutics [https://labtesting.wuxiapptec.com/2025/07/10/3-therapeutic-considerations-for-the-future-of-oligonucleotide-development/]
- 101. How do ASOs drug differ from other small nucleic acid drugs? [https://synbio-tech.com/difference-between-asos-drug-and-small-nucleic-drugs]
- 102. Current status and trends in small nucleic acid drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11413693/]
- 103. Drug Discovery Perspectives of Antisense Oligonucleotides [https://pmc.ncbi.nlm.nih.gov/articles/PMC10129852/]
- 104. Small Nucleic Acid Drug Market 2025 Clinical Trials Rise [https://www.towardshealthcare.com/insights/small-nucleic-acid-drug-market-sizing]
- 105. Antisense Oligonucleotides Market [https://www.futuremarketinsights.com/reports/antisense-oligonucleotides-market]
- 106. Antisense Oligonucleotides Market Trends Report 2025- ... [https://www.globenewswire.com/news-release/2025/10/01/3159255/28124/en/Antisense-Oligonucleotides-Market-Trends-Report-2025-2035-170-Pipeline-Candidates-30-Players-and-18-000-Patients-Drive-Growth-in-Genetic-Neurological-and-Oncological-Disorders.html]
- 107. Antisense Oligonucleotides Market Size & Share, Forecast [https://www.transparencymarketresearch.com/antisense-oligonucleotides-market-report.html]
- 108. Novel Drugs Market Forecast 2035 | Key Driver, Restraint, [https://www.openpr.com/news/4273905/novel-drugs-market-forecast-2035-key-driver-restraint]